February 28, 2021
https://doi.org/10.23999/j.dtomp.2021.2.1
J Diagn Treat Oral Maxillofac Pathol 2021;5:15–9.
Under a Creative Commons license
HOW TO CITE THIS ARTICLE
Fesenko II, Snisarevskyi PP, Zaritska VI. Infected punctum–associated cyst mimicking erysipelas. J Diagn Treat Oral Maxillofac Pathol 2021;5(2):15–9.
INSTITUTIONAL REPOSITORY
https://ir.kmu.edu.ua/handle/123456789/645
Summary
Epidermoid cysts (congenital and acquired) are not the unusual benign lesions. But to our knowledge, this is the first report in the English literature that describes an uncommon presentation of the infected acquired epidermoid cyst (ie, punctum–associated cyst or atheroma) manifesting as unilateral facial erysipelas in a 74-yearold Caucasian female. Terminology and the “submarine sign” ultrasound appearance are also analyzed.
INTRODUCTION
Punctum–associated cyst (PAC) is termed in the literature as epidermoid cyst1,2, epidermal cyst3 , keratinous cyst4 , sebaceous cyst4 , retention cyst of the sebaceous gland5 , and atheroma5 . The authors are united in their opinions that cutaneous punctum is a hallmark of the clinical diagnosis for the acquired keratin-filled cutaneous-linked cysts (ie, acquired epidermoid cyst).1–5 They describe punctum as 1) a place of plugging of the follicular orifice1 and 2) a place where the skin is fused with the cyst membrane (in this place, a cutaneous retraction point can be found).5
Hoang et al notes that such benign lesions may become inflamed as a result of the rupture of the cyst wall (ie, cyst lining).1 Usually, with suppuration of PAC, the skin above it has a round-shape hyperemia, edematous, does not fold into a fold, the formation is painful and badly movable.5 Even fluctuation can be determined (due to the appearance of pus).5
The differential diagnosis of PAC can be performed with furuncle6 , cutaneous abovethe-skin-level manifestations (subcutaneous granuloma) of odontogenic cutaneous sinus tract7 , non-odontogenic subcutaneous granuloma5 , and pyogenic granuloma8.
This study presents a uniquely rare case of infected PAC of the infraorbital area mimicking unilateral erysipelas in a 74-year-old female.
CASE
A 74-year-old Caucasian female presented to the center of maxillofacial surgery in July 2015 with a local facial pain and a skin erythema in the right infraorbital area which began 4 days ago.
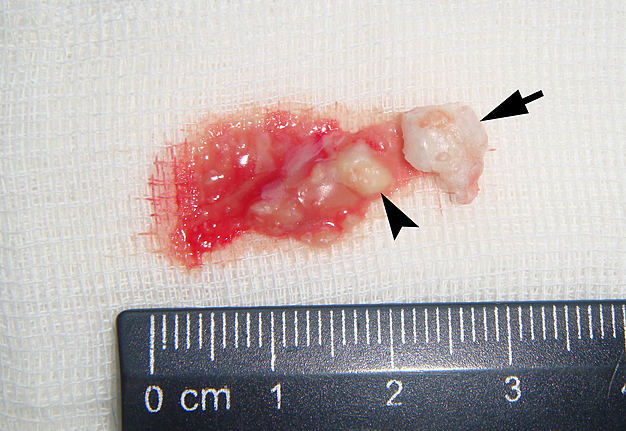
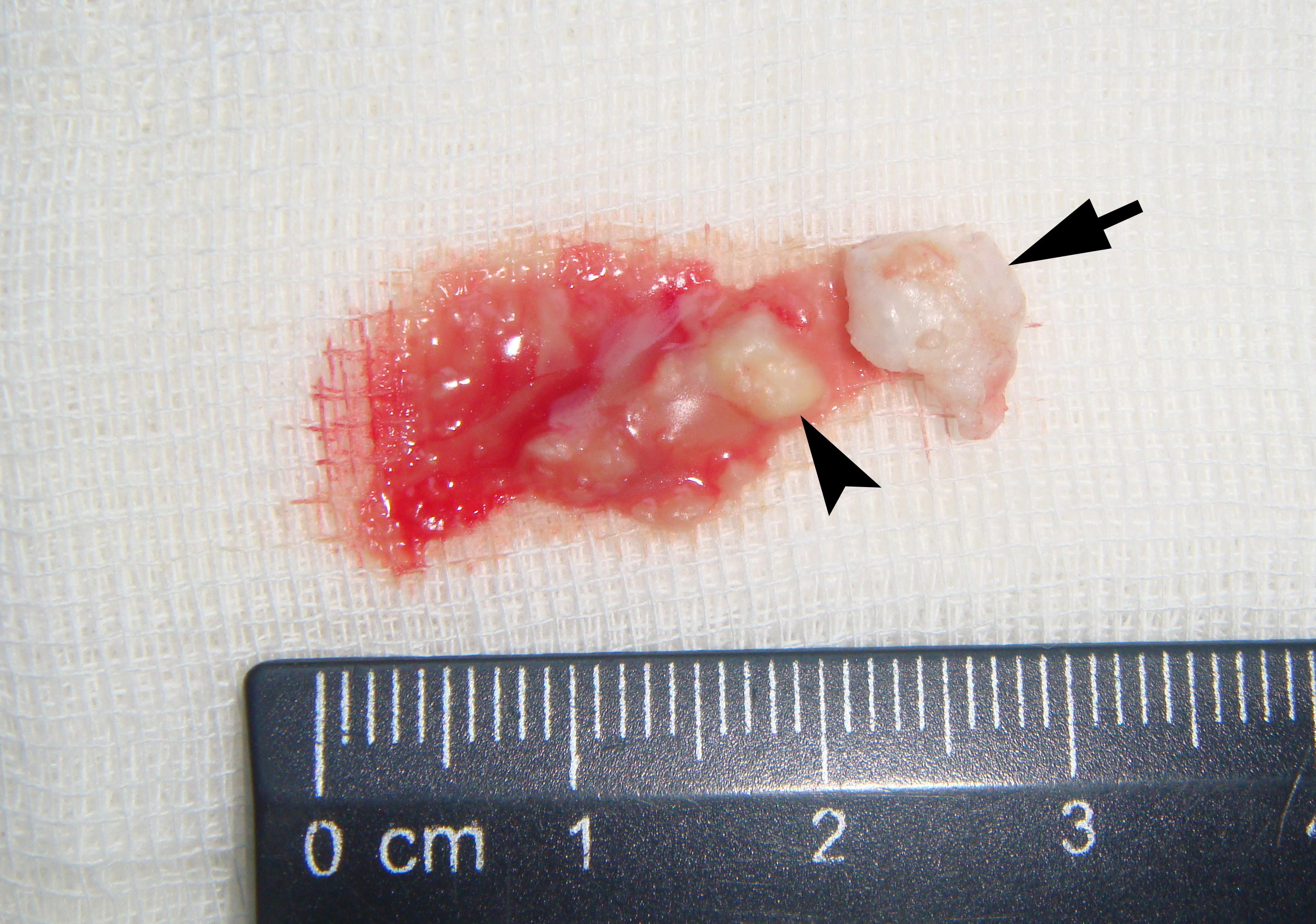
Examination revealed an erythematous area (severe redness) of the right face extending vertically from the projection of the infraorbital rim to the angle of the mouth and horizontally from the right zygomatic area to the right nasal ala. Also, a separate erythematous area (moderate redness) at the dorsum of the nose with a wound on the skin was visualized what mimicked the facial emphysema. But, the presence of a punctum (Fig 1) on the skin surface (in the middle of erythema) at the right infraorbital area with a white 1.5-mm circle around gave a reason to suspect an infected punctum–associated cyst with atypical manifestation.
