February 18, 2017
https://doi.org/10.23999/j.dtomp.2017.1.6
J Diagn Treat Oral Maxillofac Pathol 2017;1:41−53.
Under a Creative Commons license
HOW TO CITE THIS ARTICLE
Tymofieiev OO, Fesenko II, Tymofieiev OO. Condition of the teeth in fracture gap of the mandible. J Diagn Treat Oral Maxillofac Pathol 2017;1(1):41−53.
INSTITUTIONAL REPOSITORY
https://ir.kmu.edu.ua/handle/123456789/786
Contents: Abstract | Introduction | Materials and Methods | Results and Discussion | References (4)
ABSTRACT
Purpose: The aim of the present study was to determine condition of the teeth, which are located in the fracture gap of different parts of mandible and substantiate an indications for their removing or retaining.
Material and Methods: 114 patients with 186 fractures were involved in this research.
Results: 50% or more cases of post-traumatic inflammatory complications were observed in case of contact failure of the teeth roots, that are in a gap of fracture, with the periodontium of these teeth al 1/2 or more of their length. Saving teeth in fracture gap, which have failure of contact with the surrounding periodontium 1/2 and 3/4 the length of the root causes high risk of inflammatory complications in bone and surrounding soft tissues.
Conclusions: Based on the specified condition of teeth in the fracture gap different areas of the mandible justified indication for removal or preservation.
Introduction
In many textbooks on maxillofacial and oral surgery meet a different attitude to the tooth, which is located in the gap of the mandible fracture. Absolute indications for teeth removal from the fracture gap are: roots and fractured teeth or completely dislocated from the socket teeth; teeth periodontitis (with periapical chronic inflammatory lesions); teeth with symptoms of periodontitis or parodontosis of moderate and severe course; if exposed root is in the fracture gap or impacted tooth, thereby preventing tight (right) reposition of jaw fragments (tooth, wedged in the fracture gap); teeth, intractable to conservative treatment and support inflammatory manifestation [1, 2, 3]. In some cases, it proposed to remove the tooth, which can be further potential cause of post-traumatic osteomyelitis [4]. In other cases, we have to hold it, because the tooth can keep the broken-off fragment of the mandibular bone.
The purpose of the present study was to determine condition of the teeth, which are located in the fracture gap of different parts of mandibular bone and substantiate an indications for its removing and/or retaining.
Materials and Methods
We observed 114 patients with open fractures of the mandible, which were treated in the maxillofacial department №1 of the Kyiv City Clinical Hospital №12 (Center of Oral and Maxillofacial Surgery, Shupyk National Medical Academy of Postgraduate Education) and the Center of Maxillofacial Surgery of Kyiv Regional Clinical Hospital. This study examined only those victims who have a tooth from fracture line is not removed upon hospitalisation.
The observation period for patients was performed for one year after the injury. Age of victims was between 18 and 53 years. Of the 114 patients with mandibular fractures in 42 of examined (36.8%) were unilateral and in 72 patients (63.2%) – bilateral fractures. In 114 of victims were diagnosed 186 fractures. In all victims the damages of the mandible were obtained in household injuries. Seeking medical help, i.e. hospitalization of patients was 1-4 days after the injury.
During hospitalization all the victims were carried out X-ray examination, namely making radiographs of the jaws (in different projections), panoramic radiography and / or CT cans. Reduction and fixation of mandibular bone fragments was performed by bimaxillary arch bars with gearing loops and intermaxillary rubber traction. Teeth from the fractures gap upon hospitalization were not removed. Surgical treatment (osteosynthesis) was used in 14 victims (12.3%). After the reduction and fixation of bone fragments of jaws, in addition to hygiene oral care, all patients with mandibular fractures performed traditional medical treatment that included antibiotics, analgesics, hyposensitization drugs and physiotherapy.
Among the special methods of the examination, we have chosen periotestometry and pulp vitality test (electric pulp test) of the tooth in the fracture gap.
