Obstructive Submandibular Sialadenitis Complicated with Severe Neck Phlegmon: Transcutaneous Removal of Sialolith with a Flow of Pus: Literature Review of Extraoral Complications
November 30, 2021
https://doi.org/10.23999/j.dtomp.2021.11.1
J Diagn Treat Oral Maxillofac Pathol 2021;125–134.
Under a Creative Commons license
HOW TO CITE THIS ARTICLE
Savchuk LA, Fesenko II. Obstructive submandibular sialadenitis complicated with severe neck phlegmon: transcutaneous removal of sialolith with a flow of pus: literature review of extraoral complications. J Diagn Treat Oral Maxillofac Pathol 2021;5(11):125–34.
INSTITUTIONAL REPOSITORY
https://ir.kmu.edu.ua/handle/123456789/623
SUMMARY
Sialolithiasis, as the most common reason (60–85 percent) of obstructive salivary gland disease, in the rare cases, may be complicated by soft tissues abscess or/and fistula. The purpose of this report is to present a rare case of submandibular gland sialolithiasis complicated with severe neck phlegmon in a 47-year-old Caucasian male. Ultrasonography and transcutaneous removal of sialolith upon the purulent locus lancing are highlighted. Our literature review based on the existed ones with a total 24 complication cases is presented. Wakoh et al`s classification of submandibular gland sialolith-associated fistulas types is analyzed. The ultrasound imaging is still underestimated and not adequately popularized among head and neck and oral and maxillofacial surgeons. Presented case and published reports show the usefulness of this constantly developing diagnostic technique in a combination with knowledge of possible extraoral purulent complications’ and its management.
INTRODUCTION
Sialolithiasis, as the most common reason (60–85 percent)1 of obstructive salivary gland disease, in the rare cases, may be complicated by soft tissues abscess2,3 or/and fistula.4,5 A clinical study by Kishore Kumar et al (2012) of the 200 cases of cutaneous sinuses revealed that only in 0.5 percent of cases was noted cutaneous fistula as a result of submandibular gland calculus.6 Such fistula usually is named by authors as orocutaneous or sialo-cutaneous fistula.5,7
According to our literature search, submandibular gland calculus-associated abscesses/phlegmons are even rarer comparing with sialo-cutaneous fistulae. Purulent floor of the mouth processes as a complication of obstructive salivary stone usually were diagnosed by multi-slice computed tomography (MSCT).3,8 Despite ultrasound (US) are widely described as a diagnostic tool for submandibular sialolithiasis1,9,10 its application in case of calculus-associated cervical fistulae and abscess/phlegmon to our knowledge is presented in very limited publications.11,12
The purpose of this report is to present a rare case of submandibular gland sialolithiasis complicated with severe neck phlegmon in a 47-year-old male. Ultrasound and transcutaneous removal of sialolith upon the purulent locus lancing are highlighted. Our own literature review based on the existed ones with a total 24 complication cases is presented.
CASE
A 47-year-old Caucasian gentleman was referred to the Kyiv Regional Clinical Hospital with a left neck and submandibular swelling (Fig 1), fever, difficulty of swallowing. The complaints had been initiated with salivary colics several weeks before. Previously, during the last years, patient noted a painful chewing–associated submandibular swelling at the left side.
