A Lower Lip Infection (Furuncle) Complicated by Abscess of the Lip, Suppurative Cheilitis Glandularis, Lip Necrosis, Septic Bilateral Multilobar Necrotizing (Destructive) Pneumonia, and Pleurisy (Pleuritis): A Case Report and Literature Review
September 30, 2023
J Diagn Treat Oral Maxillofac Pathol 2023;7:94–114.
DOI: 10.23999/j.dtomp.2023.9.1
Under a Creative Commons license
HOW TO CITE THIS ARTICLE
Morkotun V, Tymofieiev OO, Fesenko II, Chaikovskyi I, Kuzmenko F. A lower lip infection (furuncle) complicated by abscess of the lip, suppurative cheilitis glandularis, lip necrosis, septic bilateral multilobar necrotizing (destructive) pneumonia, and pleurisy (pleuritis): a case report and literature review. J Diagn Treat Oral Maxillofac Pathol 2023;7(9):94–114. https://doi.org/10.23999/j.dtomp.2023.9.1
NATIONAL REPOSITORY OF ACADEMIC TEXTS
https://nrat.ukrintei.ua/en/searchdoc/2023U000204/
SUMMARY
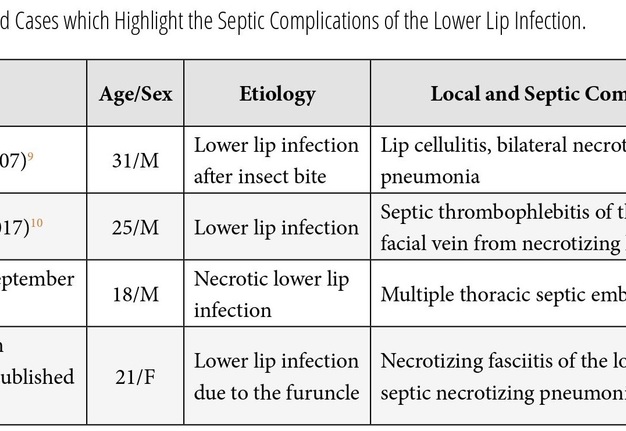
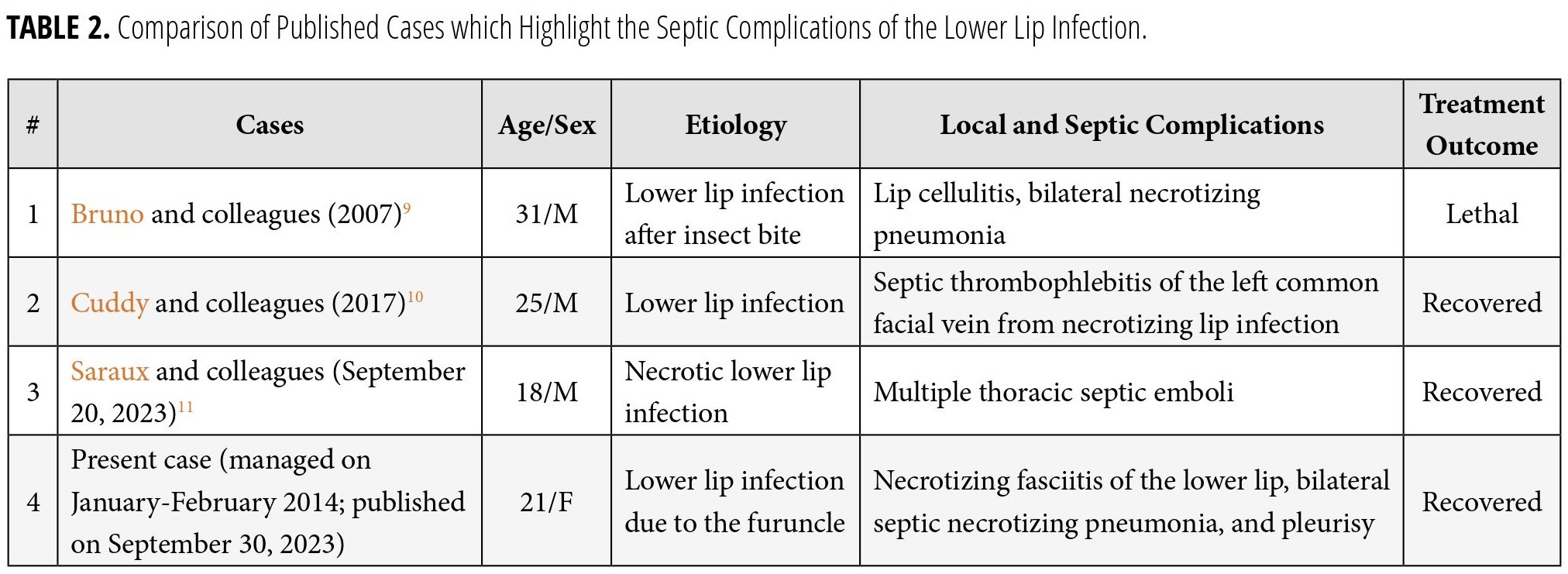
Infection of the lower lip can manifest differently. The likelihood of such prompt life- threatening septic complications, as thrombophlebitis, pneumonia, pleurisy, etc, may be underestimated due to the small size of the local inflammation of the lip. We present a 21-year-old Caucasian female with a Staphylococcus epidermidis infection of the lower lip (furuncle) complicated by lip abscess, suppurative cheilitis glandularis, lip necrosis, septic bilateral multilobar necrotizing (destructive) pneumonia, pleurisy (pleuritis), and pulmonary insufficiency of the first degree (type I). Clinical photos of the report demonstrate all stages of the course of inflammation and treatment of the severe lower lip infection from the moment of admission. Preoperative condition, the period of formation and demarcation of necrosis, cleaning of the wound from purulent content, demonstration of fibrinous exudate (also known as fibrinous plaques), the appearance of granulations, and visualization of lip scars as of the day of discharge from the hospital (day 26) are presented. The article also includes a chest X-ray at the time of admission, on the second day, and on the seventh day of hospital stay. The report is enriched as well by three-dimensional multi-slice computed tomography (3D MSCT) images on the eighth, eighteenth, and fortieth days from the moment of admission to our hospital. 3D MSCT of the lungs is showing the areas of pulmonary tissue necrosis and the healing phase. The article contains two videos (cine images) with a duration of 21 seconds and 2 minutes 11 seconds, which demonstrate chest MSCT on the hospital day 8 and 18. The patient was discharged on the 27th day of admission. According to our English-language literature search, it's a first ever reported case of the lower lip furuncle which led such a unique combination of severe local and septic complications documented at all stages of treatment from both aspects clinical and radiological. An update of the classification of uncomplicated and complicated forms of development of furuncles (i.e., boils) and carbuncles is done and presented. More than 37 literary sources were analyzed, and their key aspects complemented our report. Articles with necrotizing fasciitis of the lips were also analyzed.
KEY WORDS
Furuncle, boil, lower lip, lip necrosis, necrotizing fasciitis, suppurative cheilitis glandularis, necrotizing pneumonia, destructive pneumonia, pleurisy, pleuritis, chest X-ray, multi-slice computed tomography.
INTRODUCTION
Furuncles and carbuncles of the lips are an extremely dangerous inflammatory conditions.1 Furuncles also termed as boils.2,3 According to Tymofieiev (2020), coincidentally with a furuncle, acute purulent-necrotic inflammation of the hair follicle and surrounding connective tissue develops.4 A carbuncle is a diffuse purulent-necrotic inflammation of the skin and subcutaneous fatty tissue, emanating from several hair follicles and sebaceous glands.4 The carbuncle is also described as a cluster of furuncles.5 Consequently, the main difference between boils and carbuncles from odontogenic abscesses/phlegmons is the absence of odontogenic foci and the presence of purulent-necrotic rods.4
The danger of these two somewhat similar pathological conditions lies in extremely formidable general complications, like sinus thrombosis, meningitis, and septic conditions.1,6 Back in 1926, Wheeler summarized articles devoted to carbuncles and furuncles of the lips and their septic complications.7 Some articles highlight lower lip infection cases with local complications (simple/suppurative cheilitis glandularis,1 labio-facial necrotizing fasciitis,7 etc). But very limited number of English language papers present combination of local and general complications of the lower lip infection.8–10 And only one study (Bruno and colleagues, 2007) describes septic necrotizing pneumonia as a complication of the lower lip infection.8 In their study, the necrotizing pneumonia was a septic complication of the lower lip bite but not a furuncle or carbuncle. So, it’s a reason why we report a first to our knowledge presentation of lower lip abscessing furuncle complicated by suppurative cheilitis glandularis, lip necrosis, septic bilateral multilobar necrotizing pneumonia, and pleurisy. Our study is enhanced by a multi-slice computed tomography (MSCT) with three-dimensional reconstruction at different stages of necrotizing pneumonia treatment which was done in case of lower lip infection for the first time in the English-language literature.
