Surgery in the Area of Accessory Infraorbital Foramen and Nerve: Cone-Beam Computed Tomography versus Intraoperative Appearance
May 31, 2022
https://doi.org/10.23999/j.dtomp.2022.5.2
J Diagn Treat Oral Maxillofac Pathol 2022;6:71–76.
Under a Creative Commons license
HOW TO CITE THIS ARTICLE
Kuchynskyi AV, Fesenko II. Surgery in the area of accessory infraorbital foramen and nerve: cone-beam computed tomography versus intraoperative appearance. J Diagn Treat Oral Maxillofac Pathol 2022;6(5):71–6.
NATIONAL REPOSITORY OF ACADEMIC TEXTS
https://nrat.ukrintei.ua/en/searchdoc/2022U000186/
INSTITUTIONAL REPOSITORY
https://ir.kmu.edu.ua/handle/123456789/616
SUMMARY
We present a unique comparison of cone-beam computed tomography (CBCT) and intraoperative view of the accessory infraorbital foramen and nerve in a 60-year-old woman who was surgically treated due to the giant dentigerous cyst of the maxillary sinus from ectopic upper third molar. CBCT imaging demonstrates highest level of accuracy in verification of the accessory infraorbital foramina what makes this imaging technique a perfect tool for the surgery planning in the area of middle face. Avoidance of iatrogenic trauma of both infraorbital and accessory nerves will be ensured significantly in professionals who understand this topic. Oral and maxillofacial surgeons and doctors of neighboring specialties should be aware of such unusual anatomic variation as unilateral or even bilateral accessory infraorbital foramina and intraosseous nerve ramification.