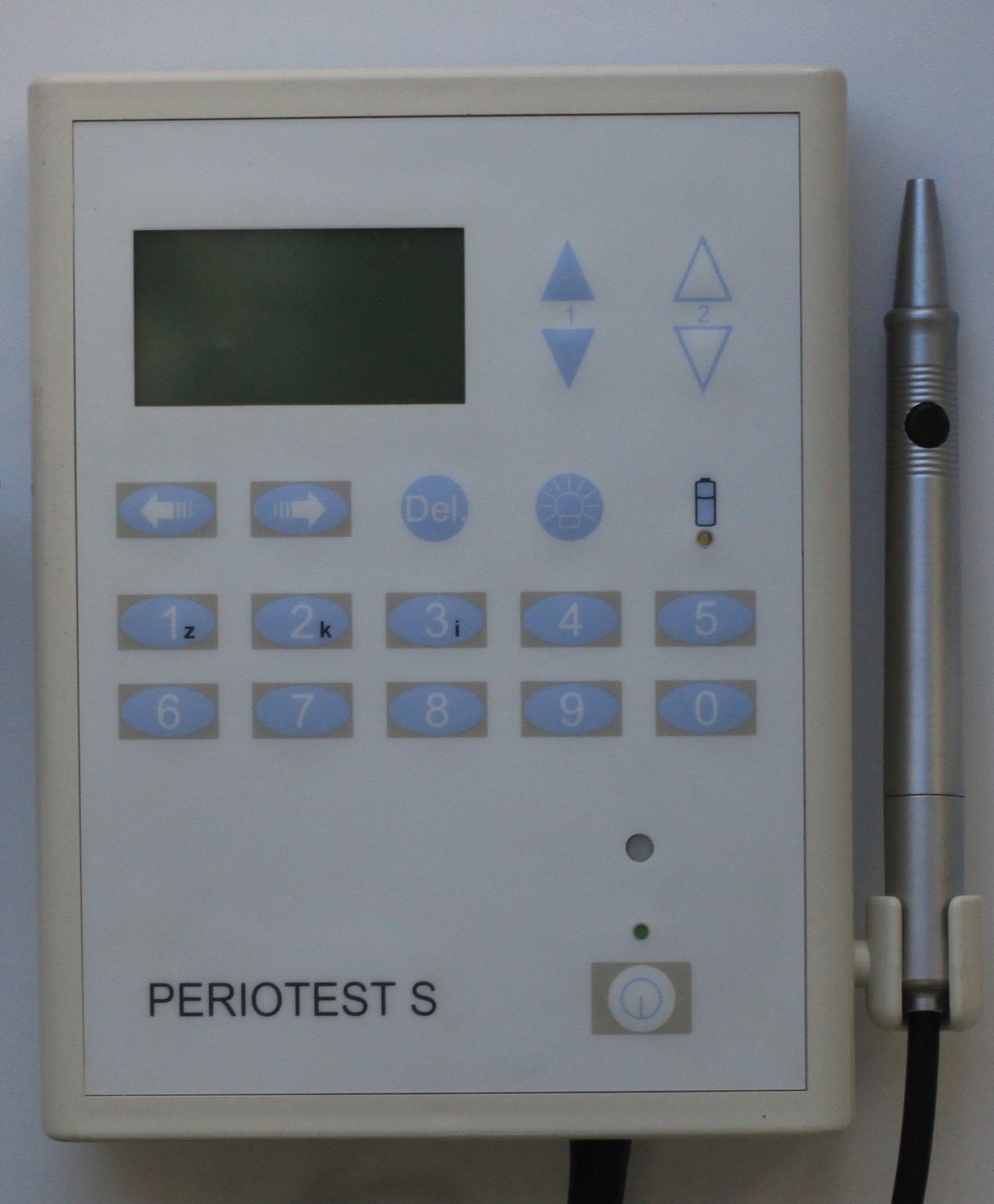
Periotestometry is a method of the indirect state estimation of the tooth attachment tissues, e.g. estimation of the functional ability of parodontium in the areas of interest, which is performed using Periotest S desktop unit. This appliance complies with the norms EN 60601 and EN 60601-1-2 and was awarded the CE mark in accordance with the guidance document 93/42/EWG for medical devices dated on June 14, 1993. The Periotest S (Fig 1) evaluates the ability of the parodontium tissues to reset the tooth after it was exposed to the certain external load. The appliance consists of the instrument box, computer analyser and handpiece which are intercommunicated with each other. Working element of a handpiece is a two-mode tine which includes the piezoelectric element. Its physical working principle is to convert an electric pulse to a mechanical pulse. The examined tooth or implant with the abutment is percussed with the tine of the handpiece at regular intervals (250 msec) applying the force which is non-invasive both for the hard dental tissues and the tissues of the parodontium.
