July 31, 2021
https://doi.org/10.23999/j.dtomp.2021.7.1
J Diagn Treat Oral Maxillofac Pathol 2021;77–86.
Under a Creative Commons license
HOW TO CITE THIS ARTICLE
Demidov VH, Khrulenko SI. Sialoliths of submandibular gland and Wharton’s duct: orthopantomography. J Diagn Treat Oral Maxillofac Pathol 2021;5(7):77–86.
SUMMARY
Orthopantomography (OPG), which is also known as panoramic radiography, pantomography, and panoramic imaging, proved its efficacy in infection, trauma, jaw lesions, tumor cases, etc. Calcification of the soft tissues in perimaxillary and perimandibular regions can also be visualized on OPG images. Reports clearly showed sialolith occurrence in the parotid gland in 10%, in submandibular gland in 83%, and in sublingual and minor salivary glands in 7%. Typically, sialoliths are visualized on the panoramic radiographs as radiopaque lesions. They are of round or oval shape, cylindrical or irregularly-shaped calcifications. Only in limited cases, sialoliths can be X-ray negative. The research data shows – from 10 to 20% the salivary stones are radiolucent. Digital OPG combines a lot of advantages. In summary, digital orthopantomography proved its efficacy in diagnostics of sialoliths located in the submandibular gland and its duct. Simultaneously, OPG is more than useful for diagnosis establishment and control of treatment for neighboring specialties.
INTRODUCTION
Sialolithiasis of the submandibular gland to some moment can be asymptomatic or can lead to symptoms of obstructive sialadenitis. According to the 10-year experience of the Department of Maxillofacial Surgery, Shupyk National Healthcare University of Ukraine, calculous submaxillitis occurs in 98.2% of patients, and calculous parotitis – only in 1.8% of all calculous sialadenitis (Tymofieiev, 2012).1 In their observations, salivary stones in the sublingual gland were not detected. Nikulin et al (2020) presented the case of sublingual gland sialolithiasis with description of ultrasound appearance.2 Study of Lommen et al (2021) revealed that in 58.6% of cases the sialoliths is localized in submandibular glands and in 41.4% – in the parotid gland.3 Other reports showed sialolith occurrence in the parotid gland in 10%, in submandibular gland in 83%, and in sublingual and minor salivary glands in 7%.4–5
Stone size can vary from less than 1 mm (microsialolith) (Demidov and Ripolovska, 2019) to giant ones, reaching 3.5 cm (Goh et al, 2016), 3.7 cm (Omezli et al, 2016), or even 5.5 cm (megasialolith) (Raksin et al, 1975).6–9
For example, the case published in 2019 revealed that number of sialoliths in the intraglandular duct system of the submandibular gland specimen can reach 8 stones (Demidov and Ripolovska, 2019).6
A lot of basic imaging techniques (unenhanced computed tomography [CT], magnetic resonance imaging [MRI], different Х-ray, ultrasonography, sialoendoscopy, and different sialography imaging techniques) for sialolith detection are applied around the globe (Rzymska-Grala et al, 2010).10 In some countries (like United States) the leading imaging for that purpose is unenhanced CT,11 in others (like European countries) ultrasonography and X-ray techniques are equally popular.10 Application of orthopantomography (OPG) in our hospital became a new first line imaging for the patients with obstructive sialadenitis symptoms.
OPG, which is also known as panoramic radiography, pantomography (Benson, 2014),12 and panoramic imaging, proved its efficacy in infection, trauma, jaw lesions, tumor cases, etc. Calcification of the soft tissues in perimaxillary and perimandibular regions can also be visualized on OPG images (Huang et al, 2009).13 Digital OPG combines a lot of advantages. Advantages and disadvantages of OPG were presented in detail study of Sidorenko de Oliveira Capote et al (2015).14 The main advantage of OPG over trans-oclusal endoral radiography is that all teeth, upper and lower jaw, maxillary sinuses, nasal cavity, and styloid processes are showed on the OPG image. And such OPG images can be used for the treatment by different dental specialists.
For identification of the sialoliths in the anterior part of the Wharton’s duct both an occlusal radiography (Jardim et al, 2011)15 (also known as mandibular occlusal radiography [Rzymska-Grala et al, 2010]10 and transoclusal endoral radiography [Shahoon et al, 2015])16 are useful. And for the stone identification in the posterior part of the duct, the transangular flour of the mouth radiography is recommended (Tymofieiev, 2012).1
In the literature (Benson, 2014) can be also found such terms as a cross-sectional mandibular occlusal projection radiography for examination of the anterior two thirds of the Wharton’s duct and an over-the-shoulder occlusal projection view for the posterior one third.12
Comparison of sialolith visualization on trans-oclusal endoral radiography versus OPG is highlighted in the case series of Oteri et al (2011).17 The purpose of our essay is to present appearance of submandibular gland and its duct sialoliths on orthopantomography.
MATERIALS AND METHODS
OPG presented in this publication was obtained at panoramic x-ray machine (Planmeca ProMax® 2D S3, Planmeca, Helsinki, Finland), Kyiv Regional Clinical Hospital by an experienced x-ray technician (S.I.K., his experience – 25 years). The digital processing of radiographs was carried out using the Romexis Viewer software. The OPG images of the patients with submandibular gland sialolithiasis were retrospectively meticulously analyzed. OPG with radiopaque salivary stones were collected for this essay.