INTRODUCTION
Direct visualization of infraorbital nerve (IN) with accessory infraorbital foramen (AIF) and nerve is not common during the maxillofacial surgery procedures. Bahrami et al (2016) presented an intraoperative view of the right duplicated IN upon the facial bones osteosynthesis.1 We remember, that part of the maxillary branch of the trigeminal nerve which is going in the orbital floor terms as IN. According to the available data, IN can give an accessory branch before2 and inside infraorbital canal3. Gruber in 1875 reported that number of IN foramens at every hemiface can reach even the number of 5.4 Understanding the anatomy of this anatomic area is important for local anesthesia performance5, percutaneous V2 (i.e., second branch of the fifth cranial nerve [trigeminal nerve]) ablation,3 nerve decompression,6 osteosynthesis, etc. No English-literature data of the comparison of the cone-beam computed tomography (CBCT) and intraoperative view of accessory infraorbital nerve (AIN) have been noted during the literature search. Thus, we present a unique comparison of computed tomography imaging and intraoperative view of the accessory infraorbital foramen and nerve in a 60-year-old woman who was surgically treated due to the gigantic follicular cyst of the maxillary sinus.
CASE REPORT
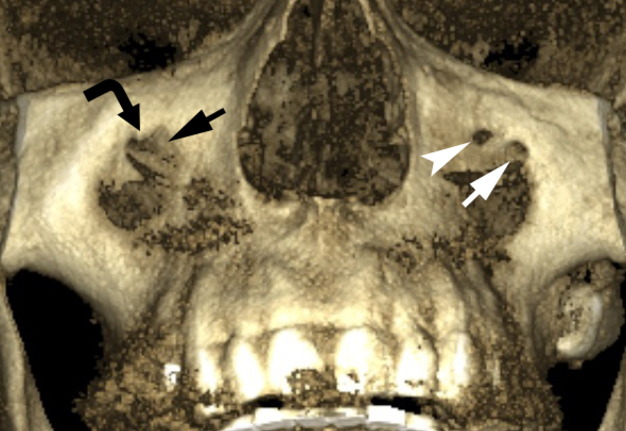
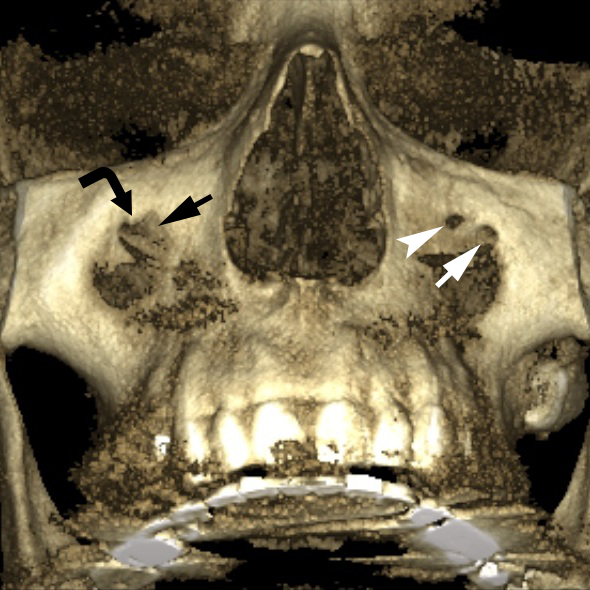
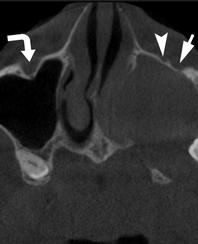
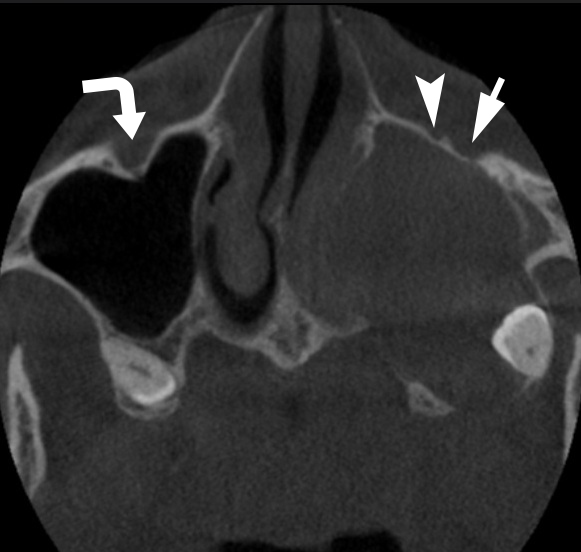
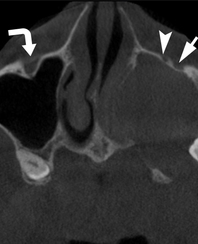
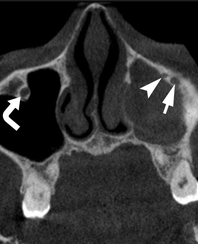
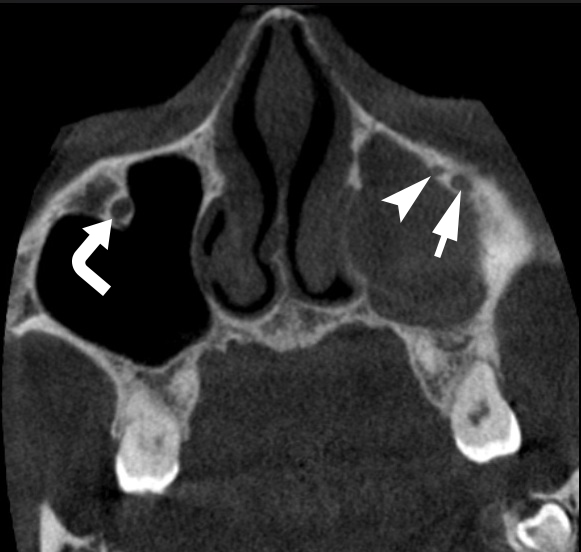
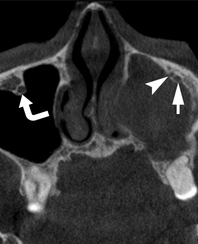
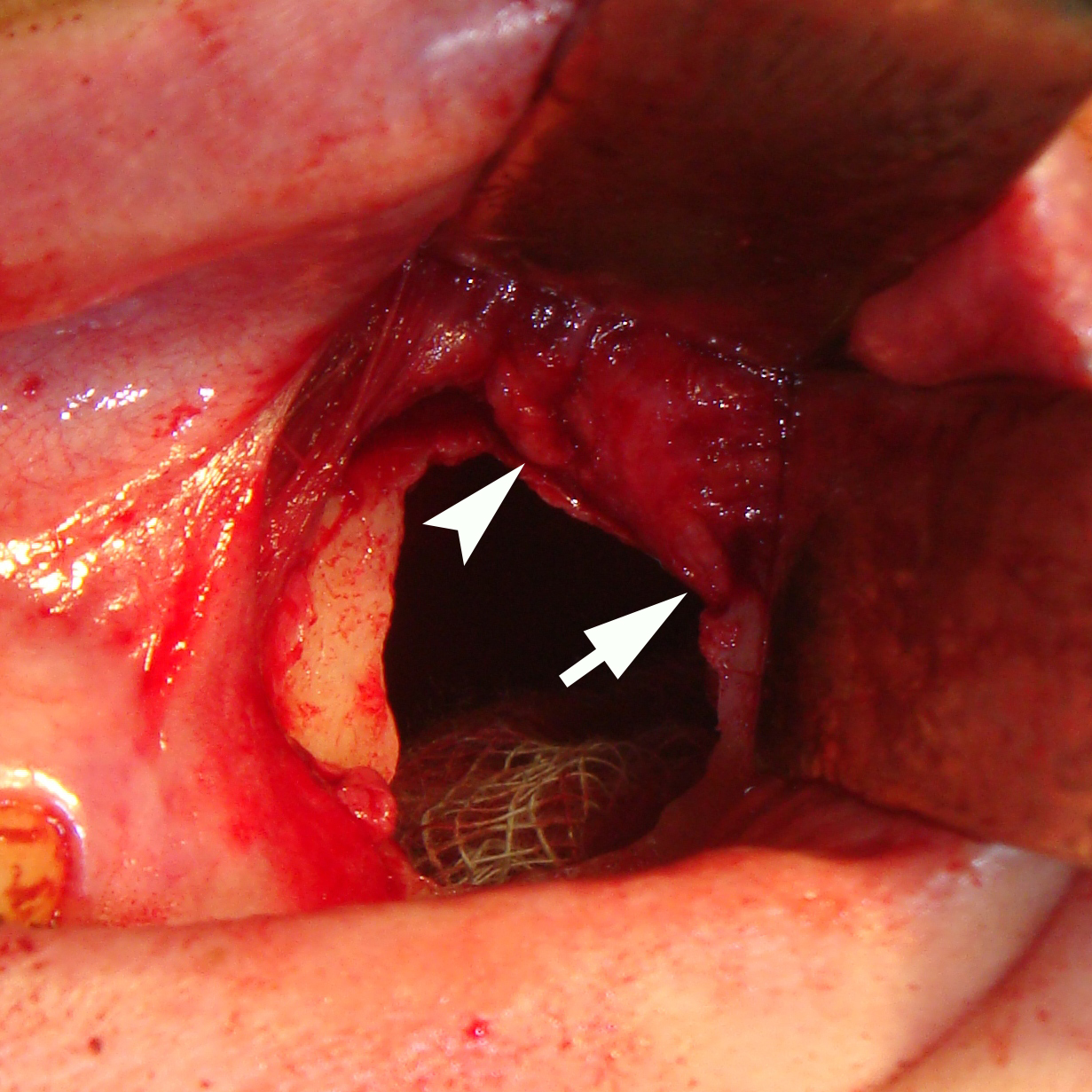
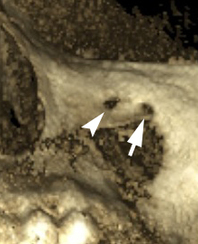
A case of 60-year-old female with a left eye tearing due to the nasolacrimal duct obstruction by gigantic follicular cyst of the left maxillary sinus from the upper left third molar was reported in the previous study.7 The preoperative CBCT (Planmeca ProMax 3D Max, Planmeca, Finland) (Fig 1) showed a small bony lingula above the wide right infraorbital foramen measured 4.62 × 3.11 mm. Left infraorbital foramen and accessory foramen measured 2.60 × 1.90 mm and 1.82 × 1.79 mm respectively. AIF was located 2.56 mm medially and slightly superiorly. The left infraorbital canal has bifurcated at the last third of its length (Fig 2). No CBCT data of accessory infraorbital canals and foramina at the right side have been noted on all scans. Two widely spaced infraorbital foramina with two thick INs were directly visualized (Fig 3B) upon the osteotomy of the anterior wall of the left maxillary sinus and cyst removal.