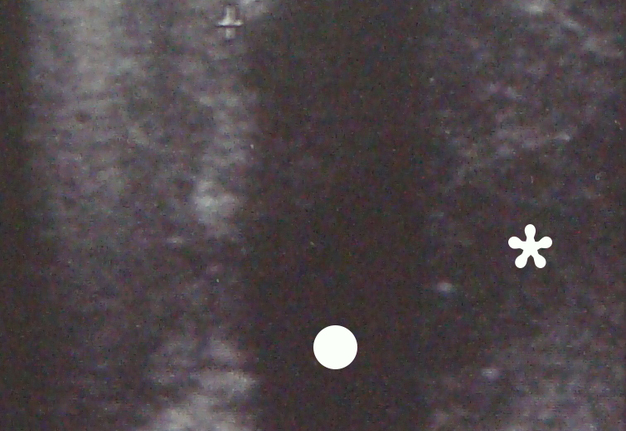
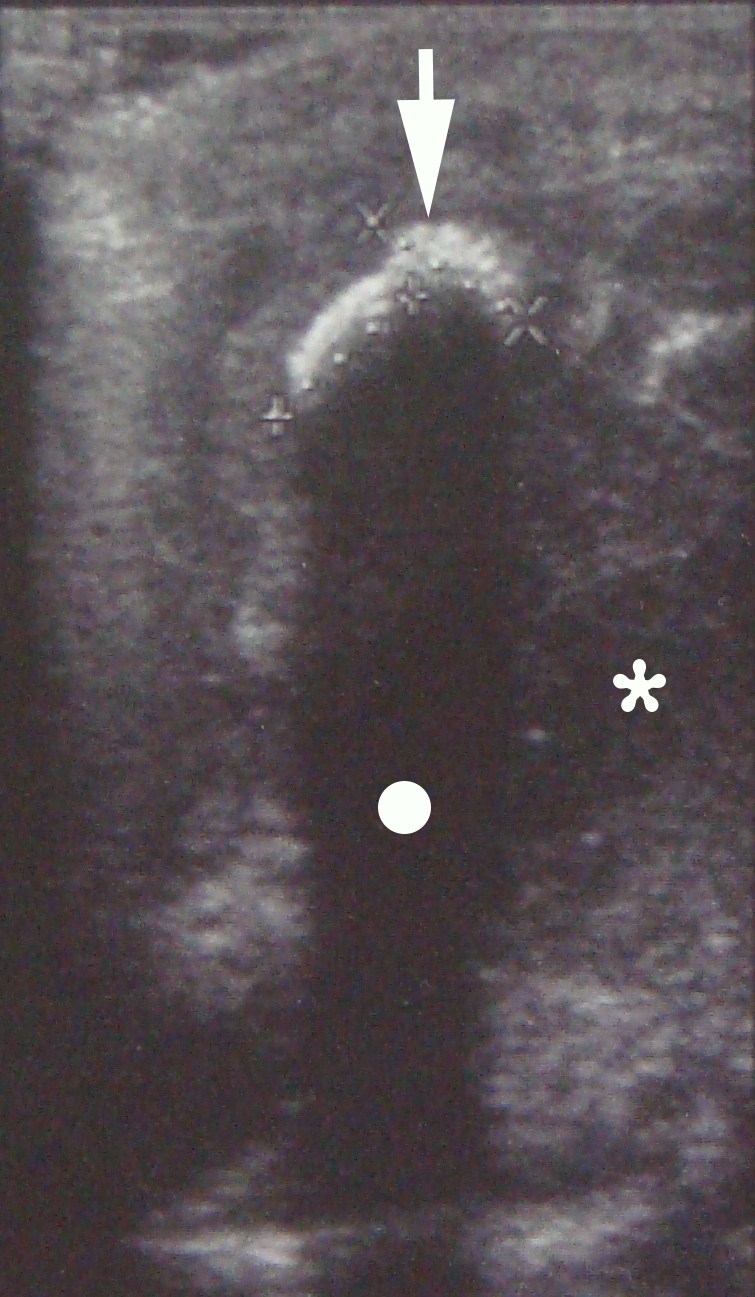
US was performed by an experienced doctor of ultrasound diagnostics (L.A.S., her experience – 31 years). Submandibular and neck regions were examined bilaterally according to the protocol (ie, swelled and healthy side). Using linear transducer (12-5 MHz) in a longitudinal submandibular position, the gray scale US (also known as B-mode [brightness mode]) showed hyperechoic semilunar structure (ie, sialolith, measured 0.76 × 0.78 cm) with an artifact of acoustic shadowing behind (Fig 2). Also, in this left submandibular region, the submandibular gland with a hypoechoic parenchyma and the collection of hypoechoic heterogenic content (ie, pus) were visualized. The diagnosis of obstructive sialadenitis caused by sialolith and complicated with submandibular and left neck phlegmon was established.
The phlegmon lancing was done under the local infiltration anesthesia using 8.0 ml of 4 percent Ultracain® D-S solution (Sanofi-Aventis Deutschland GmbH, Frankfurt am Main, Germany) mixed with 12.0 ml of 0.9% saline solution in a 20-ml syringe. Intravenous sedation was done by anesthesiologist`s team. An oblique 3.5-cm incision was planned and done inside the prominent upper neck skin crease (Fig 1C). A 1.2-cm salivary calculus (ie, sialolith) was removed with a flow of pus (~22 ml) upon the finger examination (ie, revision) of the purulent wound (Fig 3). Tubular double drainage was installed after rinsing with an antiseptic solution. Post-operative period associated with infusion and antibacterial therapy and wound rinsing showed gradual decrease of soft tissues inflammatory changes and complaints.