During the measuring, the tip of a handpiece automatically taps on the tooth for 16 times, i.e. 4 times per second. To analyse the results, the arithmetic mean from 3 measurements performed with intervals from 10 to 15 seconds is used. When evaluating the function of individual parodontium, the teeth of the upper and lower jaws should not come in contact! During the measurement, the sleeve of handpiece should not touch any tooth. The distance between handpiece and tooth should be from 0.7 up to 2.0 mm. The specifics of using the periotestometry method in persons with mandibular fracture was the fact that it could be performed only if there was a solution of continuity of the mandibular bone in the area of incisors, canines, premolars, and the first molar. The examined tooth, i.e. the tooth in the fracture gap, was not fixed with an arch bar during periotestometry however it was fixed with a ligature wire after the procedure had been completed.
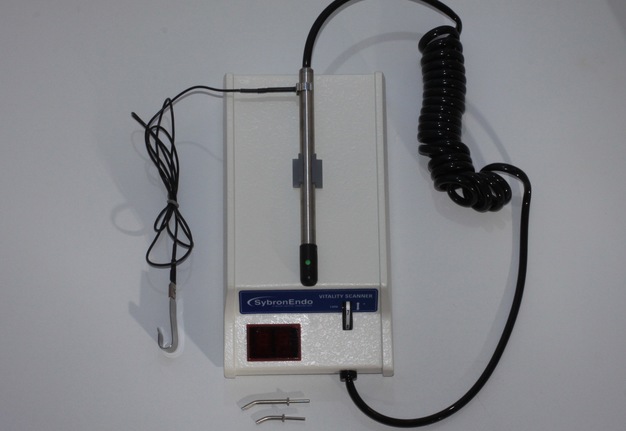
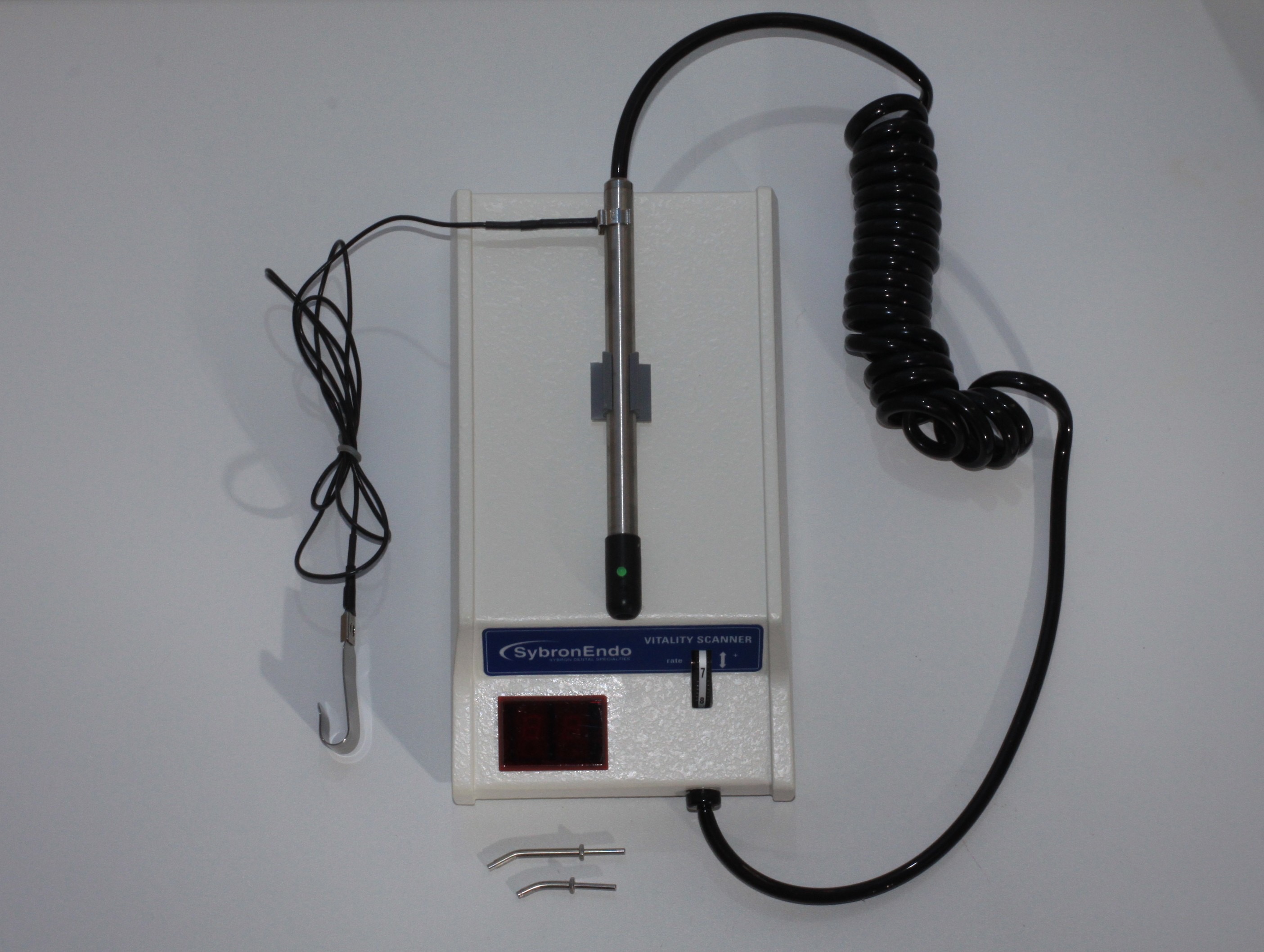
Vitality test of the tooth, i.e. the investigation of the pulp vitality, has been conducted with Vitality Scanner (Fig 2A). During manipulations in the oral cavity, we have used only a disposable wooden spatula along with the appliance (Fig 2B). When using Vitality Scanner, we have also used the following sequence of actions recommended in the manual:
- Before using the appliance, we have adjusted the deflection speed to its minimal value by turning the wheel "1" on the panel. We have also connected the earth wire of the spatula detector and inserted the handpiece into the front part of the sensitive element.
- The clip for lips was attached to the patient's lip (the patient could hold it with his/her hands).
- The test tooth was dried (according to the manual, we did not use chemicals (ether, alcohol) in order to prevent changes in the excitability threshold of the tooth pulp).