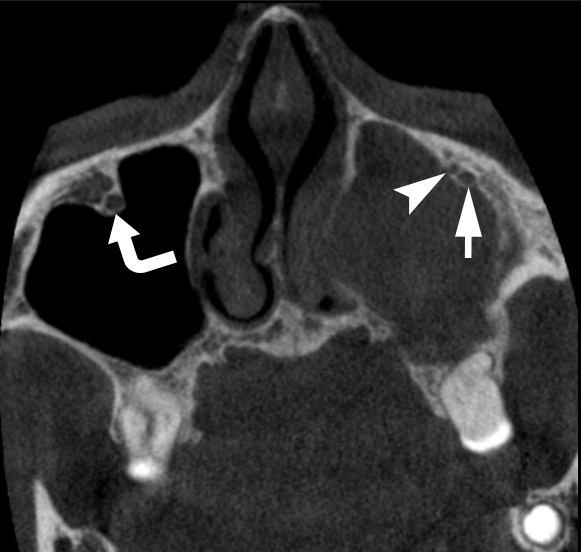
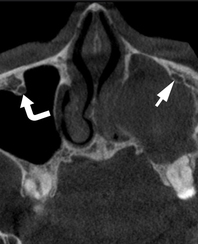
FIGURE 1. The preoperative three-dimensional CBCT image shows a small bony projection (i.e., lingula) (black curved arrow) above the wide right infraorbital foramen (black arrow) measured 4.62 × 3.11 mm. Left infraorbital foramen (white arrow) and accessory foramen (white arrowhead) measured 2.60 × 1.90 mm and 1.82 × 1.79 mm. Printed with permission and copyrights retained by I.I.F.
FIGURE 2. Comparison of preoperative anteriorly rotated axial CBCT scans. Image A shows right infraorbital canal (curved arrow) and left infraorbital canal (arrow) prior to bifurcation. Images B, C, and D show the course of right (curved arrow), left infraorbital canal (arrow) and accessory canal (arrowhead). No CBCT data of accessory infraorbital canal and foramen at the right side have been noted on all scans. Images E and F show right (curved arrow) and left infraorbital foramen (arrow) and accessory foramen (arrowhead). Printed with permission and copyrights retained by I.I.F.
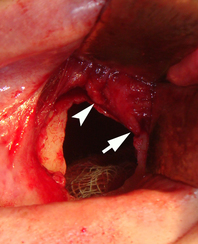
FIGURE 3. The preoperative three-dimensional CBCT image (A) shows the infraorbital foramen (arrow) and medially located accessory infraorbital foramen (arrowhead) at the left side. Two thick infraorbital neurovascular bundles were visualized intraoperatively (B): Arrow labels the left infraorbital nerve and arrowhead – the accessory infraorbital nerve. Printed with permission and copyrights retained by I.I.F.
DISCUSSION
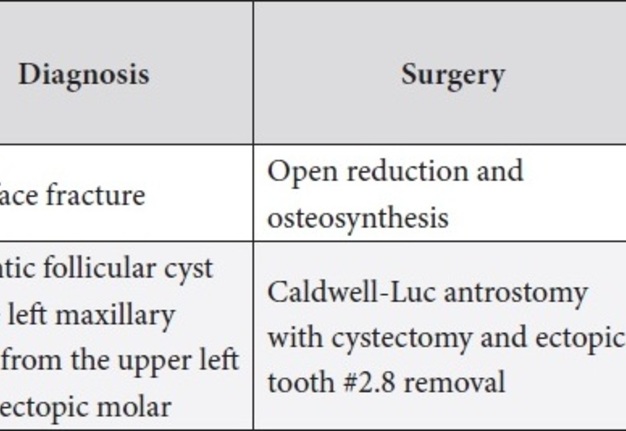
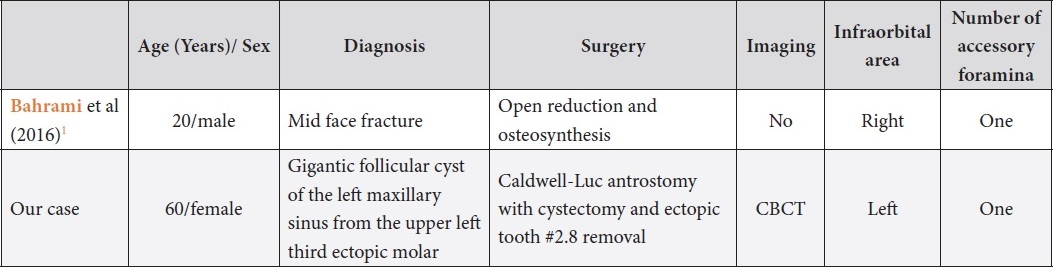
Analysis of the English-language literature showed that unilateral two separate IN branches during the cadaver dissection of a 69-year-old male highlighted by Tubbs et al (2010) looks very similar to our clinical case.3 The differences between case of the Bahrami et al (2016) with intraoperative AIN view and our case are presented in the Table 1.1
TABLE 1. Comparison of Published Cases with Intraoperative View of the Accessory Infraorbital Foramens and Nerves.