DISCUSSION
Digestion-associated swelling9 (also known as “mealtime syndrome”13) in the submandibular region is a common disorder at the in- and out-patient oral and maxillofacial units. And typically, this is a manifestation of obstructive sialadenitis caused by sialoliths. Such complications of obstructive sialoliths as pus collection in the cellular spaces and fistulae are not common and its diagnostic features and management strategies are to be analyzed. In a literature review we analyze all purulent extraoral complications’ manifestations (abscesses, phlegmons, sialo-cutaneous fistulae, and tender cutaneous nodules).
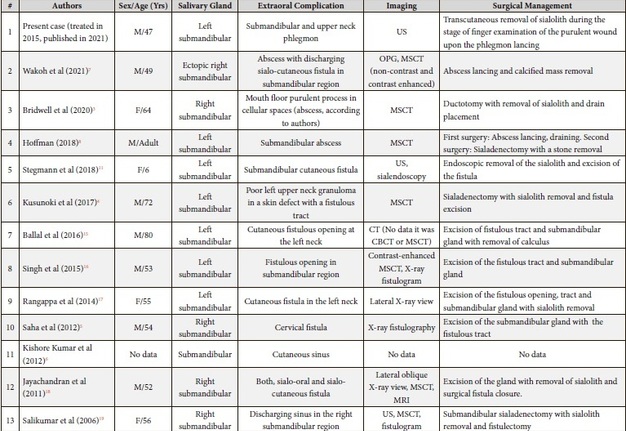
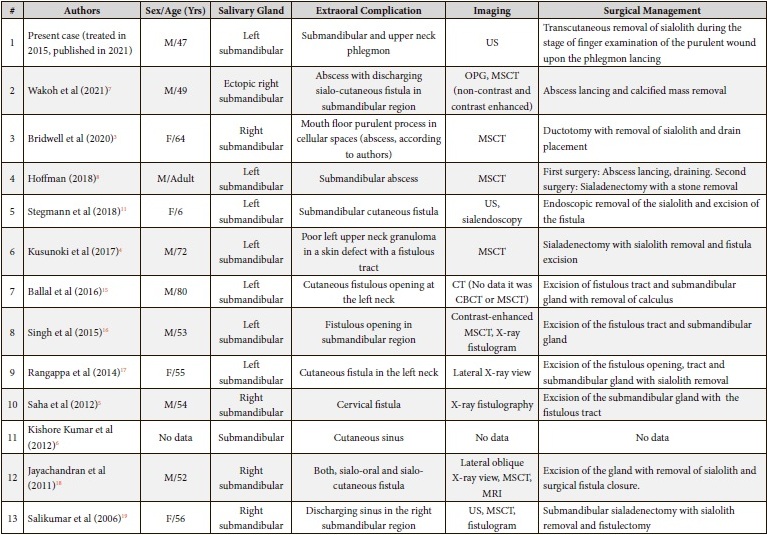
Table 1 is presenting our literature review of submandibular sialolithiasis complications and its management strategies based on the reviews of Ha et al (2020),14 Wakoh et al (2021)7.
TABLE 1. Literature Review of Submandibular Sialolithiasis with Purulent Extraoral Complications’ Manifestations and Its Management.
Among all 24 published cases (Table 1) of submandibular sialolithiasis with extraoral complications in the majority of cases (n = 17) there were noted the cutaneous fistulous tracts (in 69.56 percent), collection of pus in cellular space – in 5 cases (in 21.74 percent), and tender cutaneous nodule – in 2 cases (in 8.7 percent).
Among 16 fistulous cases, in two cases both sialo-oral and sialocutaneous fistulae were noted from one calculus, and in one case – the fistula located in a tissues with a resolution of the submandibular abscess.
Among five abscess/phlegmon cases, the abscess with discharging fistula was noted in one case (Wakoh et al)7.