Under the local anesthesia (right extraoral infraorbital nerve block using 0.7 ml Ultracain D-S forte, Frankfurt, Aventis Pharma Deutschland GmbH, Germany) a small diameter elliptical incision was performed with the inclusion of the punctum1 . A suppurated malodorous cheese-like content was obtained and the fragment of a thick white cystic wall (what is typical for the PACs) was removed during the curettage (Fig 2).
Microscopic histopathologic examination confirmed the diagnosis atheroma (common term in some East European countries) (ie, acquired type of epidermoid cysts) showing a stratified squamous epithelium with perifocal inflammation. Postoperative period was smooth with no pain and gradual (during several days) decrease of skin erythema.
DISCUSSION
Epidermoid cyst can be congenital and acquired.1 To the acquired ones belong punctum–associated cysts (ie, atheromas) which can be suspected by collecting anamnesis and performing clinical and ultrasound examination.1–3,5 Moreover, Lee et al introduced a “submarine sign” term as a special ultrasonographic feature of the epidermoid cysts.9 Such term was applied because a keratin-plugged orifice of the PAC was visualized on sonograms as a submarine periscope.
Nowadays, the literature indicate that the term sebaceous cyst is considered misnomer due to the fact of absence of sebaceous glands within the cyst lining.
A small elliptical incision with partial skin removal and cystectomy is recommended if a punctum or scar is present.5 Also, the malignant degeneration of the epidermoid cysts is described what required a wide excision of the tumor (with a small possibility of radiation therapy after surgery) or radiation therapy as a primary treatment.10 Multiple works reported carcinomas arising from epidermoid/sebaceous cysts (patients` age varied from 21 to 89 yrs) what required from surgeons to motivate patients to remove the cysts as soon as possible.10–15
Veenstra et al summarized global literature presenting the data that squamous cell carcinoma arising from epidermal cysts has an incidence ranging from 0.011 to 0.045 percent.14
According to Ochs and Dolwick erysipelas distinguished from other soft tissue infection (cellulitis) primarily by its well-defined and raised margins.16 In our case the presence of only one part of a cystic wall explains why the erythematous skin area was so large and had no well-defined round-shape borders. Analysis of the English literature sources show no evidence of previously published cases of acquired infected epidermoid cysts mimicking erysipelas.