CASE
A 21-year-old Caucasian female was referred to the Center of Maxillofacial Surgery with complaints for a severe lower lip swelling, change of its color, pain, inability to eat, and fever. On the day of the visit to the hospital, the patient did not notice any other complaints. According to the patient, the large swelling of the lip began when she tried to squeeze out the furuncle located in the red border of the lower lip.
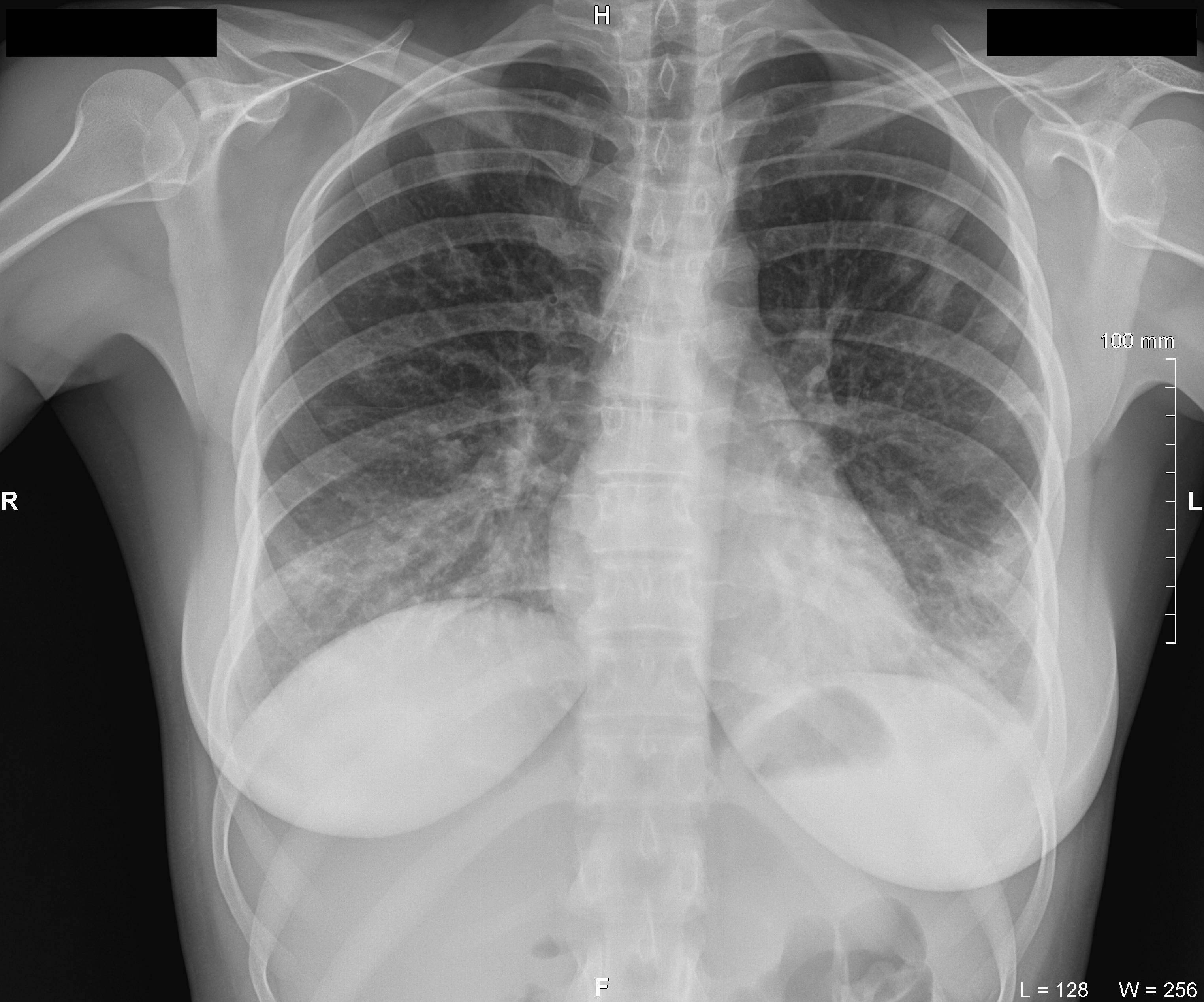
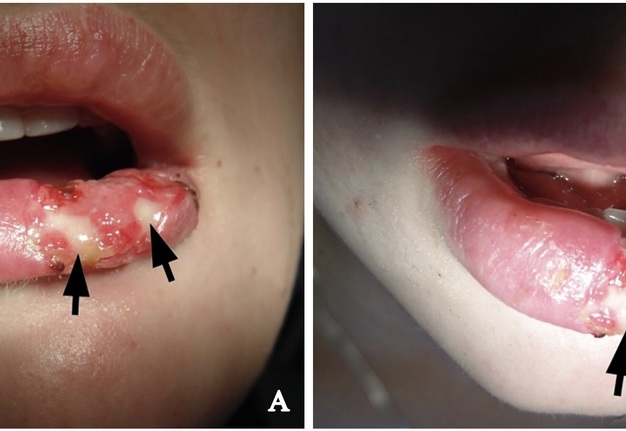
Clinical examination revealed significant lower lip swelling and the bluishness of the one third of lip mucosa, which resembled the formation of limited necrosis (Fig 1). The lower vermillion body (also known as lower lip vermillion) closer to the area of necrosis was covered with densely fixed red-yellow crusts. Palpation of the lower lip was very painful and opening of the mouth was slightly limited. Chest X-ray (Fig 2) was performed according to the treatment protocol. The diagnosis of the abscessing furuncle of lower lip complicated by suppurative cheilitis glandularis and necrosis of the lip mucosa was established. Drainage of the purulent locus in the lower lip was done under the local potentiated anesthesia (2.0 mL of Dexalgin® inject [Laboratorios Menarini S.A., Barcelona, Spain] intramuscularly 45 minutes before surgery and 3.0 mL of 4% Ultracaine® D-S forte [Aventis Pharma Deutschland GmbH, Frankfurt, Germany] intraorally for the nerves block. During the surgical treatment of the focus of infection of the lower lip, a clinical picture more usual for the lower lip carbuncles was noted1. From the lingual side of the lower lip under its mucous membrane, the presence of prolapsing numerous anatomically limited areas of suppuration corresponding to the localization and size of the small salivary glands was noted. This clinical/intraoperative picture corresponded to secondary suppurative cheilitis glandularis (also known as purulent cheilitis1). A smear was taken from the wound during the surgery to determine the type of bacterial pathogens and sensitivity to antibiotics. Drug therapy was started immediately upon admission in the form of intramuscular injections of ceftriaxone (1.0 g two times daily), intravenous metrogyl (100 mL two times daily) and detoxification therapy.
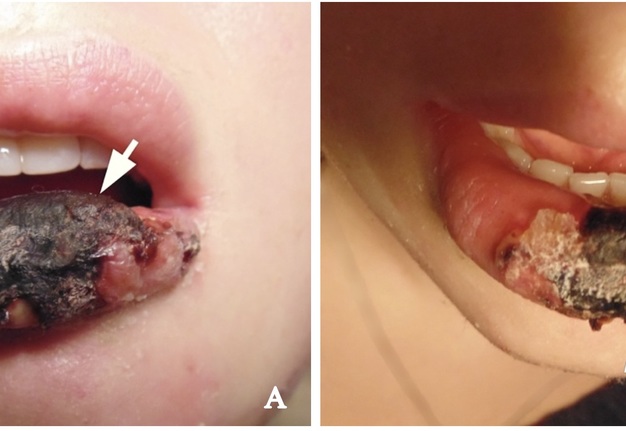
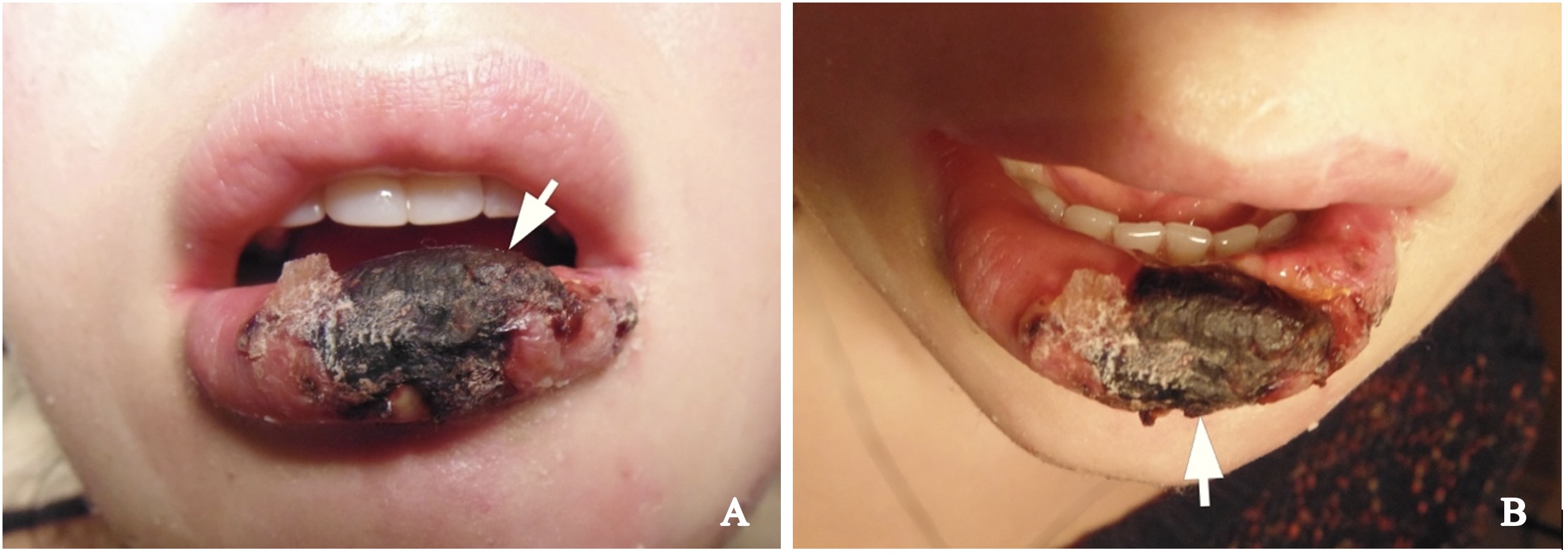
FIGURE 1. Hospital day 1. The pretreatment view of lower lip abscessing furuncle complicated by suppurative cheilitis glandularis and necrotizing fasciitis. Formation of the necrotic tissue is indicated by arrow. The lower vermillion body closer to the area of necrosis is covered with densely fixed red-yellow crusts. Printed with permission and copyrights retained by I.I.F.