Bridwell et al presented the description and computed tomography of an obstructed submandibular sialolith with abscess mimicking Ludwig's angina.3
Henry Hoffman presented an adult patient with submandibular region abscess due to the submandibular gland sialolithiasis, obstruction disease, and acute infection.8 In the reported institution`s protocol, the step by step management strategy was perfectly highlighted with a purpose to be a helpful guidelines for other practitioners designed to bridge the gap between procedural concepts and their implementation.25
Among five calculus-associated abscesses presentations and descriptions in three cases (Cartwright and Hardingham, Hoffman, and Wakoh et al)2,8,7 a limited collection of pus was noted, and in two cases (Bridwell et al and our case)3 the purulent process was diffuse and localized in two or more anatomical regions.
Worth of attention is the classification proposed by the authors from Japan who classified all submandibular gland sialolith-associated fistulas into four types7:
-
Sialo-oral fistula.26
-
Sialo-cutaneous fistula.4–6,11–13,15–17,19–21,23,24
-
Sialo-pharyngeal fistula (synonym: sialo-parapharyngeal fistula).27
-
Sialo-oro-cutaneous fistula.18,22
Wakoh et al presented the case of cutaneous fistula related with ectopic submandibular gland sialolith.7 Ha et al (2020) exhibited a sialo-cutaneous fistula but with no evidence of submandibular gland sialolith. In their cases the diagnosis of submandibular sialadenitis was established and the conservative treatment helped to eliminate the symptoms.14
Cases with intraoral complications of submandibular sialolithiasis (like submandibular duct fistula, etc.) were excluded from this discussion and can be analyzed in further studies. Despite the fact that in the report of Chandak et al (2012) the case with diagnosis of acute submandibular sialadenitis complicated with abscess was established there was no radiological evidence of sialoliths in submandibular gland.28
In the reported cases, some authors combined multiple diagnostic tools, like Jayachandran et al (X-ray, MSCT, MRI),18 others used a single one, like Hoffman (MSCT)8. Among 24 complication cases presented in the Table 1, computed tomography (non-contrast/contrast enhanced) was used in 10 cases, OPG – in three cases, X-ray – in five cases, X-ray fistulography – in three cases, fluoroscopy – in one case, US – in four cases, MRI – in 1 case, sialoendoscopy – in one case, and X-ray sialography – in one case. Thus, despite the fact that in the majority of cases (n = 10) the teams had chosen CT, ultrasonography (n = 4) has an undiscovered potential among surgeons.
US became a vital diagnostic tool for pathology detection in different glands―thyroid,29 lymphatic (ie, lymph nodes),30 and salivary ones31. Katz et al are more than right pointing out that a clinical US is to be indicated as soon as the first symptoms of sialadenitis occur.32 US is more than useful in the detection of structural changes of the salivary gland parenchyma, vascularization, condition of the duct system, sialoliths9,10 and even mucous plugs31. The authors note that approximately 20 to 40% of the salivary stones are not opaque on plain radiography, but most of these sialoliths are visible upon sialography.32 2.0-mm and longer sialoliths can be detected on gray scale US.32
Practitioners must keep in mind the possible calcifications in the area of major salivary glands as potential mimickers of sialoliths. These can be: healed tuberculous lymphadenitis, phleboliths, tonsilloliths, segmental ossification of the stylohyoid ligament.33 So, analysis of the anamnesis data, complaints and radiological features can significantly help in differential diagnostics.
In different countries, the purulent process presented in our case can be described by different terms. In English-speaking countries the term abscess34 is usually used, and in some of East European countries (Ukraine, etc.) the term phlegmon can be used for the similar condition. In general, phlegmon is an acute, clearly not limited purulent inflammation of cellular tissue.35 And abscess is a cavity filled with pus and delimited from the surrounding tissues by a pyogenic membrane.35 In this particular case the term phlegmon was used to describe the spread of the purulent process up to two anatomical regions.
In general, based on our literature search, the transcutaneous removal of submandibular gland sialoliths was reported in 4 cases. And our case became the fifth one. More than rare case of cutaneous exfoliation of the submandibular gland sialolith was recorded Karengera et al (1998).21 Very unusual two cases of the submandibular salivary stones migration in the cutaneous direction was described by Drage et al (2005).13 In 2021, Wakoh et al also highlighted the submandibular gland calculus migration to subcutaneous tissue.7 Calculi removal in those three cases7,13 was similar with our case in which the gland was preserved.