CONCLUSIONS
In sum, the proposed term punctum–associated cysts can be applied to the acquired epidermoid cysts which show the presence of plugged orifice, which have “submarine sign” ultrasonographic appearance and which were previously termed sebaceous cysts (also known as atheroma and retention cysts of the sebaceous glands). Such punctum can be very useful in differential diagnostics between infect cyst and unilateral facial erysipelas.
REFERENCES (16)
- Hoang VT, Trinh CT, Nguyen CH, Chansomphou V, Chansomphou V, Tran TTT. Overview of epidermoid cyst. Eur J Radiol Open 2019;6:291–301. https://doi.org/10.1016/j.ejro.2019.08.003
- Wollina U, Langner D, Tchernev G, França K, Lotti T. Epidermoid cysts - a wide spectrum of clinical presentation and successful treatment by surgery: a retrospective 10-year analysis and literature review. Open Access Maced J Med Sci 2018;6(1):28–30. https://doi.org/10.3889/oamjms.2018.027
- Takemura N, Fujii N, Tanaka T. Epidermal cysts: the best surgical method can be determined by ultrasonographic imaging. Clin Exp Dermatol 2007;32(4):445–7. https://doi.org/10.1111/j.1365-2230.2007.02408.x 4
- Sabhlok S, Kalele K, Phirange A, Kheur S. Congenital giant keratinous cyst mimicking lipoma: сase report and review. Indian J Dermatol 2015;60(6):637. https://doi.org/10.4103/0019-5154.169160
- Tymofieiev OO. Maxillofacial surgery and surgical dentistry [Russian]. Kyiv, Ukraine: Medicine; 2020.
- Lin HS, Lin PT, Tsai YS, Wang SH, Chi CC. Interventions for bacterial folliculitis and boils (furuncles and carbuncles). Cochrane Database Syst Rev 2018;2018(8):CD013099. https://doi. org/10.1002/14651858.CD013099 7
- Cherniak OS, Zaritska VI, Snisarevskyi PP, Fesenko II, Blinova VP, Koba NM, Pavlenko RA, Holodenko VM. Single and multiple odontogenic cutaneous sinus tracts. J Diagn Treat Oral Maxillofac Pathol 2020;4(11):197–216. https://doi.org/10.23999/j.dtomp.2020.11.2 8
- Wollina U, Langner D, França K, Gianfaldoni S, Lotti T, Tchernev G. Pyogenic granuloma – a common benign vascular tumor with variable. Open Access Maced J Med Sci 2017;5(4):423–6. https://doi.org/10.3889/oamjms.2017.111
- Lee DH, Yoon CS, Lim BJ, Lee HS, Kim S, Choi AL, Kim S. Ultrasound feature-based diagnostic model focusing on the “submarine sign” for epidermal cysts among superficial soft tissue lesions. Korean J Radiol 2019;20(10):1409–21. https://doi.org/10.3348/kjr.2019.0241
- Faltaous AA, Leigh EC, Ray P, Wolbert TT. A rare transformation of epidermoid cyst into squamous cell carcinoma: a case report with literature review. Am J Case Rep 2019;20:1141–3. https://doi.org/10.12659/AJCR.912828
- López-Ríos F, Rodríguez-Peralto JL, Castaño E, Benito A. Squamous cell carcinoma arising in a cutaneous epidermal cyst. Am J Dermatopathol 1999;21(2):174–7. https://doi.org/10.1097/00000372-199904000-00012
- Bauer BS, Lewis VL. Carcinoma arising in sebaceous and epidermoid cysts. Ann Plast Surg 1980;5(3):222–45. https://doi.org/10.1097/00000637-198009000-00008
- Yaffe HS. Squamous cell carcinoma arising in an epidermal cyst. Arch Dermatol 1982;118(12):961.
- Veenstra JJ, Choudhry S, Krajenta RJ, Eide MJ. Squamous cell carcinoma originating from cutaneous cysts: The Henry Ford Experience and review of the literature. J Dermatolog Treat 2016;27(1):95–8. https://doi.org/10.3109/09546634.2015.1054779
- Morgan MB, Stevens GL, Somach S, Tannenbaum M. Carcinoma arising in epidermoid cyst: a case series and aetiological investigation of human papillomavirus. Br J Dermatol 2001;145(3):505–6. https://doi.org/10.1046/j.1365-2133.2001.04400.x
- Ochs MW, Dolwick MF. Facial erysipelas: report of a case and review of the literature. J Oral Maxillofac Surg 1991;49(10):1116–20. https://doi.org/10.1016/0278-2391(91)90148-f