On the second day after hospitalization and surgical treatment of the infectious process of the lower lip, despite improvement of the local status and cleaning of the wound from purulent exudate, the attending physician (I.I.F) noticed a slight cough in the patient. Chest X-ray (Fig 3) revealed radiological signs of the pneumonia and after the consultation of the pulmonologist (V.M.M.) the diagnosis of septic bilateral multilobar pneumonia was established and correction of treatment was performed. Figure 4 demonstrates condition of the lower lip on day 4 of the treatment. Lip swelling is decreased. Notes the formation and demarcation of the area of necrosis.
FIGURE 3. Antero-posterior view of the chest X-ray at day 2 of the treatment of lower lip furuncle complicated by necrotizing fasciitis of the lip. Radiological data corresponds to the bilateral multilobar pneumonia. H, head; R, right; L, left. Printed with permission and copyrights retained by I.I.F.
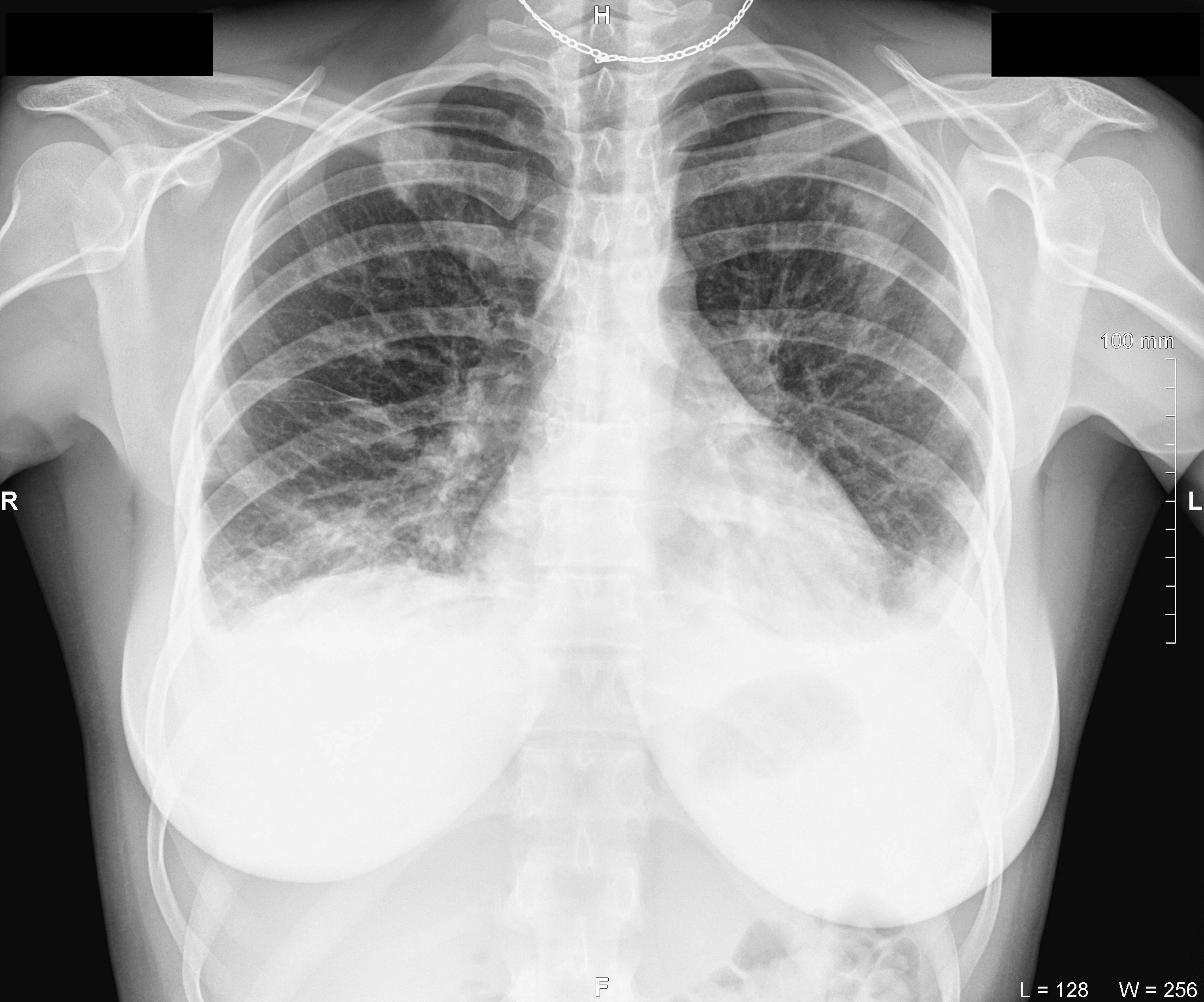
Chest X-ray (Fig 5) on hospital day 7 showed the radiological signs of the bilateral multilobar pneumonia and pleurisy (pleuritis) and the dynamic of the process.
Microbiological examination of a purulent wound showed the presence of Staphylococcus epidermidis (S. epidermidis) sensitive to Augmentin, Lincomycin, Oxacillin, Moxifloxacin, Vancomycin, and Candida spp. sensitive to Fluconazole and Ketoconazole.