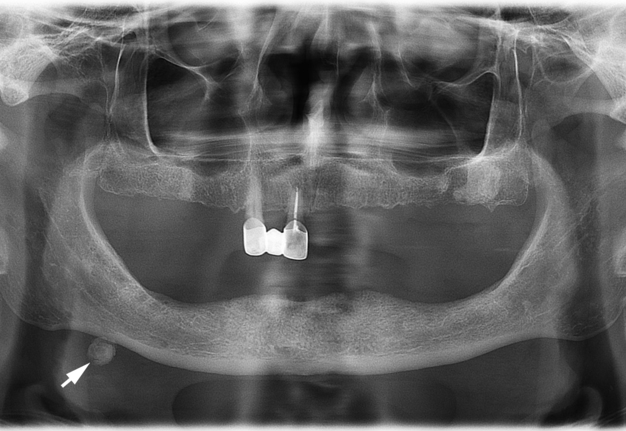
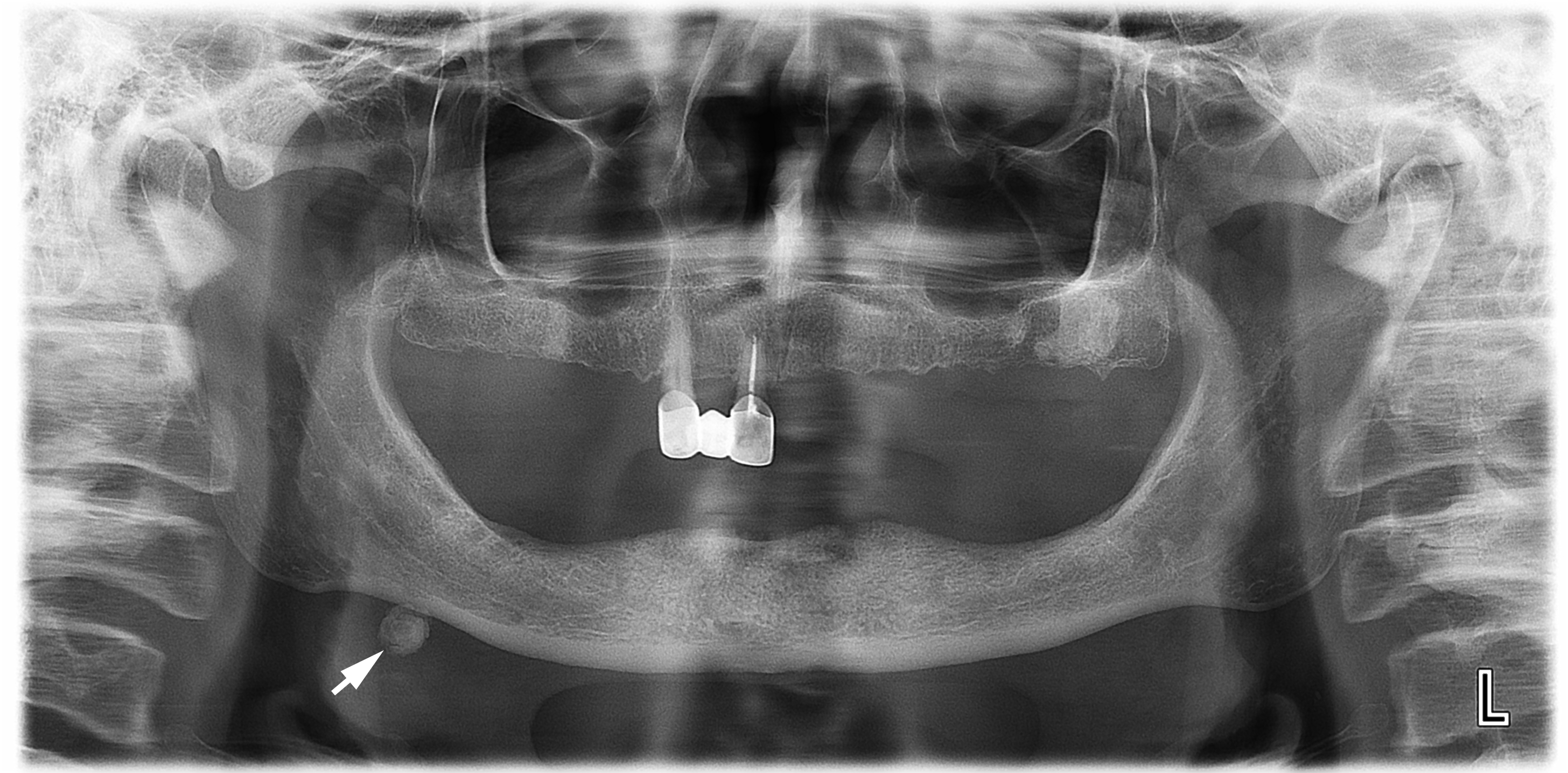
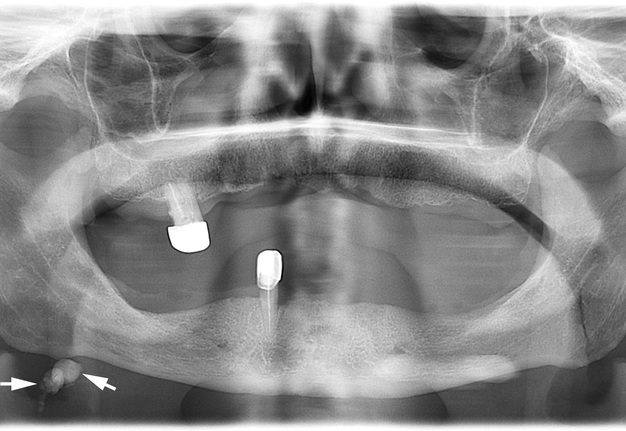
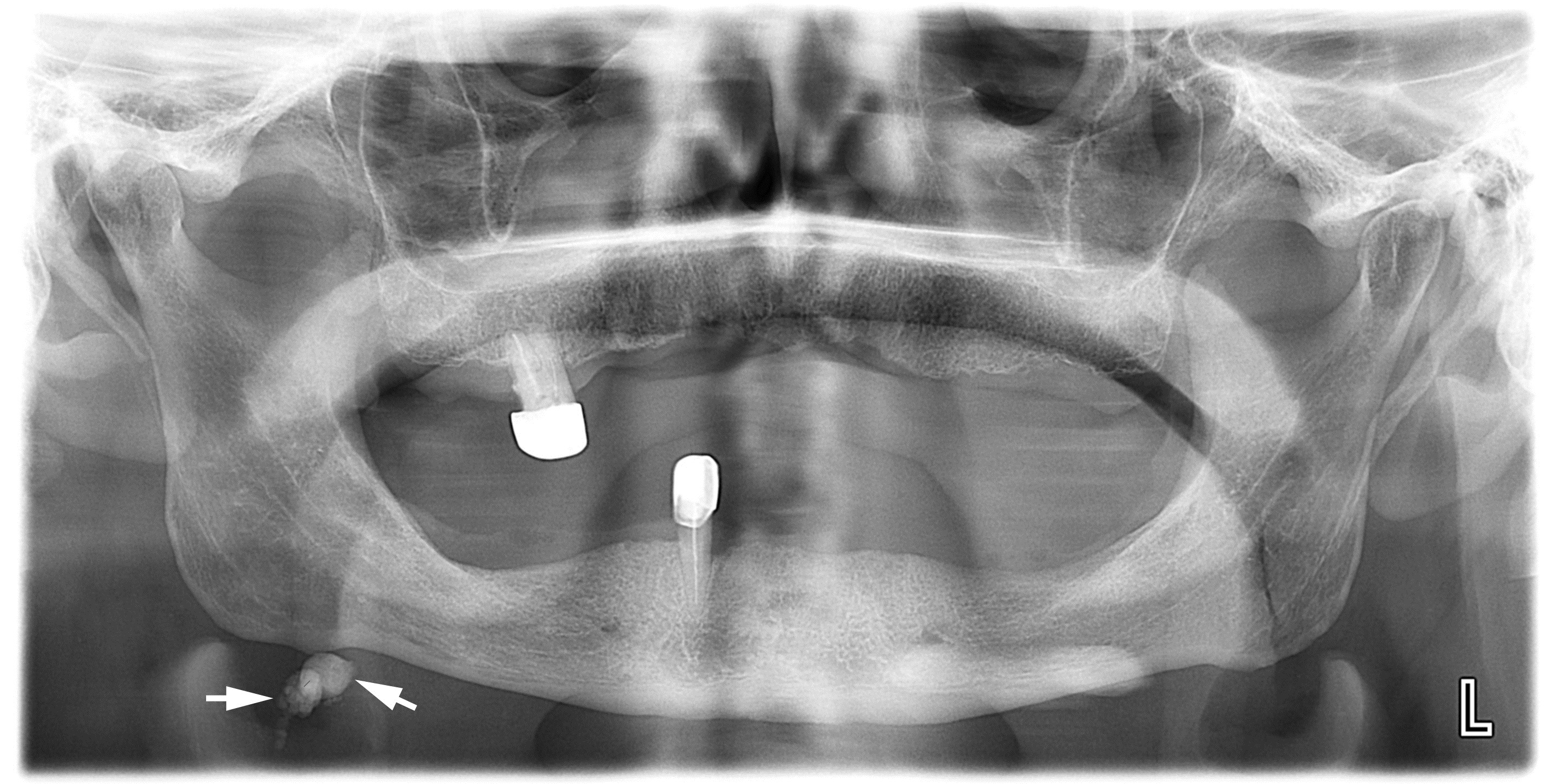
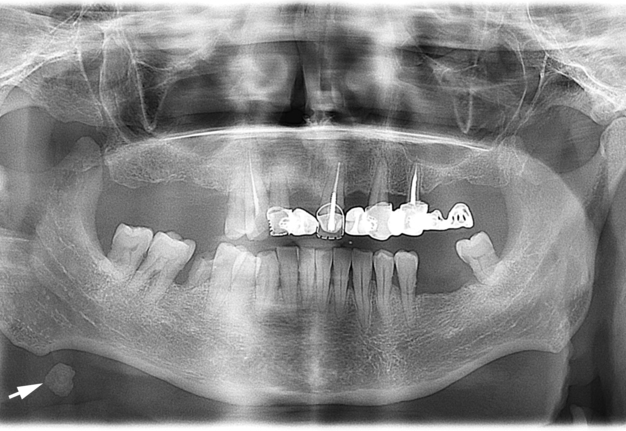
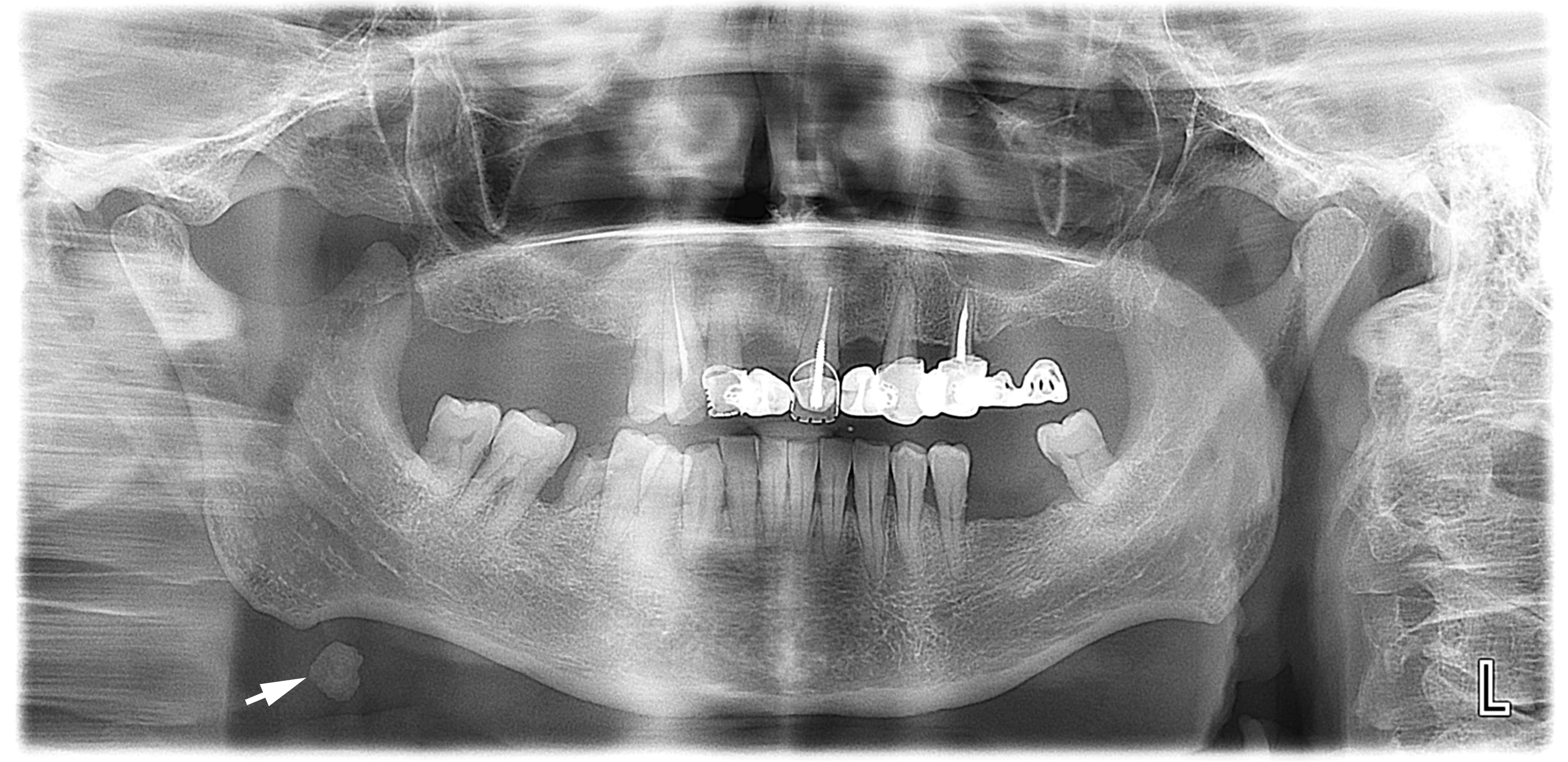
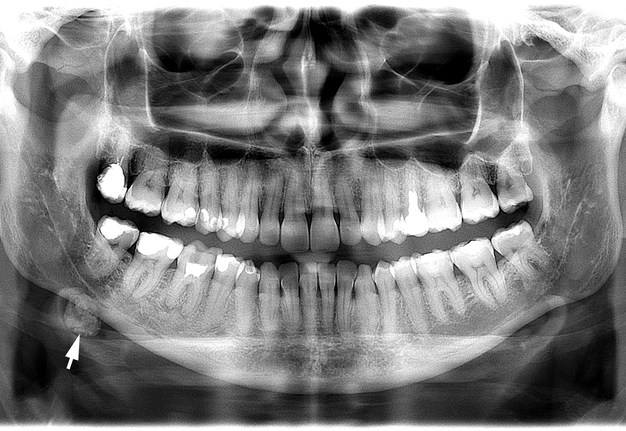
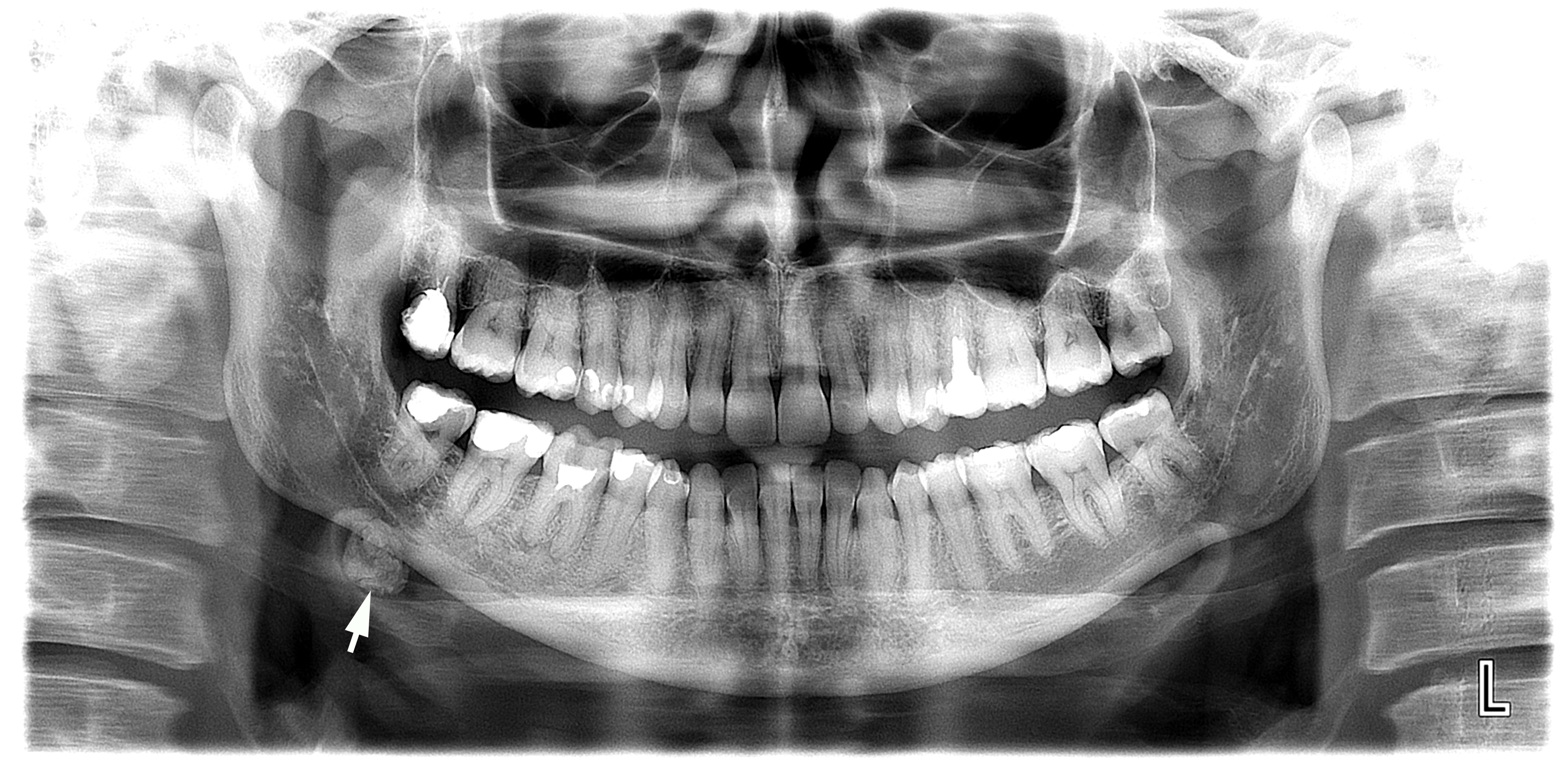
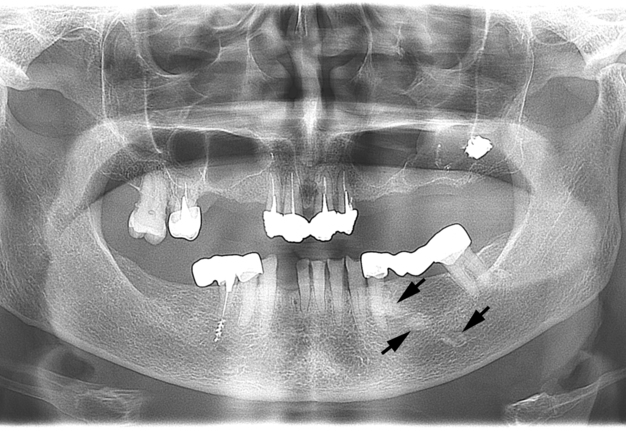
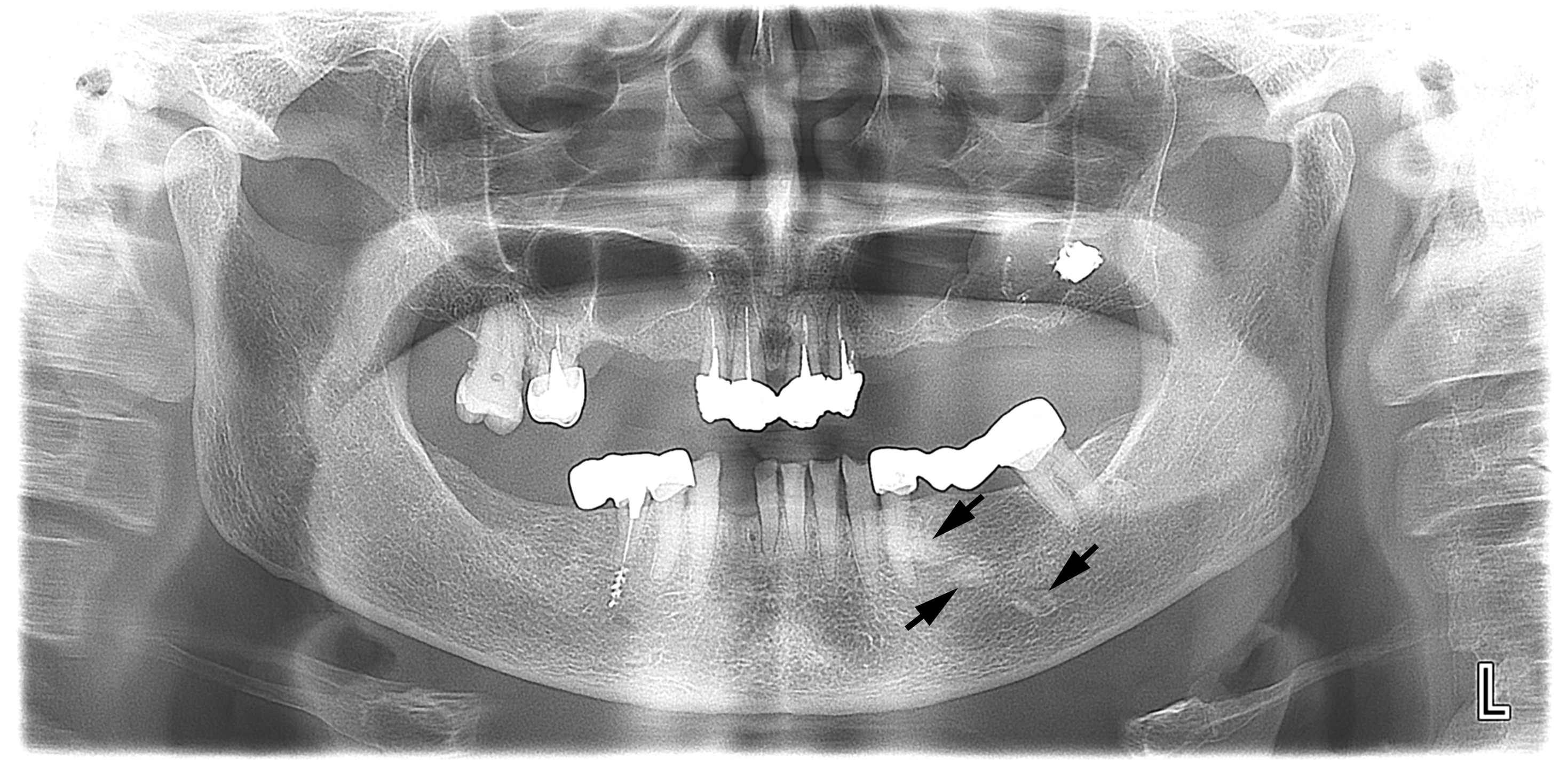
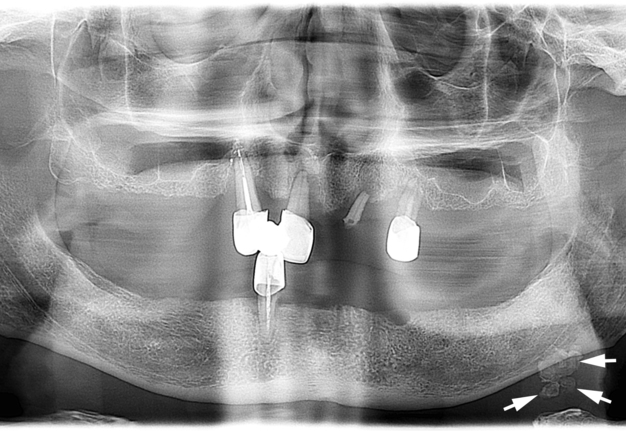
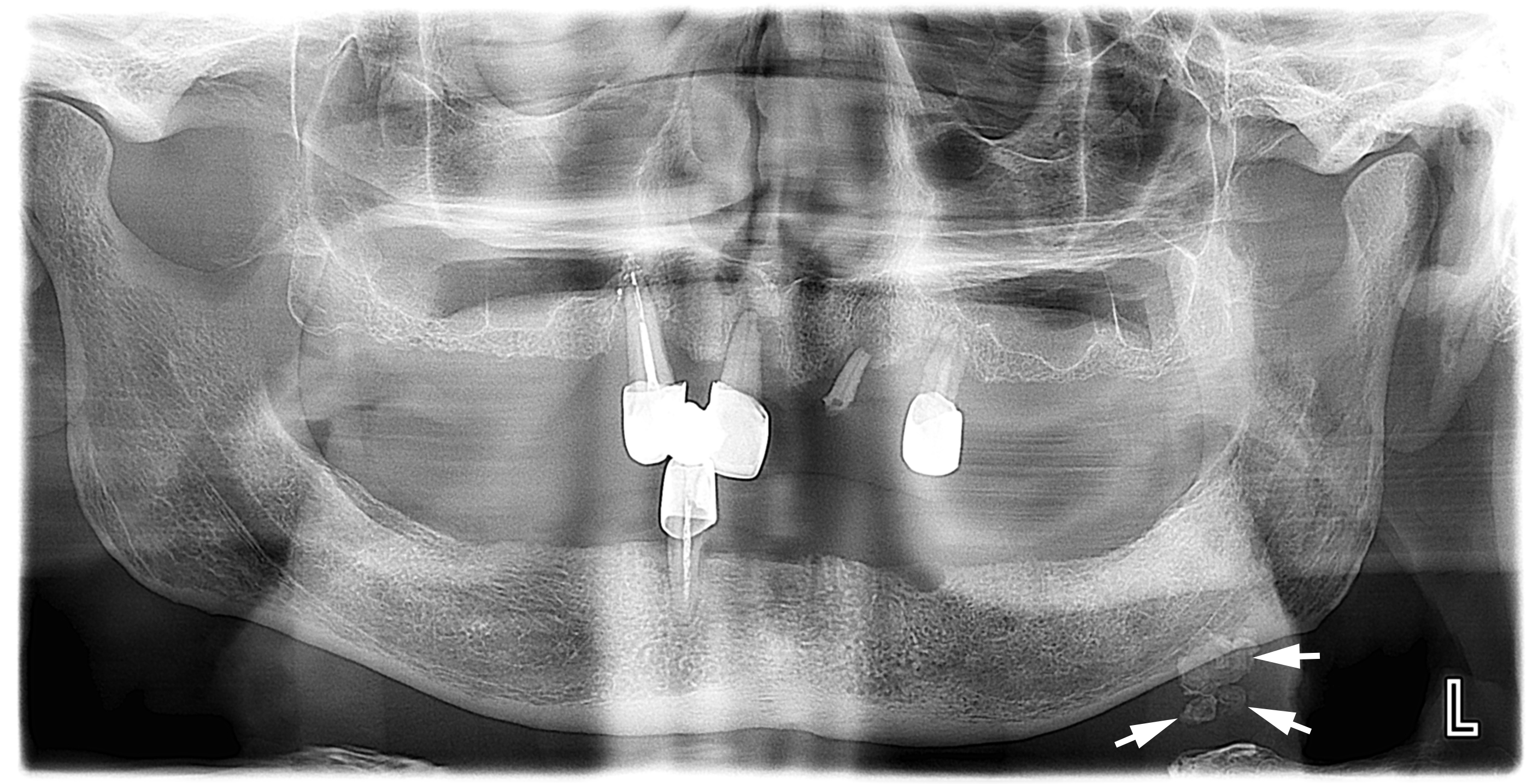