- The tip of the sensitive element was immersed into a small quantity of the fluoride gel and placed on the tooth while not touching the gingiva.
- Once a good electrical contact was achieved, the light on the sensitive element turned on. The sensitive element was kept in contact with the tooth until the patient felt the stimulation.
- The response level was indicated on the digital display.
- After waiting for two seconds, the next tooth was tested. The display was automatically rebooted to its home position once the tine contacted the tooth.
- After the test was completed, Vitality Scanner automatically turned off in 10-15 seconds.
According to the device manual provided by the manufacturer, the normal range of the pulp vitality response is 10-40 un., 20-50 un., and 30-70 un. for incisors, premolars, and molars, respectively. The values of Vitality Scanner exceeding these indices indicate any vitality decline of the pulp.
To control the indices of the conducted periotestometry and tooth vitality test in patients with unilateral open fractures of the mandibular bone, the teeth on the healthy side (the side opposite to the damage) have been used while in patients with bilateral open fractures the teeth of the upper jaw were used.
When carrying out this method of the patient’s examination, we have always taken into account the following parameters: localization of the fracture; the displacement degree of the mandibular bone fragments; correlation between the tooth located in the fracture gap and periodontium.
Depending on the displacement degree of the mandibular bone fragments, we have divided the patients with fractures of any localization into three groups: group 1 - the fractures without dislocation of the fragments (subperiosteal), i.e. the fracture gap was clearly visible in the X-ray images as a 'fine thread or the hairline'; group 2 – with minimal dislocation of the fragments (1 to 2 mm); group 3 – with remarkable dislocation of the fragments (more than 2 mm).