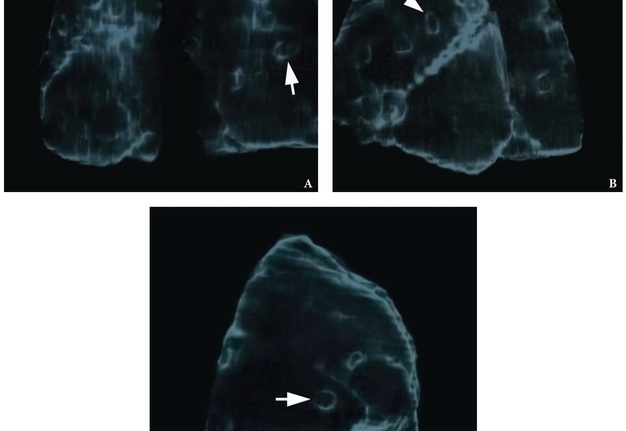
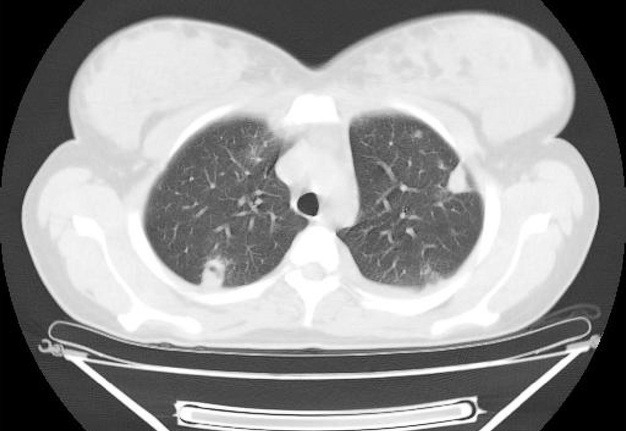
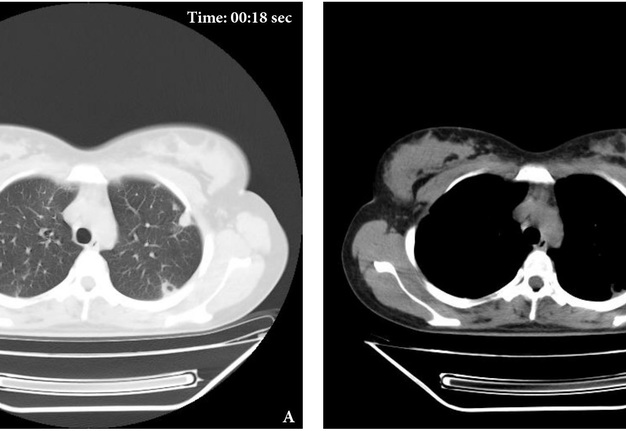
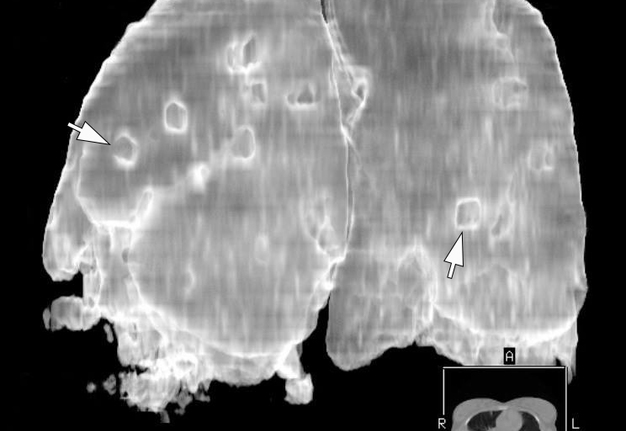
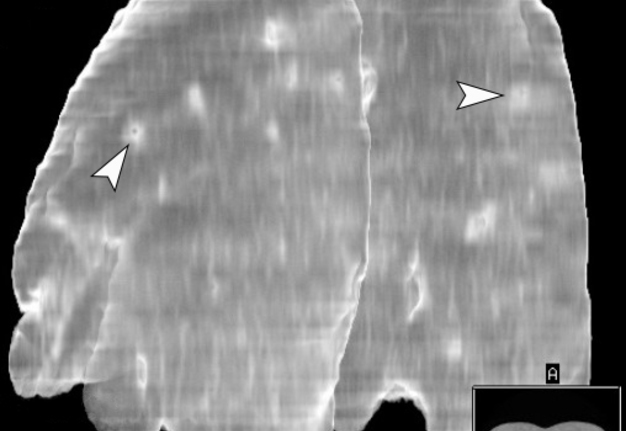
The MSCT (HiSpeed Dual, General Electric Company, Boston, Massachusetts, United States) of the lungs performed on hospital day 8 showed multiple areas of pulmonary tissue necrosis (Fig 6). Supplemental Video Content 1 demonstrates a sequence of MSCT images of the chest with bilateral necrotizing pneumonia and pleurisy. Video is available in the page of the full-text article on dtjournal.org and in the YouTube channel, available at https://youtu.be/R0RtPQm2mK8.
FIGURE 6. A 3D MSCT images (A, posterior view; B, latero-posterior view; C, lateral view) of the lungs. Day 8 of treatment of the severe lower lip infection complicated by lip necrosis, septic bilateral necrotizing pneumonia, and pleurisy (pleuritis). Multiple areas of pulmonary tissue defects are indicated by arrows. Printed with permission and copyrights retained by I.I.F.
VIDEO 1. Supplemental Video Content 1 demonstrates a sequence of non-contrast axial MSCT images (in lung and in chest windows) and reformatted coronal and sagittal images of the chest (in lung and in chest windows). Magnification 1.3x. The MSCT shows the state of the lungs at day 8 of treatment of the severe lower lip infection complicated by lip necrosis, septic bilateral multilobar necrotizing pneumonia, and pleurisy. This axial MSCT image in lung window corresponds to the 21st second of the video. Video is available in the page of the full-text article on www.dtjournal.org and in the YouTube channel ‘Videos of JDTOMP,’ available at https://youtu.be/R0RtPQm2mK8. Total video’s duration: 3 min 08 sec. Video time of the image: 0 min 21 sec.
Based on clinical and radiological data the diagnosis was adjusted to the following – a lower lip infection (abscessing furuncle) complicated by suppurative cheilitis glandularis, lip necrosis, septic bilateral multilobar necrotizing pneumonia, pleurisy (pleuritis), and pulmonary insufficiency of the first degree (type I).
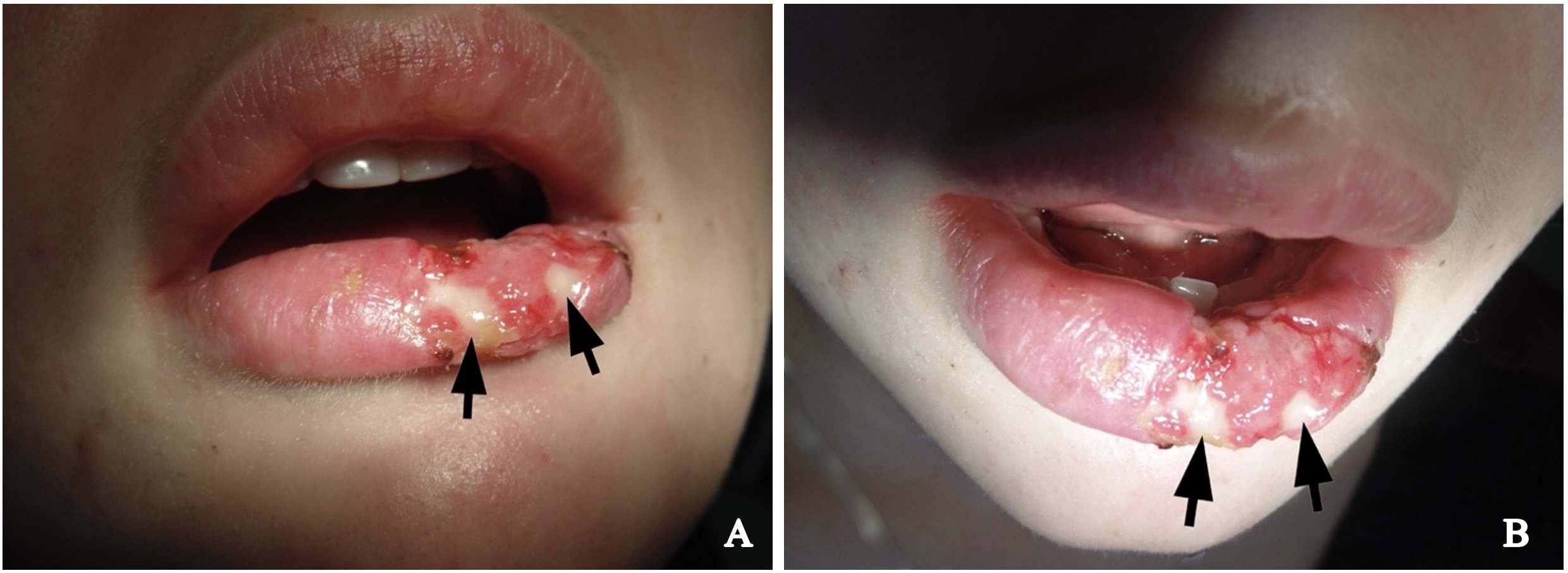
Daily dressing with liniment (Oflocain-Darnitsa®, tube 15 g, Kyiv, Ukraine) and debridement (minimally invasive necrectomy [also known as necrosectomy]) were performed upon the treatment of the lip infection. Figure 7 shows anterior and superior lip views after removal of necrotic tissue on hospital day 11. Noted a presence of fibrinous exudate (also known as fibrinous plaques).
Figure 8 shows anterior lip view on day 17 of the treatment. An appearance of the granulation tissue was noted.
Microbiological examination of the blood showed no growth of microflora.
