April 29, 2022
https://doi.org/10.23999/j.dtomp.2022.4.2
J Diagn Treat Oral Maxillofac Pathol 2022;6:63–4.
Under a Creative Commons license
HOW TO CITE THIS ARTICLE
Rybak VA. Severe self-inflicted gunshot wound of the face. J Diagn Treat Oral Maxillofac Pathol 2022;6(4):63–4.
NATIONAL REPOSITORY OF ACADEMIC TEXTS
https://nrat.ukrintei.ua/en/searchdoc/2022U000183/
ARTICLE
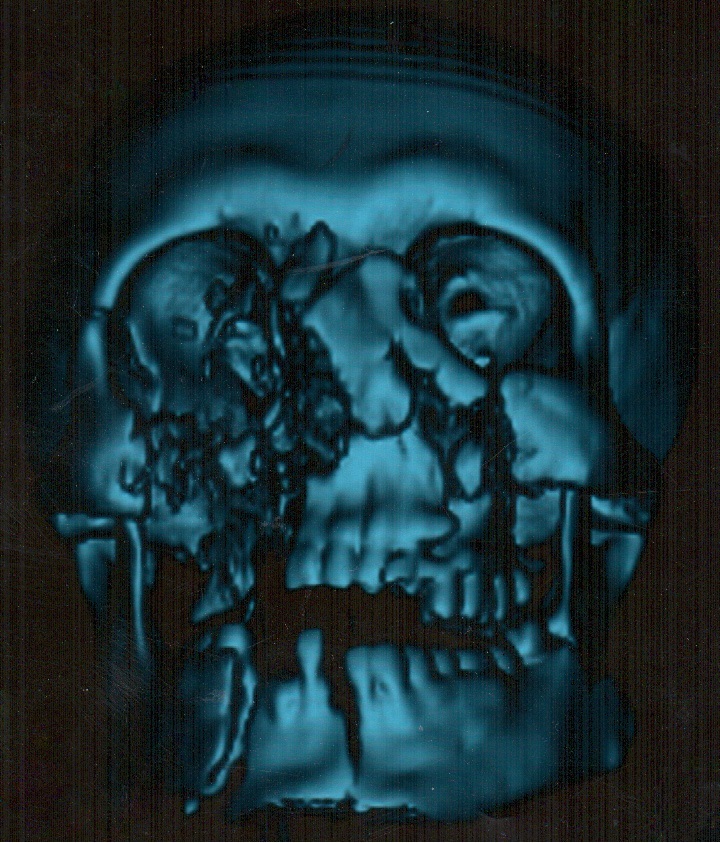
A 26-year-old male was transported to the hospital with a severe self-inflicted gunshot wound of the middle and lower face (Panel A) due to the suicide attempt. Three-dimensional computed tomography (CT) showed multiple site comminuted fracture of the facial skeleton including maxilla, mandible, right zygomatic, ethmoid, and nasal bones (Panel B). Also, the sockets of multiple avulsed teeth were noted. The patient was transported from the region several days after the injury. Due to the osseous and soft tissue loss, this type of gunshot wounds typically poses a considerable challenge to the oral and maxillofacial and plastic surgeons.2 Acute management in such cases includes resuscitative and life-saving measures.1 Timing of each surgical procedure should be chosen according to the patient condition, extent of the injury, and international recommendations.1 Operative principles include: (1) general considerations (all reconstructive options are to be taking into account, moreover, the volume of bone and soft tissue loss, functional and aesthetic purposes should be analyzed and planned very precisely), (2) skeletal fixation, (3) bone grafts, (4) soft tissue coverage, and even (5) a facial transplantation in some cases.1 In our case, the right eye enucleation (removal of the entire globe with all intraocular contents, while preserving orbital/periorbital structures) was done due to the severely ruptured globe.2,3 Typical indications for enucleation are severe eye trauma and blind, intraocular tumors, painful, and cosmetically disfiguring eyes.4 In case of evisceration the intraocular contents are removed from an intact sclera, extraocular muscle attachments and the orbital adnexa are preserved, with placement of an implant within the scleral shell with a purpose to retain orbital volume.3 Common indications for enucleation are unresponsive endophthalmitis and for improvement of cosmesis in a blind eye. The most common indication for orbital exenteration (removal of the globe and all orbital contents, including muscles, fat, optic nerve, lacrimal gland, nerves, periorbital bone, upper and lower lid complexes) is malignancy.5 ■ DTJournal.org
REFERENCES (5)
-
Volk AS, Shokri T, Sokoya M, Ducic Y, Hollier LH Jr. Facial gunshot wounds. Facial Plast Surg 2019;35(6):578–83. Crossref
-
Ben Simon GJ, Moisseiev J, Rosen N, Alhalel A. Gunshot wound to the eye and orbit: a descriptive case series and literature review. J Trauma 2011;71(3):771–8; discussion 778. Crossref
-
Reed D, Papp A, Brundridge W, Mehta A, Santamaria J, Valentin F, Davies B. Evisceration versus enucleation following ocular trauma, a retrospective analysis at a level one trauma center. Mil Med 2020;185(3–4):409–12. Crossref
-
Ababneh OH, AboTaleb EA, Abu Ameerh MA, Yousef YA. Enucleation and evisceration at a tertiary care hospital in a developing country. BMC Ophthalmol 2015;15:120. Crossref
-
Notz GM, Purdy N. Indication and technique of orbital exenteration. Oper Tech Otolaryngol 2018;29(4):218–21. Crossref