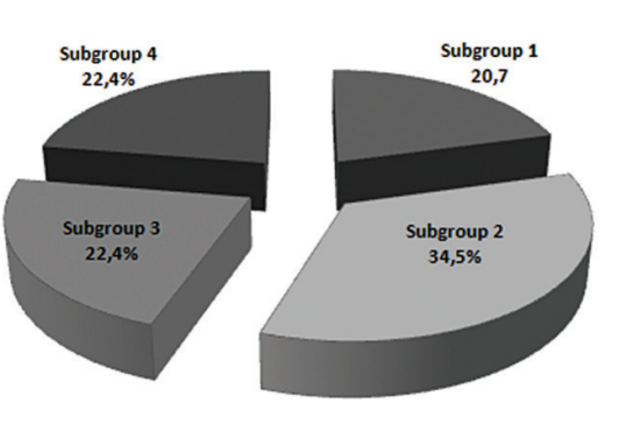
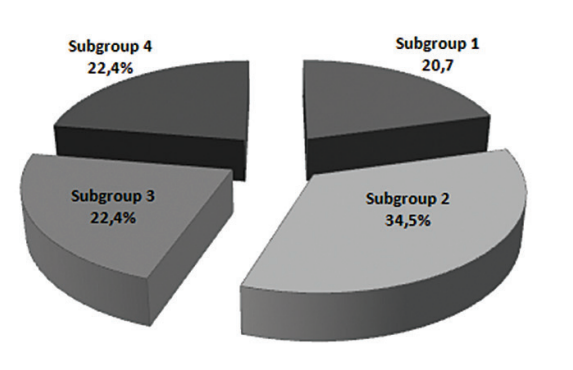
Depending on the contact area between the root of the tooth (located in fracture gap) and periodontium, we have also divided all the patients into 4 subgroups: subgroup 1 - the contact between the root of the tooth and periodontium is preserved along the whole length of the root; subgroup 2 - the contact between the root of the tooth and periodontium is disrupted along 1/3 of its length; \subgroup 3 - the contact with periodontium is disrupted along 1/2 of its length; subgroup 4 - contact with periodontium is disrupted along 3/4 of its length.
Digital data obtained from the laboratory examination has been processed using the standard variable-statistical approach and a PC with the statistical program SPSS 11.0 for Windows and Microsoft Excel 2000. The accuracy of the test results has been estimated using the Student’s t-test. Variations have been considered significant when р < 0.05.
Results and Discussion
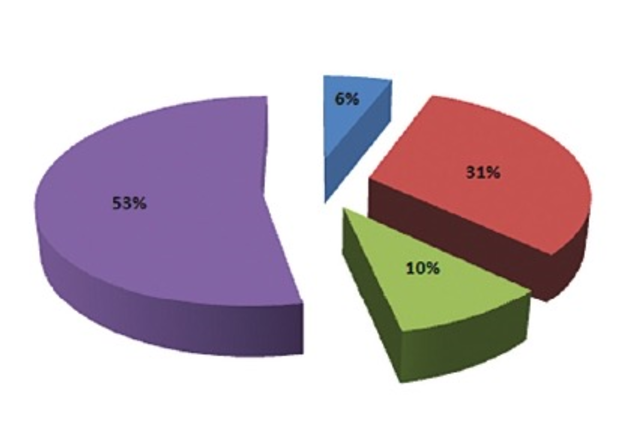
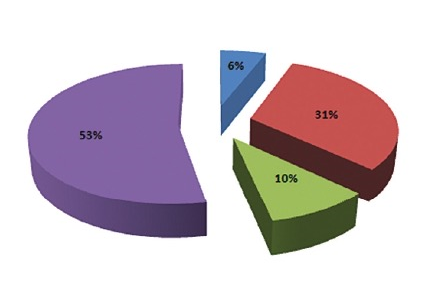
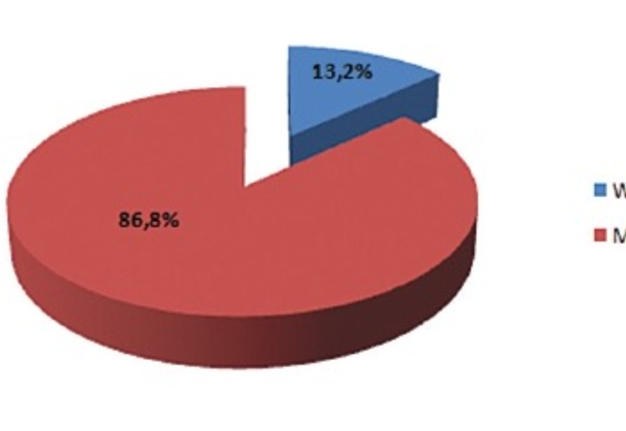
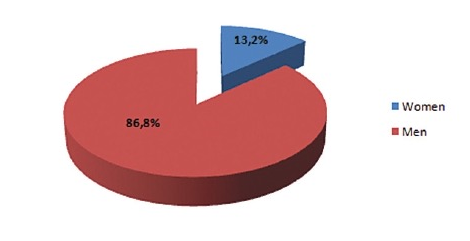
We would like to evaluate 114 patients with open mandibular fractures of the lower jaw depending on their location. As we have previously pointed out, there were identified 186 fractures. If all previously mentioned mandibular fractures are taken as 100%, the median fractures have been diagnosed in 5.9% of cases, of those 53.2% were located in the mental section, 9.7% − in the area of the body, and 31.2% periotestometry of the teeth in the angular zone (Fig 3). 15 women (13.2%) (Fig 4) and 99 men (86.8%) were examined during the study.
During the further study course, we will carry out a detailed analysis of mandibular fractures depending on their location and purpose of our examination.