The analysis of 1,064 skulls by Bressan et al (2004) reveled that accessory infraorbital foramina (AIFa) were noted in 4.7 percent of skulls.8 Dissection of 44 hemifaces from 25 cadavers presented in the study of Shin et al (2020) showed that AIF can be found in 18.2 percent of cases.9 It is of interest that in 2.72 percent of cases the AIF was noted bilaterally.9
Presented cadaver study with 94 hemifaces, reported by Aziz et al (2020), showed the evidence of possible quadruple ipsilateral IN what is close to the INs number in the study of Gruber.10,4
Chandra and Kennedy (2004) emphasized that IN is particularly at risk during a Caldwell-Luc antrostomy11 which was done in our case. In the post-operative period, no hypoesthesia, paresthesia, or neuralgia has been noted.
A “classic location” of IN without AIN and with reference to the tissues for the nerve block performance is described by Shin et al (2020) what is extremely useful for understanding the extraoral route of anesthesia.12 Moreover, ultrasound-guided IN block is also proposed by Michalek et al (2013).13 Anyway, a meticulous computed tomography analysis before the IN block and midface bone surgery will make the anesthesia and surgery performance smoother.14 Recommendations of Kazkayasi et al (2003) and Iwanaga et al (2020) on the Le Fort osteotomy and AINs are also need to taken into account before surgery.15,16
One of the possible routes of pterygopalatine anesthesia (i.e., V2 nerve block) is a needle movement through the infraorbital canal (i.e., orbital route of maxillary nerve block).5 It is well to bear in mind that the diameter of the canal, its curvature, and presence of possible accessory canal can contribute to anesthesia performance failure.
The data of Canan et al (1999) will be helpful for doctors in anesthesia performance.17 The analysis of 229 maxilla revealed that single AIF was present in 11.5 percent of specimens and double AIF – in 1.28 percent of specimens.17
Hwang et al (2015) perfectly summarize 13 articles among the 166 PubMed searched papers with a term infraorbital foramen.18 They concluded that in 92.2 percent of AIN cases it`s located at the superomedial side of the infraorbital foramen.18 That knowledge is useful during anesthetization of the infraorbital area and maxillary bone.
Rusu et al (2020) insist on a need to distinguish true, false AIFa and the infraorbital lamina cribriformis.19 In their retrospective CBCT study of 200 patients, the AIFa at the sutura notha of the frontal process of maxillary bone is well illustrated.19
In summary, oral and maxillofacial surgeons and doctors of neighboring specialties should be aware of such unusual anatomic variation as unilateral or even bilateral accessory infraorbital foramina and intraosseous nerve ramification. Usage of cone-beam computed tomography proved its efficacy in verification of the accessory infraorbital foramina what make this imaging technique a perfect tool for the surgery planning in the area of middle face. Avoidance of iatrogenic trauma of infraorbital nerve and accessory nerve will be ensured significantly in professionals who understand this topic.
TERM OF CONSENT
No needed.
AUTHOR CONTRIBUTIONS
Conceptualization: Fesenko II. Data acquisition: Kuchynskyi AV, Fesenko II. Data analysis or interpretation: Kuchynskyi AV. Drafting of the manuscript: Fesenko II. Critical revision of the manuscript: Fesenko II, Kuchynskyi AV. Approval of the final version of the manuscript: all authors.
CONFLICT OF INTERESTS
The authors declare no conflict of interest.
FUNDINGS
No funding was received for this study.