Eight patients of the age varied from 41 to 74 years (5 males and 3 females) with radiopaque lesions on OPG images were analyzed (Figs 1–8). One case (Fig 5) depicts two OPG – before and after sialolith removal. In five cases single sialoliths have been noted and in three cases – multiple sialoliths (two or three calculi).
FIGURE 5. Case 5: The orthomantomograms of 41-year-old gentleman before (A) and after (B) sialolith removal. The sialolith (arrow) is visualized as elongated radiopaque lesion overlapping the right mandibular body in the projection of posterior part of Wharton’s duct. Image B shows no evidence of sialolith. Time period between two images is 4 days.
DISCUSSION
Sialoliths are visualized on the panoramic radiographs as radiopaque lesions (Mumtaz, 2018).18 They look are of round (Huang et al, 2009)13 or oval shape (Larheim and Westesson, 2006),19 cylindric or irregularly-shaped (Huang et al, 2009)13 calcifications. Only in limited cases, sialoliths can be X-ray negative (Tymofieiev, 2012).1 The data of Larheim and Westesson (2006) shows ― from 10 to 20% of the salivary stones are radiolucent.19
Rzymska-Grala et al (2010) emphasized that submandibular gland sialoliths produce opacity only in 80–90 percent of the cases, while the calculi of the parotid salivary gland – only in 60 percent.10
According to Huang et al (2009), sialoliths in the Wharton’s duct are predominantly radiopaque (with a laminated or homogeneous structure).13
At OP, calculus can be overlapped on teeth, jaw bones (Oteri et al, 2011; Duong et al, 2019)17,20 or even hyoid bone (Mumtaz, 2018)18. When sialolith overlaps the mandibular bone it can mimic mandibular torus and osteoma.
According to Huang et al (2009), sialoliths should be differentiated from mandibular tori, osteomas, calcified lymph nodes, phleboliths and other vascular calcifications, tuberculosis of lymph nodes or of the salivary gland itself, calcified atherosclerotic plaques in major blood vessels, myositis ossificans, metastasis from distinct calcifying neoplasms.13
An important radiographic retrospective study performed by Aoun et al, which included 500 OPG images of patients with different pathology, showed that submandibular sialoliths were noted only in 1.8% of cases and parotid sialoliths only in 1.2% of cases.21
Cases presented in this essay clearly showed the radiologic features of sialoliths located in the submandibular gland and Wharton’s duct. Sialoliths in our cases are visualized as single or multiple radiopaque lesions being a completely different form – elongated, round, and teardrop-shaped.