The median fractures have been identified in 11 cases which make up 5.9% of all mandibular fractures. The median fractures have been diagnosed in 6 cases (1 of the patients had a single fracture and 5 patients had bilateral or segmental fractures). In median fractures, no dislocation of the fragments was found (the damage of the hard tissue was visible in the X-ray image as 'a fine thread or a hairline') in 36.4% of cases (group 1) and minimal dislocation (group 2) took place in 63.6% of cases (Fig 5).
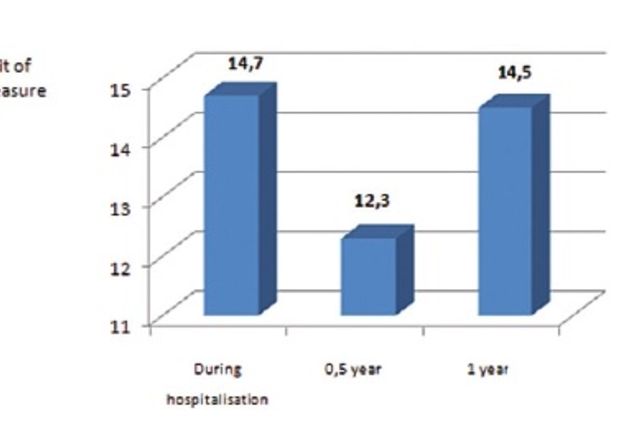
The teeth in the median fracture gap should be assigned to subgroup 1, i.e. the contact between of the root of the tooth and periodontium has been preserved along the whole length of the root. These teeth had the following perotestometry values − 1.53 ± 0.31 un. (р > 0.05). These figures did not differ significantly from those of healthy people (arithmetic mean upon periotestometry is 1.18 ± 0.24 un. for the maxilla and 1.43 ± 0,35 un. for the mandible). Almost in all patients with median mandibular fractures of the lower jaw, the contact between the teeth (in the fracture gap) and periodontium was totally preserved. The pulp vitality of these teeth was also preserved and was equal to 14.4 ± 4.7 un. During the monitoring of the patients with fractures localised in the midline (median fractures) of the lower jaw at six months and one year after the injury, it has been shown that the healing of the damaged jaw bone went smoothly, without inflammatory complications. During this period of time, there have been no clinical problems with the teeth in the fracture gap, they have not been subjected to the treatment. At six months and one year after the injury, the pulp vitality of the previously examined teeth (in the fracture gap) remained without significant changes compared both to the previous survey period (during hospitalisation) and healthy people and was 12.3 ± 3.6 un. and 14.5 ± 5.9 un, respectively. The previous results of periotestometry in the same terms have also been preserved without significant changes and were 1.42 ± 0.27 un. (р > 0.05) and 1.56 ± 0.33 un. (р > 0.05), respectively.