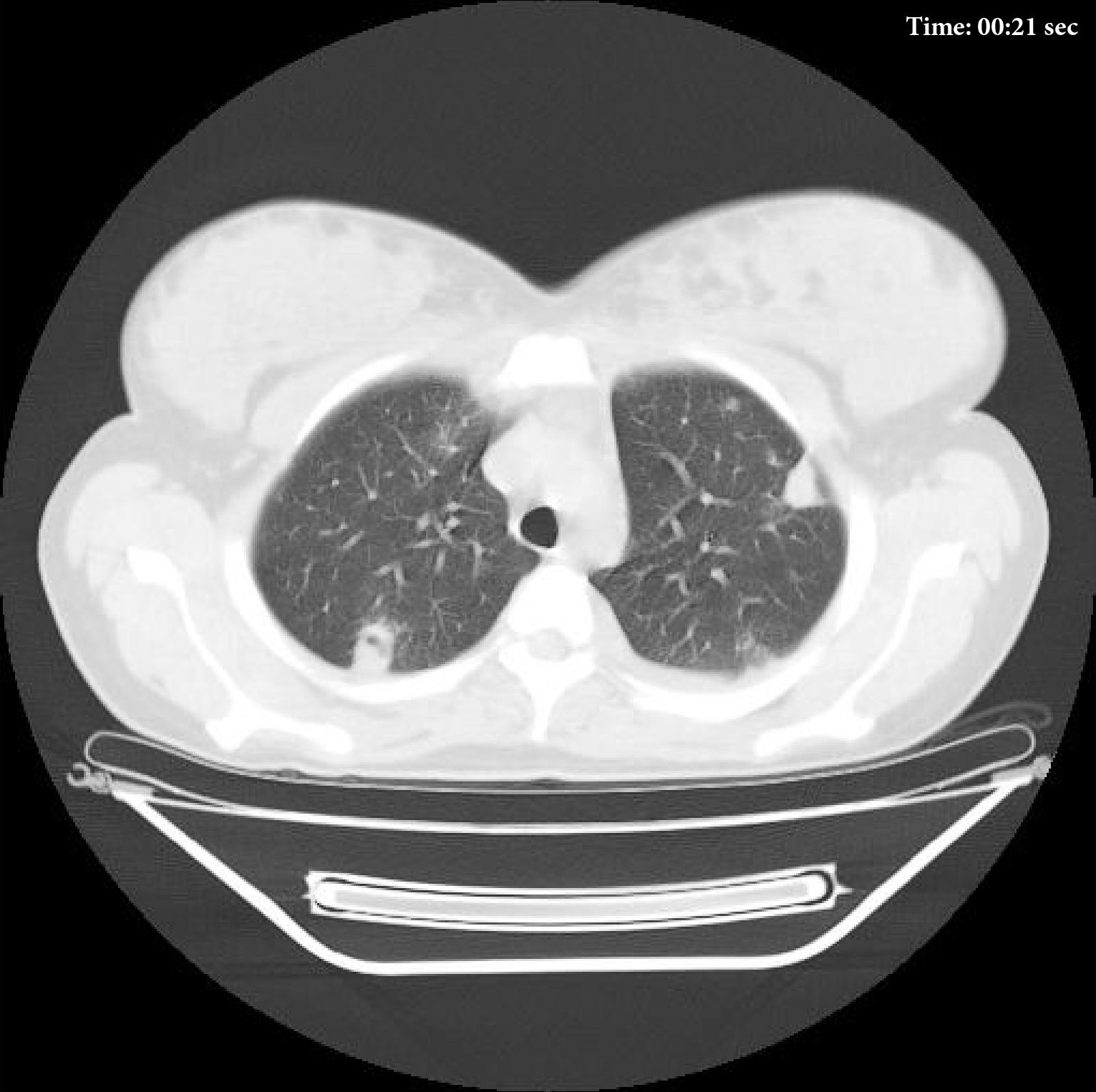
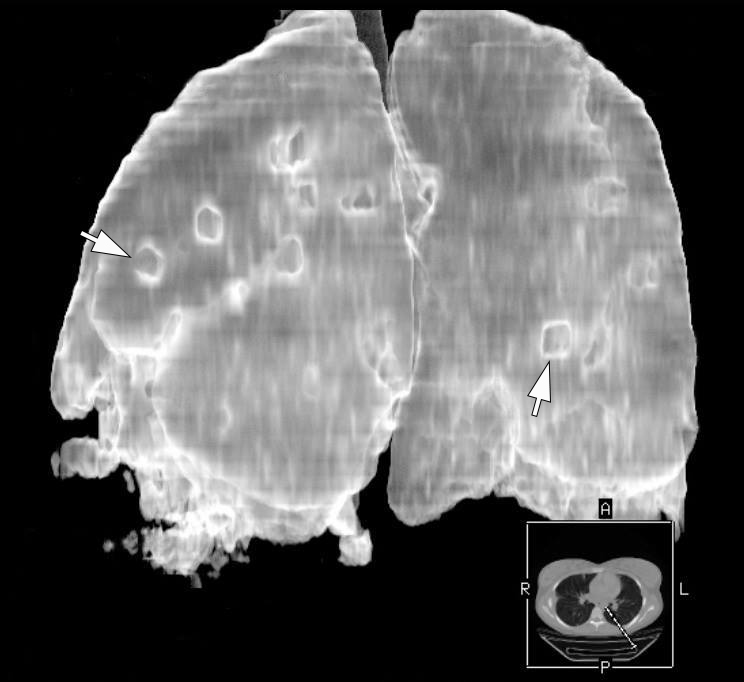
Supplemental Video Content 2 demonstrates MSCT images at day 18 of treatment of the severe lower lip infection complicated by lip necrosis, septic bilateral necrotizing pneumonia, and pleurisy. A decrease in the number of infiltrates and the amount of fluid is noted. The dynamics is weakly positive. Video is available in the page of the full-text article on dtjournal.org and in the YouTube channel, available at https://youtu.be/k7OEuPlUUJ8.
VIDEO 2. Day 18 of treatment of the severe lower lip infection complicated by lip necrosis, septic bilateral necrotizing pneumonia, and pleurisy (pleuritis). Notes presence of the cavitary lesions. A decrease in the number of infiltrates and the amount of fluid is noted. The dynamics is weakly positive. Supplemental Video Content 2 demonstrates a sequence of non-contrast axial MSCT images (in lung and in mediastinal [chest] windows) and 3-dimensional MSCT images of the lungs. A, axial MSCT scan in lung window; B, axial MSCT scan in mediastinal window. Magnification 1.3x. Video is available in the page of the full-text article on www.dtjournal.org and in the YouTube channel ‘Videos of JDTOMP,’ available at https://youtu.be/k7OEuPlUUJ8. Total video’s duration: 2 min 11 sec. Video time of the images: 0 min 18 sec (A) and 1 min 42 sec (B).
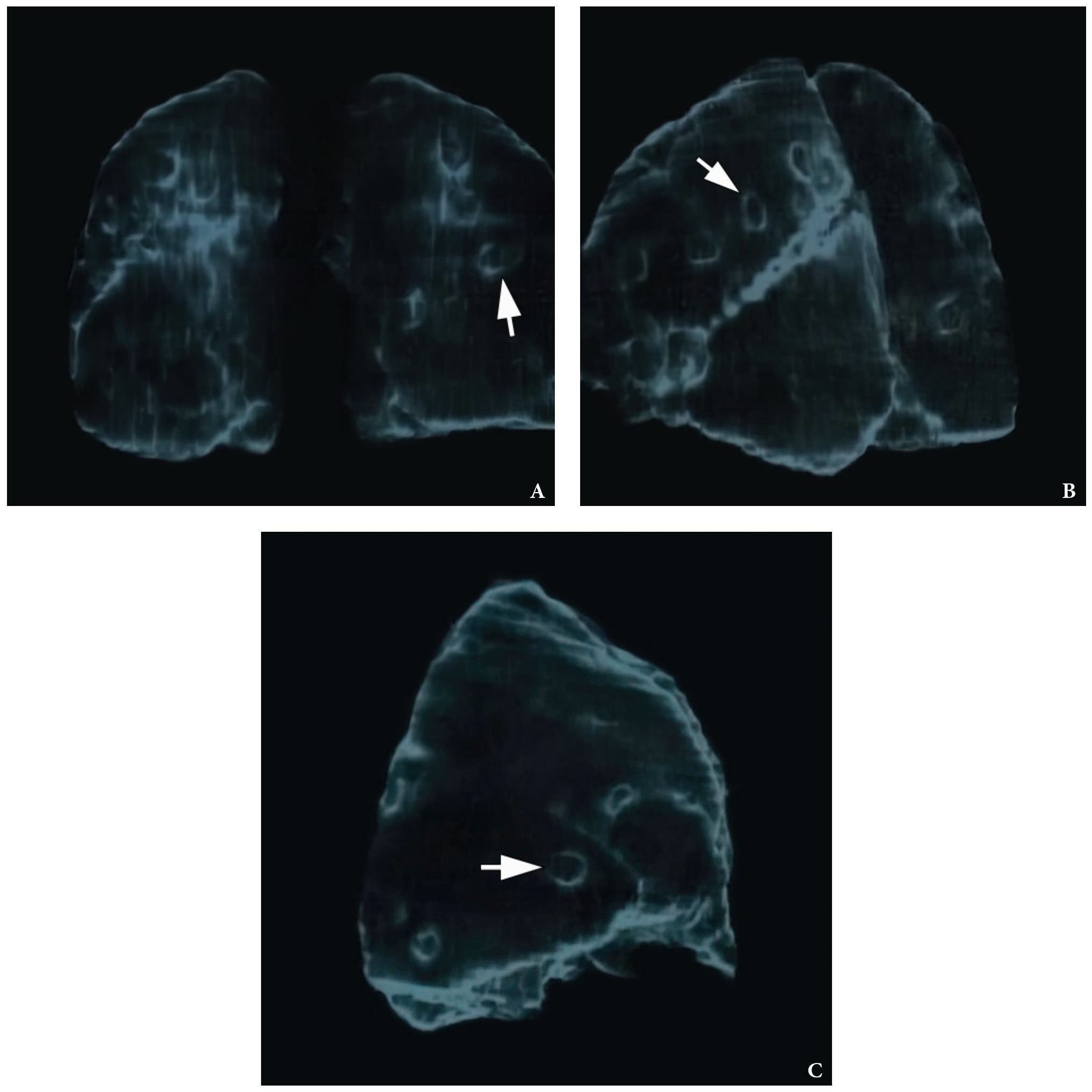
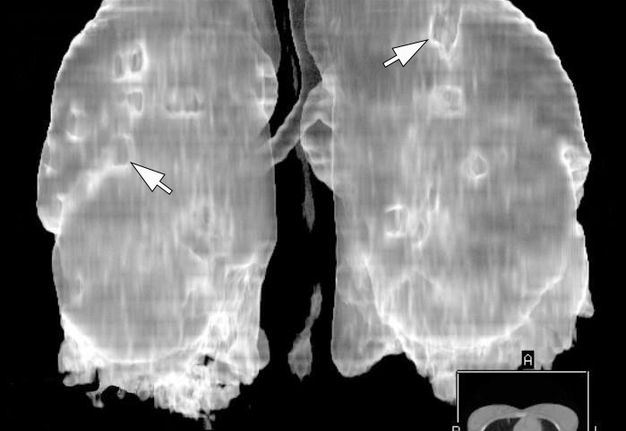
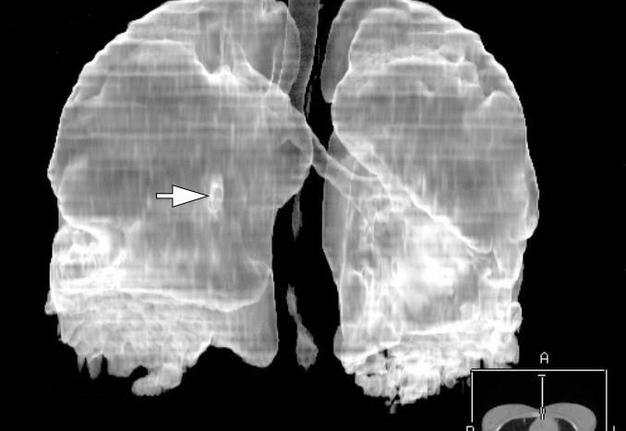
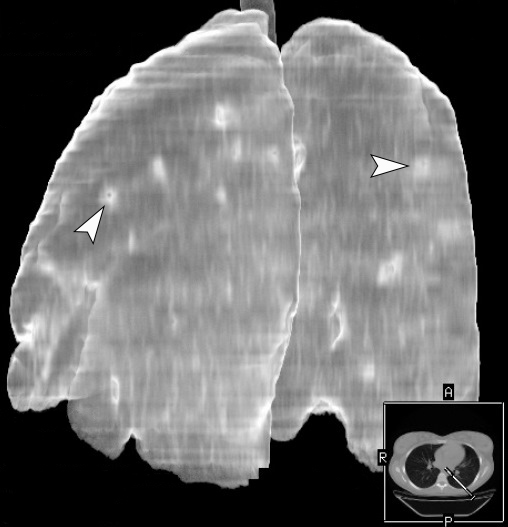
Figure 9 demonstrates three-dimensional MSCT images of the lungs at day 18 of treatment of the severe lower lip infection complicated by lip necrosis, septic bilateral necrotizing pneumonia, and pleuritis. Multiple areas of pulmonary tissue defects are indicated on the images.
FIGURE 9A. A three-dimensional multi-slice computed tomography images (A, posterior view; B, latero-posterior view; C, anterior view) of the lungs at day 18 of treatment of the severe lower lip infection. The infection process complicated by lip necrosis, septic bilateral necrotizing pneumonia, and pleurisy (pleuritis). Notes multiple areas of pulmonary tissue defects (arrows) due to septic bilateral necrotizing pneumonia. A, anterior; P, posterior; R; right; L, left. Magnification 1.1x. Printed with permission and copyrights retained by I.I.F.