CONCLUSIONS
In summary, digital orthopantomography proved its efficacy in diagnostics of sialoliths located in the submandibular gland and its duct. Simultaneously, OPG is more than useful for diagnosis establishment and control of treatment for neighboring specialties.
AUTHOR CONTRIBUTIONS
Conceptualization: Demidov VH. Data acquisition: Khrulenko SI. Data analysis, interpretation, and drafting of the manuscript: Demidov VH. Approval of the final version of the manuscript: both authors.
REFERENCES (21)
-
Tymofieiev OO. Manual of maxillofacial and oral surgery [Russian]. 5th ed. Kyiv, Ukraine: Chervona Ruta-Turs; 2012.
-
Nikulin DS, Fesenko II, Cherniak OS. Sialoliths in ipsilateral Bartholin`s and Wharton’s duct: the first clinical and ultrasound report. J Diagn Treat Oral Maxillofac Pathol 2020;4(7):112–8. Crossref
-
Lommen J, Schorn L, Roth B, Naujoks C, Handschel J, Holtmann H, Kübler NR, Sproll C. Sialolithiasis: retrospective analysis of the effect of an escalating treatment algorithm on patient-perceived health-related quality of life. Head Face Med 2021;17(1):8. Crossref
-
Taher AA. The incidence and composition of salivary stones (sialolithiasis) in Iran: analysis of 95 cases--a short report. Singapore Dent J 1989;14(1):33−5.
-
Cho SH, Han JD, Kim JH, Lee SH, Jo JB, Kim CH, Kim BJ. Removal of submandibular calculi by surgical method and hydraulic power with curved needle: a case report. J Korean Assoc Oral Maxillofac Surg 2017;43(3):182−5. Crossref
-
Demidov VH, Ripolovska OV. How multiple the submandubular gland sialoliths can be? J Diagn Treat Oral Maxillofac Pathol 2019;3(7):174–5. Crossref
-
Goh LC, Chitra BK, Shaariyah MM, Ng WS. Transcervical approach to the removal of a deep-seated giant submandibular calculus and the submandibular gland. BMJ Case Rep 2016;2016:bcr2016217514. Crossref
-
Omezli MM, Ayranci F, Sadik E, Polat ME. Case report of giant sialolith (megalith) of the Wharton's duct. Niger J Clin Pract 2016;19(3):414–7. Crossref
-
Raksin SZ, Gould SM, Williams AC. Submandibular duct sialolith of unusual shape and shape. J Oral Surg 1975;33(2):142–5.
-
Rzymska-Grala I, Stopa Z, Grala B, Gołębiowski M, Wanyura H, Zuchowska A, Sawicka M, Zmorzyński M. Salivary gland calculi - contemporary methods of imaging. Pol J Radiol 2010;75(3):25–37.
-
Fernandes RP, Salman S, Quimby A. Minimally invasive techniques for management of salivary gland pathology. J Diagn Treat Oral Maxillofac Pathol 2017;1(1):11−4. Crossref
-
Benson BW. Salivary gland diseases. In: Oral radiology. White SC, Pharoah MJ, editors. 7th edition. Elsevier Mosby; 2014:542–61.
-
Huang TC, Dalton JB, Monsour FN, Savage NW. Multiple, large sialoliths of the submandibular gland duct: a case report. Aust Dent J 2009;54(1):61–5. Crossref
-
Sidorenko de Oliveira Capote T, de Almeida Gonçalves M, Gonçalves A, Gonçalves M. Panoramic radiography — diagnosis of relevant structures that might compromise oral and general health of the patient. In: Emerging trends in oral health sciences and dentistry. Singh Virdi M, editor. IntechOpen; 2015. Crossref
-
Jardim EC, Ponzoni D, de Carvalho PS, Demétrio MR, Aranega AM. Sialolithiasis of the submandibular gland. J Craniofac Surg 2011;22(3):1128–31. Crossref
-
Shahoon H, Farhadi S, Hamedi R. Giant sialoliths of Wharton duct: report of two rare cases and review of literature. Dent Res J (Isfahan) 2015;12(5):494–7. Crossref
-
Oteri G, Procopio RM, Cicciù M. Giant salivary gland calculi (GSGC): report of two cases. Open Dent J 2011;5:90–5. Crossref
-
Mumtaz S. Sialolith infection. Br Dent J 2018;224(8):557–8. Crossref
-
Larheim TA, Westesson P-L. Salivary glands. In: Larheim TA, Westesson P-L. Maxillofacial imaging. 1st ed. Berlin, Heidelberg, Germany: Springer-Verlag; 2006:335–59.
-
Duong LT, Kakiche T, Ferré F, Nawrocki L, Bouattour A. Management of anterior submandibular sialolithiasis. J Oral Med Oral Surg 2019;25:16. Crossref
-
Aoun G, El-Outa A, Nasseh I. Sialoliths: a radiographic retrospective study. Curr Res Dent 2020;11(1):1. Crossref