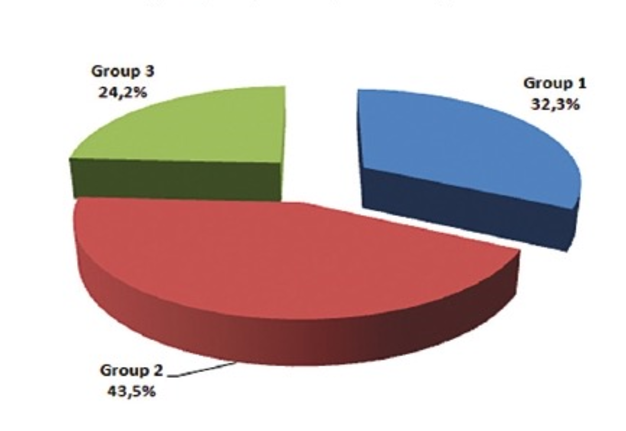
In the mental section of the mandible, the fracture of the lower jaw has been diagnosed in 99 cases (53.2%). We have revealed this localisation in 54 cases (9 patients had unilateral fractions, 45 patients had bilateral fractures). In mental mandibular fractures, the dislocation degrees of the bone fragments were as follows (Fig 7): group 1 (32.3%) − damage of hard tissue which looked like 'a fine thread or hairline' could be found in the X-ray image, group 2 (43.5%) had minimum dislocation and group 3 (24.2%) had a significant dislocation.
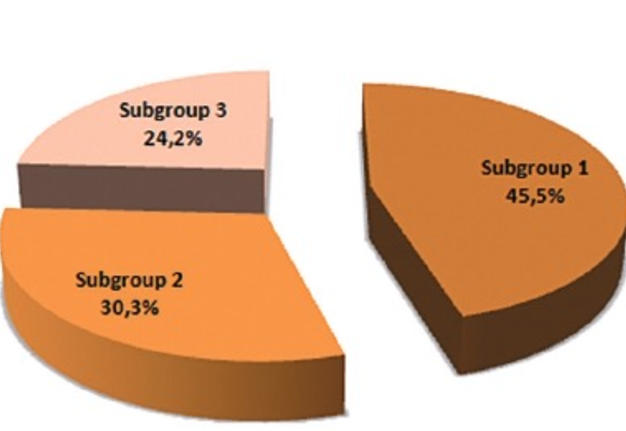
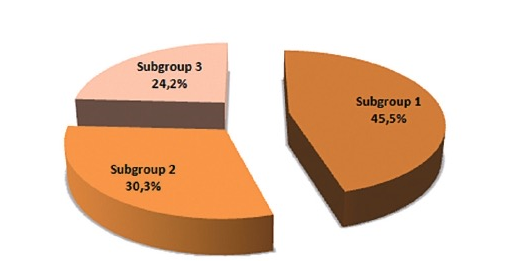
According to clinical symptoms, in all cases, in the patients with a mental mandibular fracture of the mental section a bruise (contusion) of the inferior alveolar nerve was diagnosed. In 45.5% of cases, the teeth in the mental fracture gap contacted with periodontium along its whole length of the root (subgroup 1). In 30.3% of cases, the teeth in the fracture gap must be assigned to subgroup 2, and 24.2% − to subgroup 3 (Fig 8).