FIGURE 9B. A three-dimensional multi-slice computed tomography images (A, posterior view; B, latero-posterior view; C, anterior view) of the lungs at day 18 of treatment of the severe lower lip infection. The infection process complicated by lip necrosis, septic bilateral necrotizing pneumonia, and pleurisy (pleuritis). Notes multiple areas of pulmonary tissue defects (arrows) due to septic bilateral necrotizing pneumonia. A, anterior; P, posterior; R; right; L, left. Magnification 1.1x. Printed with permission and copyrights retained by I.I.F.
FIGURE 9C. A three-dimensional multi-slice computed tomography images (A, posterior view; B, latero-posterior view; C, anterior view) of the lungs at day 18 of treatment of the severe lower lip infection. The infection process complicated by lip necrosis, septic bilateral necrotizing pneumonia, and pleurisy (pleuritis). Notes multiple areas of pulmonary tissue defects (arrows) due to septic bilateral necrotizing pneumonia. A, anterior; P, posterior; R; right; L, left. Magnification 1.1x. Printed with permission and copyrights retained by I.I.F.
Figure 10 shows anterior view of the lips on day 26 after the initiated treatment in hospital. Visualized is a complete healing of the lower lip and its scarring. The patient was discharged with a significant improvement in her local and general condition. The medical treatment carried out in the hospital included: ceftriaxone, levofloxacin, metrogyl, amicil, meropenem, avelox, karsil, yogurt (capsules), fluconazole, naclofen, omez, dexalgin, acelysin, reosorbilact, and lasolvan. The patient was discharged on the 27th day of admission.
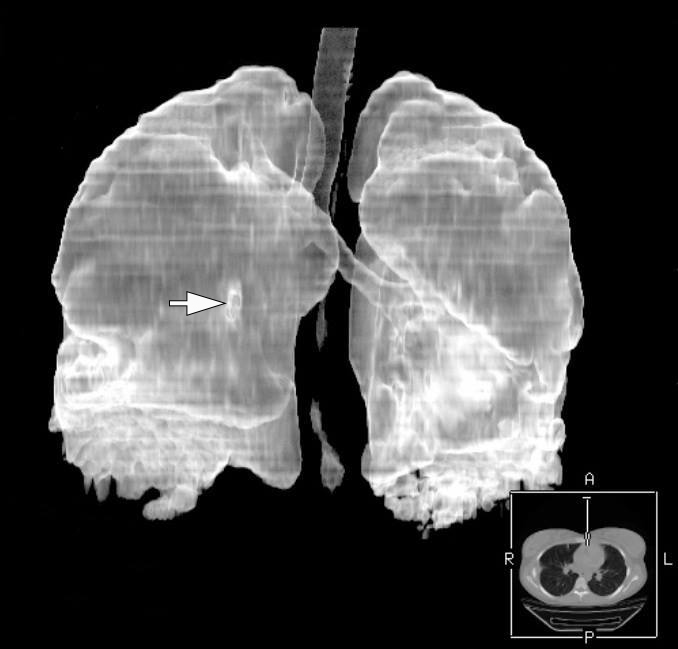
Figure 11 highlights a follow-up 3D MSCT image of the lungs at day 40 after the treatment of the severe lower lip infection complicated by septic bilateral necrotizing pneumonia and pleurisy was initiated. Noted a healing of the areas of pulmonary tissue defects.
FIGURE 11. A follow-up three-dimensional MSCT image (latero-posterior view) of the lungs at day 40 after thetreatment of the severe lower lip infection complicated by septic bilateral necrotizing pneumonia and pleurisy was initiated. Notes healing (arrowheads) of the multiple areas of pulmonary tissue defects. A, anterior; P, posterior; R, right.Magnification 1.1x. Printed with permission and copyrights retained by I.I.F.
According to analysis of sputum no acid-resistant rods (Mycobacterium tuberculosis) were detected.