REFERENCES (19)
-
Bahrami A, Saman M, Ducic Y. Duplicate infraorbital nerve–an uncommon anatomical variation. JSM Oro Facial Surg 2016;1(1):1001.
-
Jordan J. Double infraorbital nerve in man. Folia Morphol 1967;26:405–7.
-
Tubbs RS, Loukas M, May WR, Cohen-Gadol AA. A variation of the infraorbital nerve: its potential clinical consequence especially in the treatment of trigeminal neuralgia: case report. Neurosurgery 2010;67(3 Suppl Operative):onsE315; discussion onsE315. Crossref
-
Gruber W. Uber die infraorbitalen Kanale des Menschen und der Saugetiere [in German]. Mem Acad Imp Sci St Petersburg 1874;21:1–27.
-
Tymofieiev OO, Fesenko II. Anesthesia in oral and maxillofacial surgery. 1st edition. Kyiv: OMF Publishing; 2016. Crossref
-
Sosin M, De La Cruz C, Christy MR. Endoscopic-assisted infraorbital nerve release. Case Reports Plast Surg Hand Surg 2014;1(1):20–2. Crossref
-
Babkina TM, Shekera OG, Storozhchuk YO, Telukha KI, Nozhenko OA, Fesenko II, Zaritska VI, Snisarevskyi PP. Gigantic dentigerous cysts associated with the ectopic/impacted upper third molars: computed tomography analysis of nasolacrimal duct and osteomeatal complex obstructions and review of literature. J Diagn Treat Oral Maxillofac Pathol 2020;4(5):79–94. Crossref
-
Bressan C, Geuna S, Malerba G, Giacobini G, Giordano M, Robecchi MG, Vercellino V. Descriptive and topographic anatomy of the accessory infraorbital foramen. Clinical implications in maxillary surgery. Minerva Stomatol 2004;53(9):495–505.
-
Shin KJ, Lee SH, Park MG, Shin HJ, Lee AG. Location of the accessory infraorbital foramen with reference to external landmarks and its clinical implications. Sci Rep 2020;10(1):8566. Crossref
-
Aziz SR, Marchena JM, Puran A. Anatomic characteristics of the infraorbital foramen: a cadaver study. J Oral Maxillofac Surg 2000;58(9):992–6. Crossref
-
Chandra RK, Kennedy DW. Surgical implications of an unusual anomaly of the infraorbital nerve. Ear Nose Throat J 2004;83(11):766–7.
-
Shin KJ, Shin HJ, Lee SH. Location of the infraorbital foramen with reference to soft tissue landmarks for regional nerve blocks during midface surgery. Clin Anat 2020;1–5. Crossref
-
Michalek P, Donaldson W, McAleavey F, Johnston P, Kiska R. Ultrasound imaging of the infraorbital foramen and simulation of the ultrasound-guided infraorbital nerve block using a skull model. Surg Radiol Anat 2013;35(4):319–22. Crossref
-
Polo CL, Abdelkarim AZ, von Arx T, Lozanof S. The. morphology of the infraorbital nerve and foramen in the presence of an accessory infraorbital foramen. J Craniofac Surg 2019;30(1):244–53. Crossref
-
Kazkayasi M, Ergin A, Ersoy M, Tekdemir I, Elhan A. Microscopic anatomy of the infraorbital canal, nerve, and foramen. Otolaryngol Head Neck Surg 2003;129(6):692–7. Crossref
-
Iwanaga J, Kikuta S, Kusukawa J, Tomaszewski KA, Walocha JA, Tubbs RS. Anatomic study of accessory infraorbital nerves and foramina: application for a better understanding of complications of Le Fort fractures and osteotomy. J Oral Maxillofac Surg 2020;78(5):717–23. Crossref
-
Canan S, Asim OM, Okan B, Ozek C, Alper M. Anatomic variations of the infraorbital foramen. Ann Plast Surg 1999;43(6):613–7. Crossref
-
Hwang K, Lee SJ, Kim SY, Hwang SW. Frequency of existence, numbers, and location of the accessory infraorbital foramen. J Craniofac Surg 2015;26(1):274–6. Crossref
-
Rusu MC, Săndulescu M, Cârstocea L. False and true accessory infraorbital foramina, and the infraorbital lamina cribriformis. Morphologie 2020;104(344):51–8. Crossref