CONCLUSIONS
Ultrasound imaging is still underestimated and not enough popularized among head and neck and oral and maxillofacial surgeons. Presented case and published reports show the usefulness of this constantly developing diagnostic technique in a combination with knowledge of possible extraoral purulent complications’ and its management.
PATIENT CONSENT
The patient provided written consent for the use of his images.
AUTHOR CONTRIBUTIONS
Conceptualization: Fesenko II. Data acquisition: Savchuk LA. Data analysis, interpretation, and drafting of the manuscript: Fesenko II. Critical revision of the manuscript: Savchuk LA, Fesenko II. Approval of the final version of the manuscript: both authors.
ACKNOWLEDGEMENTS
We would like to thank Professor Henry T. Hoffman, MD, Iowa City, Iowa, United States for the kind support in preparing the manuscript.
REFERENCES (35)
-
Koch M, Sievert M, Iro H, Mantsopoulos K, Schapher M. Ultrasound in inflammatory and obstructive salivary gland diseases: own experiences and a review of the literature. J Clin Med 2021;10(16):3547. Crossref
-
Cartwright KAV, Hardingham M. Abscess formation by Haemophilus paraphrophilus secondary to a submandibular salivary calculus. J Infect 1983;6(1):101–2. Crossref
-
Bridwell RE, Oliver JJ, Griffiths SA, Long B. Sialolithiasis with abscess: an uncommon presentation of a Ludwig's angina mimic. Am J Emerg Med 2020;38(6):1295.e1–1295.e2. Crossref
-
Kusunoki T, Homma H, Kidokoro Y, Yanai A, Hara S, Kobayashi Y, To M, Wada R, Ikeda K. Cervical fistula caused by submandibular sialolithiasis. Clin Pract 2017;7(4):985. Crossref
-
Saha S, Jha A, Navneet Kaur N. Unusual cause of orocutaneous fistula in the neck. Case Rep Surg 2012;2012:658536. Crossref
-
Kishore Kumar RV, Devireddy SK, Gali RS, Chaithanyaa N, Chakravarthy C, Kumarvelu C. Cutaneous sinuses of cervicofacial region: a clinical study of 200 cases. J Maxillofac Oral Surg 2012;11(4):411–5. Crossref
-
Wakoh M, Goto TK, Matsuzaka K, Shibahara T, Kamio T. Sialo-cutaneous fistula with ectopic submandibular gland sialolith, revealing a hidden ipsilateral enlarged and elongated styloid process: a consideration based on CT findings. Oral Radiol 2021;37(2):336–44. Crossref
-
Hoffman HT, editor. Iowa head and neck protocols “submandibular abscess from stone (sialolithiasis, neck abscess)” [document on the internet]; 10 Dec 2018 [сited 23 Oct 2021]. Available from: Link
-
Knopf A. Sonography of the major salivary glands. In: Ultrasonography of the head and neck. Welkoborsky HJ, Jecker P, editors. 1st ed. Cham, Switzerland: Springer Nature; 2019:235−57. Crossref
-
Tymofieiev OO, Cherniak OS. Ultrasound in the detection of floating sialoliths. J Diagn Treat Oral Maxillofac Pathol 2019;3(8):196−7. Crossref
-
Stegmann A, Iro H, Koch M. Pediatric submandibular gland sialolithiasis with salivary–cutaneous fistula: case report on gland–preserving treatment with combined endoscopic–transcutaneous surgery. Am J Otolaryngol Head Neck Surg 2018;1(1):1003.
-
Abe H, Kuroda K, Toma H, Takeyama K, Oka M. A case of submandibular sialolithiasis with the fistula in the lateral neck. Jpn J Oral Maxillof Surg 1990;36(12):2790–3. Crossref
-
Drage NA, Brown JE, Makdissi J, Townend J. Migrating salivary stones: report of three cases. Br J Oral Maxillofac Surg 2005;43(2):180–2. Crossref
-
Ha DL, Ryu HS, Kim GW, Kim BS, Ko HC, Kim MB, Lee HJ. Fistula of the submandibular gland presenting as a painful mass in the neck: a rare case. Ann Dermatol 2020;32(1):81–3. Crossref
-
Ballal R, Banu K, Pandya K. A Submandibular sialolith of an unusual size presenting with a cervical fistula mimicking a branchial fistula: a case report. J Health Allied Sci 2016;6(2):66–8. Crossref
-
Singh R, Bhagat S, Bhagat R and Singh B. Submandibular gland sialolithiasis presenting as fistula in the neck–a case report. Austin J Otolaryngol 2015;2(4):1040.