DISCUSSION
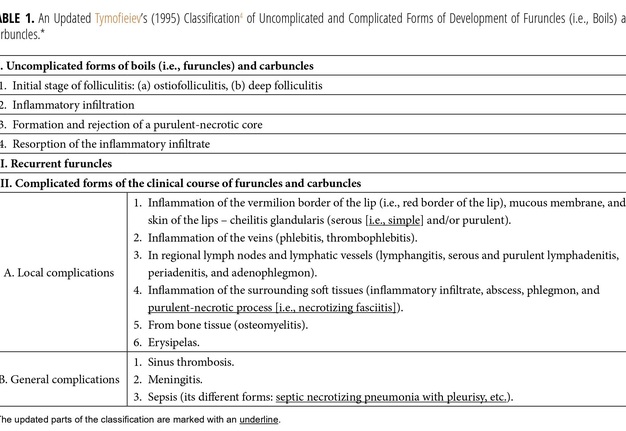
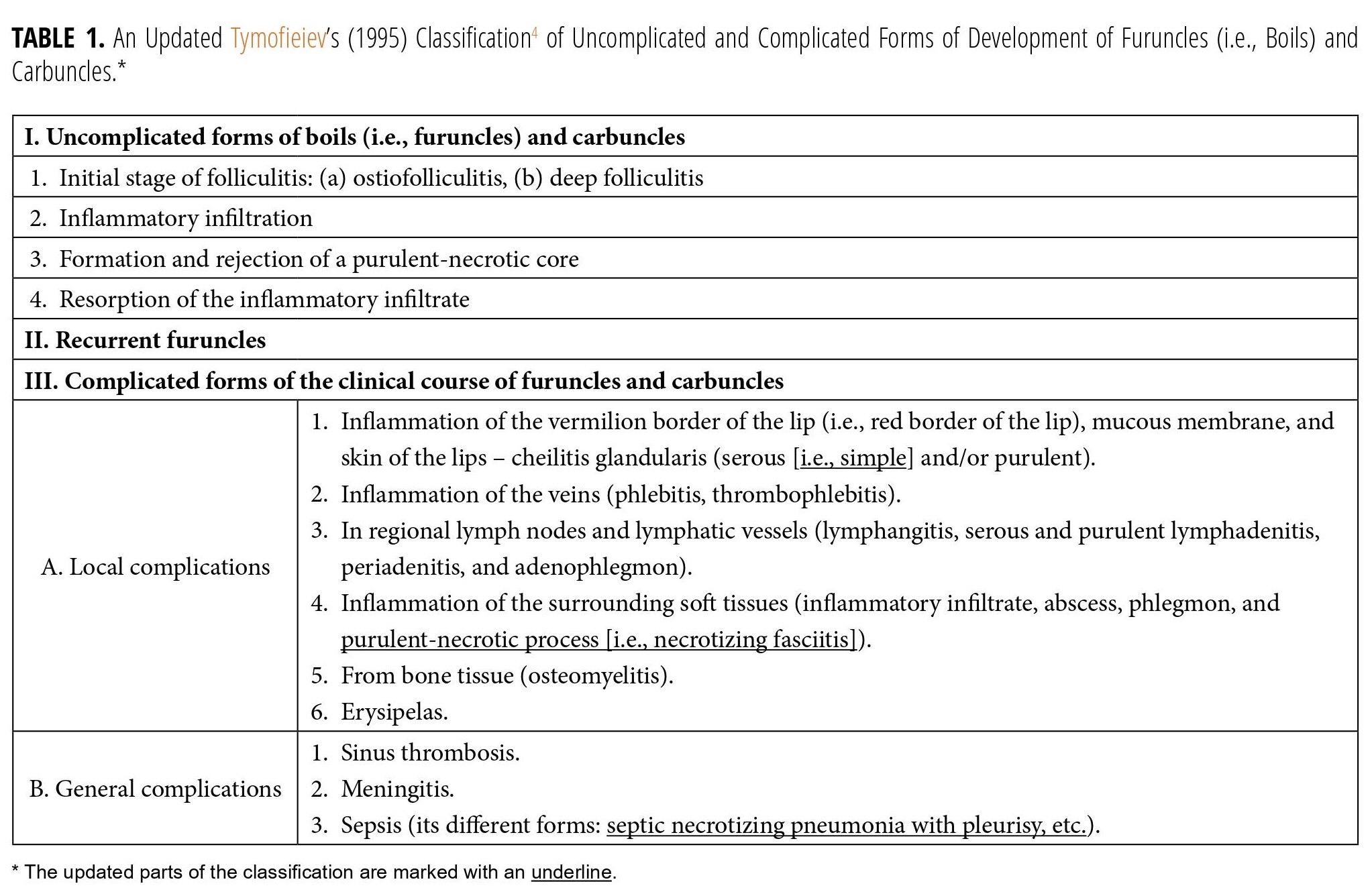
Management of lip infection and its complications is an important part of practice and current literature.12–16 For a better understanding, the systematization and possible complications of furuncles and carbuncles of different localizations (including lower lip) are presented in the classification (Table 1) developed by Tymofieiev (2012, 2020).1,4 The classification is updated by purulent-necrotic process (i.e., necrotizing fasciitis) and septic pneumonia with pleurisy presented in this report.
One of the typical forms of furuncles on the face is an abscessing furuncle without a necrotic zone.17 In this case, the patient came to us with an infection of the lip in the form of an abscessing furuncle with the formation of necrosis of the lip and suppurative cheilitis glandularis. Necrosis of the lip looked very similar to the manifestation of such a purulent-necrotic process, which is described in the English-language literature as necrotizing fasciitis.18,19 Necrotic tissues in case of Klebsiella pneumoniae necrotizing fasciitis on the upper lip (Kim and colleagues, 2020) looked like the necrotic surface of S. epidermidis infection of the lip in our case.18 In their case, necrosis developed due to the bullous lesion in a patient with diabetes.18 Even more important is that necrosis of the upper lip also led to a septic complication—embolus in the upper right lobe of the lungs.18 It is of interest that the infection condition of the lower lip in the case presented by Eltayeb and colleagues (2016) was very similar to inflammatory lip condition in the case by our team.8 They reported necrotizing fasciitis of the lower lip following lip infection (acne of the mental region).8 The authors reported lip condition in patient as labio-fascial necrotizing fasciitis.8
Usefulness of ultrasonographic examination of the lips upon lip infection was proved in the study of Tekcan Şanlı and Boyacı (2021).19 The possibilities of MSCT in lip infection cases are presented in the study of Amin and colleagues (2021).12
We bring to your attention possible variants of manifestations of necrosis of the lower lip of various etiologies. Lower lip necrosis was reported by Lanteri and colleagues (2012) in the female patient after injections of dermal filler.20 In their case, the area of necrosis was deeper, but occupied a much smaller area of the mucous membrane of the lower lip compared to our case.20
Lower lip necrosis as a complication of a prone position in scoliosis surgery was described by Alsiddiky (2011).21 Another pressure necrosis of lower lip due to Guedel’s airway was showed in the study by Bhardwaj and Bhagat (2014).22
A deep necrosis of half of the lower lip following a recurrent varicella-zoster virus infection with concomitant herpes simplex-1 infection was highlighted by McCormick and colleagues in 2016.23
A different appearance, compared to our case, had necrosis of the left lower hemilabium afterdental procedure under local anesthesia (Cervilla Martín and colleagues, 2022).24
The presence of signs of suppurative cheilitis glandularis in the patient at the time of hospitalization is one of the described local complications of the furuncles and carbuncles.1 If minor salivary glands of the lip are infected, the disease may manifest as numerous purulent cystic lesions (Musa and colleagues, 2005).25
Three types of cheilitis glandularis (i.e., simple, superficial suppurative, and deep suppurative) are considered different stages belonging to the clinical spectrum of progression characteristics of cheilitis glandularis.25,26 Paravina (2013) did an excellent analysis of the three subtypes/stages of cheilitis glandularis.27 Simple subtype of cheilitis glandularis is termed as simplex.27
Based on our English-language literature review of septic complications of lower lip infection (Table 2), we found only one literature case that described necrotizing pneumonia as a septic complication of lower lip infection. Bruno and colleagues (2007) reported lower lip infection after insect bite complicated with lip cellulitis and septic bilateral necrotizing pneumonia.9
Nicolaou and Bartlett (2017) emphasized, that necrotizing pneumonia refers to the development of necrosis, liquefication, and cavitation of the lung parenchyma from an infectious pathogen.28 Necrotizing pneumonia is also known as cavitary pneumonia or cavitary necrosis.29,30 According to Krishnadasan and colleagues (2000),31 necrotizing pneumonia (synonym: destructive pneumonia [Lossev and colleagues, 2017])32 is a pulmonary inflammation with consolidation and peripheral necrosis. Necrosis is usually representing as multiple small cavities, less than 10 mm in size.31 Complications of necrotizing pneumonia can be lung abscess and gangrene.33,34
Understanding computed tomography data in necrotizing pneumonia is important not only for radiologists, but also for surgeons. Nicolaou and Bartlett (2017) highlighted axial MSCT scans demonstrating cavitary lesions upon necrotizing pneumonia.28 MSCT analysis of the patient with bilateral necrotizing pneumonia, pleural and pericardial effusion is presented in the study by Pascualand colleagues (2010).35 Chatha and colleagues (2014) demonstrated both MSCT data of necrotizing pneumonia and pulmonary gangrene.33 Buwalda and Speelberg (1995) presented MSCT features of septic necrotizing pneumonia in patient with furuncle of the thigh.33
Analyzing the bacterial agent that was cultured from the wound of the lower lip, namely S. epidermidis, and data from the literature that confirm the possibility of septic complications with coagulase-negative staphylococci (Otto, 2017),36 we confirm the literature data that not only Staphylococcus aureus1,4 can cause similar infectious processes. S. epidermidis can cause even a septic shock, mostly in immunocompromised intensive-care unit patients.37
Our case well describes and demonstrates the descending path of septic complications when the infection is localized within the lower lip.
CONCLUSIONS
This clinical case confirms the formidable septic complications of a lower lip infection caused by Staphylococcus epidermidis. Treatment of furuncles of the lips requires urgent treatment by professionals with mandatory monitoring of the functions of internal organs and systems. Multi-slice computed tomography with three-dimensional reconstruction is the gold standard for the diagnosis of septic pulmonary complications at all stages of the treatment of complications of furuncles of the lower lip.
REFERENCES (37)
-
Tymofieiev OO. Manual of maxillofacial and dental surgery (Russian). 5th ed. Kyiv: Chervona Ruta-Turs; 2012:319–32.
-
Pratt GH. Furuncle of upper lip. Am J Surg 1937;36(1):118–21. https://doi.org/10.1016/S0002-9610(37)90799-2
-
Gordon D. Treatment of boils and carbuncles. Am J Surg 1937;36(1):107–17. https://doi.org/10.1016/S0002-9610(37)90798-0
-
Tymofieiev OO. Maxillofacial surgery and surgical dentistry (Russian). Volume 1. Kyiv: Medicine, All-Ukrainian Specialized Publishing House; 2020:563–88.
-
InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Boils and carbuncles: How are boils treated? 2018 Jun 14. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513136/
-
Stefański K. Czyrak czoła powikłany posocznicowym zapaleniem płuc. Furuncle of the forehead complicated by septic pneumonia (Polish). Czas Stomatol 1980;33(8):729–34.
-
Wheeler WIdC. The danger of sepsis about the lips. Ir J Med Sci 1926;1:369–371.https://doi.org/10.1007/BF02953980
-
Eltayeb AS, Ahmad AG, Elbeshir EI. A case of labio-facial necrotizing fasciitis complicating acne. BMC Res Notes 2016;9:232. https://doi.org/10.1186/s13104-016-2041-3
-
Bruno GJ, Bruno JM, Miyake AA. Community-acquired methicillin-resistant Staphylococcus aureus infection with fatal necrotizing pneumonia from lip abscess: a case report. J Oral Maxillofac Surg 2007;65(11):2350–3. https://doi.org/10.1016/j.joms.2006.09.020
-
Cuddy K, Saadat N, Khatib B, Patel A. Necrotizing lip infection causing septic thrombophlebitis of the neck: a rare variant of Lemierre syndrome. J Oral Maxillofac Surg 2018;76(1):134–9. https://doi.org/10.1016/j.joms.2017.05.030
-
Saraux O, Fabre F, Milpied B, et al. Necrotic lip infection complicated by facial cellulitis and septic thoracic emboli in an 18-year-old man: a quiz. Acta Derm Venereol 2023;103:adv9605. https://doi.org/10.2340/actadv.v103.9605
-
Amin D, Satishchandran S, Drew S, Abramowicz S. Diagnosis and treatment of lip infections. J Oral Maxillofac Surg 2021;79(1):133–40. https://doi.org/10.1016/j.joms.2020.06.025
-
Huoh KC, Chang KW. Lip abscess associated with isotretinoin treatment of acne vulgaris. JAMA Dermatol2013;149(8):960–1. https://doi.org/10.1001/jamadermatol.2013.4066
-
Lucerna AR, Espinosa J, Darlington AM. Methicillin-resistant Staphylococcus aureus lip infection mimicking angioedema. J Emerg Med 2015;49(1):8–11. https://doi.org/10.1016/j.jemermed.2014.12.022
-
Tekcan Şanlı DE, Boyacı Z. Immunocompetent young patient presenting with unilateral lip abscess due to peeling exfoliated lip skin. Turk Arch Otorhinolaryngol 2021;59(3):239–41. https://doi.org/10.4274/tao.2021.2021-4-9
-
Godoy-Gijón E, del Pozo-de Dios JC, Román-Curto C. Bacterial lip abscess in an immunocompetent patient (Spanish). Dermatol Online J 2013;19(4):13. https://doi.org/10.5070/D33b01j1kn
-
Cherniak OS, Fesenko II. Periorbital abscessing furuncle. J Diagn Treat Oral Maxillofac Pathol 2021;5(1):13–4. https://doi.org/10.23999/j.dtomp.2021.1.4
-
Kim HS, Chang YJ, Chung CH. Klebsiella pneumoniae necrotizing fasciitis on the upper lip in a patient with uncontrolled diabetes. Arch Craniofac Surg 2020;21(2):127–31.
-
Choi MG. Necrotizing fasciitis of the head and neck: a case report. J Korean Assoc Oral Maxillofac Surg2015;41(2):90–6. https://doi.org/10.5125/jkaoms.2015.41.2.90
-
Lanteri A, Celestin R, Trovato M, Rauscher G. Lower lip necrosis. Eplasty 2012;12:ic4.
-
Alsiddiky A. Lip necrosis as a complication of a prone position in scoliosis surgery. Sultan Qaboos Univ Med J2011;11(2):273–5.
-
Bhardwaj A, Bhagat H. Necrosis of lower lip due to Guedel's airway in a case of head injury. J Neuroanaesth Crit Care 2014;1(3):219.
-
McCormick AP, Kanas RJ, Orton M, Rice T. Unusual necrosis of the lower lip following a varicella zoster recurrence. Int J Oral Dent Health 2016;2:026.
-
Cervilla Martín MT, Romero Marchante M, Sanz Trenado R, García Jimenez M. Left lower hemilabium necrosis as a complication of infiltration under local anesthesia. Acta Otorrinolaringol Esp (Engl Ed) 2022;73(5):336–8.https://doi.org/10.1016/j.otoeng.2022.02.006
-
Musa NJ, Suresh L, Hatton M, et al. Multiple suppurative cystic lesions of the lips and buccal mucosa: a case of suppurative stomatitis glandularis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99(2):175–9. https://doi.org/10.1016/j.tripleo.2004.02.070
-
Friedrich RE, Löning T. Cheilitis glandularis: case report with respect to immunohistochemical findings. GMS Interdiscip Plast Reconstr Surg DGPW 2016;5:Doc04. https://doi.org/10.3205%2Fiprs000083
-
Paravina M. Cheilitis glandularis apostematosa in a female patient – a case report. Serb J Dermatol and Venereol2014;5(4):177–82. https://doi.org/10.2478/sjdv-2013-0015
-
Nicolaou EV, Bartlett AH. Necrotizing pneumonia. Pediatr Ann 2017;46(2):e65–e68. https://doi.org/10.3928/19382359-20170120-02
-
Lumunsad KFL, Tan-Reyes MA. Cavitary pneumonia in an otherwise immunocompetent host [who underwent nutritional changes]: a case report. Respirology 2019;24:132–3. https://doi.org/10.1111/resp.13700_114
-
Hodina M, Hanquinet S, Cotting J, et al. Imaging of cavitary necrosis in complicated childhood pneumonia. Eur Radiol 2002;12:391–6. https://doi.org/10.1007/s003300101008
-
Krishnadasan B, Sherbin VL, Vallières E, Karmy-Jones R. Surgical management of lung gangrene. Can Respir J2000;7(5):401–4. https://doi.org/10.1155/2000/174703.
-
Lossev A, Dilanyan, I. Samofalov D, et al. Destructive pneumonia in newborns with surgical diseases. Neonatol Surg Perinatal Med 2017;7(4):55–60. https://doi.org/10.24061/2413-4260.VII.4.26.2017.10
-
Chatha N, Fortin D, Bosma KJ. Management of necrotizing pneumonia and pulmonary gangrene: a case series and review of the literature. Can Respir J 2014;21(4):239–45. https://doi.org/10.1155/2014/864159
-
Buwalda M, Speelberg B. Metastatic staphylococcal lung abscess due to a cutaneous furuncle. Neth J Med1995;47(6):291–95. https://doi.org/10.1016/0300-2977(95)00042-9
-
Pascual A, Perez MH, Jaton K, et al. Mycoplasma hominis necrotizing pleuropneumonia in a previously healthy adolescent. BMC Infect Dis 2010;10:335. https://doi.org/10.1186%2F1471-2334-10-335
-
Otto M. Staphylococcus epidermidis: a major player in bacterial sepsis? Future Microbiol 2017;12(12):1031–3. https://doi.org/10.2217%2Ffmb-2017-0143
-
Demiselle J, Meyer P, Lavigne T, et al. Staphylococcus epidermidis bloodstream infections are a cause of septic shock in intensive care unit patients. Int J Infect Dis 2023;135:45–8. https://doi.org/10.1016/j.ijid.2023.07.014