-
Rangappa VB, Soumya MS, Sreenivas V. Salivary fistula with a calculus!! Int J Head Neck Surg 2014;5(2):96–8. Crossref
-
Jayachandran S, Bakyalakshmi K, Singh K. Giant submandibular sialolith presenting with sialocutaneous and sialo-oral fistula: a case report and review of literature. J Indian Acad Oral Med Radiol 2011;23(5):491–4. Crossref
-
Salilkumar K, Gopakumar KP, Divya GM, Sindhu BS. An unusual sequel of submandibular gland calculus-A case report. Indian J Otolaryngol Head Neck Surg 2006;58(3):303–4. Crossref
-
Almasri MA. Management of giant intraglandular submandibular sialolith with neck fistula. Annal Dent Univ Malaya 2005;12(1):41–5. Crossref
-
Karengera D, Yousefpour A, Reychler H. Unusual elimination of a salivary calculus. A case report. Int J Oral Maxillofac Surg 1998;27(3):224–5. Crossref
-
Paul D, Chauhan SR. Salivary megalith with a sialo-cutaneous and a sialo-oral fistula: a case report. J Laryngol Otol 1995;109(8):767–9. Crossref
-
Asfar SK, Steitiyeh MR, Abdul-Amir R. Giant salivary calculi: an orocervical fistula caused by a submandibular gland calculus. Can J Surg 1989;32(4):295–6.
-
Druez W, De Wolf JP, Tant L. Cutaneous fistula caused by submandibular lithiasis [in French]. Acta Stomatol Belg 1982;79(4):269–71.
-
Citing the Iowa protocols (use as a reference) [document on the internet]; 20 Feb 2020 [сited 23 Oct 2021]. Available from: Link
-
Szalma J, Orsi E, Nyárády Z, Szabó G, Olasz L. Submandibular sialolith: case report and review of the literature [in Hungarian]. Fogorv Sz 2008;101(6):219−23.
-
Panuganti BA, Baldassarre RL, Bykowski J, Husseman J. Chronic sialadenitis with sialolithiasis associated with parapharyngeal fistula and tonsillolith. Radiol Case Rep 2017;12(3):519−22. Crossref
-
Chandak R, Degwekar S, Chandak M, Rawlani S. Acute submandibular sialadenitis―a case report. Case Rep Dent 2012;2012:615375. Crossref
-
Novosel T, Jecker P. Ultrasound of the thyroid gland. In: Welkoborsky H, Jecker P, editors. Ultrasonography of the head and neck. 1st ed. Cham, Switzerland: Springer Nature; 2019:259–78. Crossref
-
Tymofieiev OO, Ushko NO, Fesenko II, Tymofieiev OO, Yarifa MO, Cherniak OS. Suppurative mastoid lymphadenitis mimicking mastoiditis: a case report. J Korean Assoc Oral Maxillofac Surg 2021;47(5):398−402. Crossref
-
Cherniak OS, Fesenko II. Effectiveness of ultrasound in verification of the mucus plugs and sialoliths of the Wharton`s duct. J Diagn Treat Oral Maxillofac Pathol 2019;3(5):144−53. Crossref
-
Katz P, Hartl DM, Guerre A. Clinical ultrasound of the salivary glands. Otolaryngol Clin North Am 2009;42(6):973−1000. Crossref
-
Mandel L. Tuberculous cervical node calcifications mimicking sialolithiasis: a case report. J Oral Maxillofac Surg 2006;64(9):1439–42. Crossref
-
Wong S, Dai E, Tang E, Ahuja AT. Neck abscess. In: Essential radiology for medical students, interns and residents. Ahuja AT, Antonio GE, Nung RC, Sitt JC, Yu JW, Wong SS, Dai EY, Law EK, Tang EW, Yuen BT, editors. Kyiv, Ukraine: OMF Publishing; 2017:3−6.
-
Tymofieiev OO. Maxillofacial surgery and surgical dentistry [in Russian]. Volume 1. 1st ed. Kyiv: All-Ukrainian Specialized Publishing House “Medicine”; 2020.