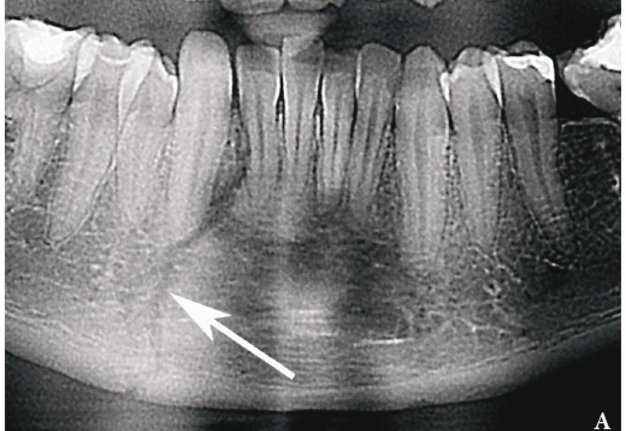
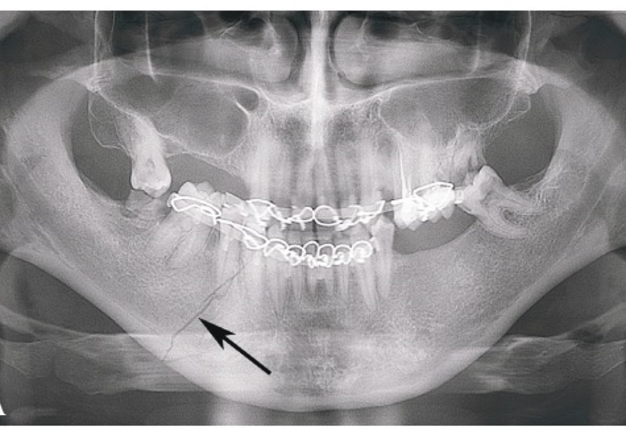
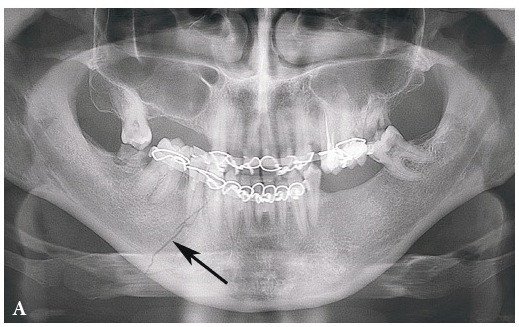
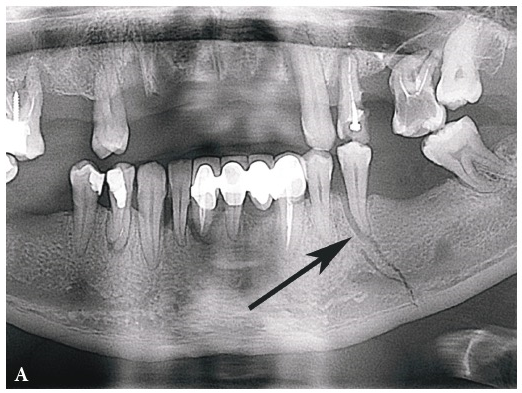
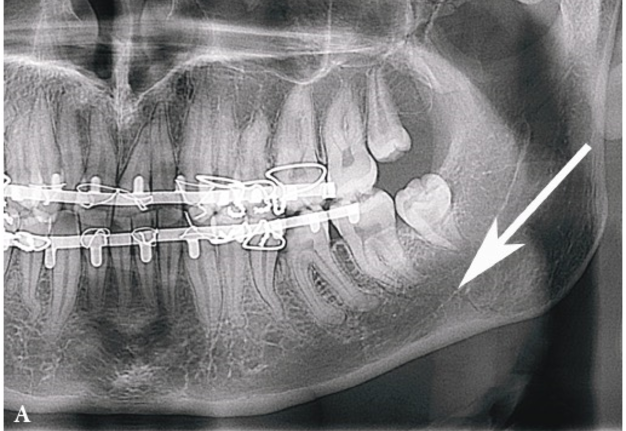
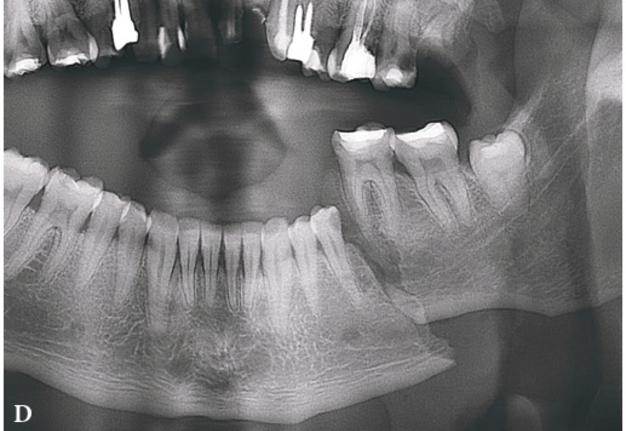
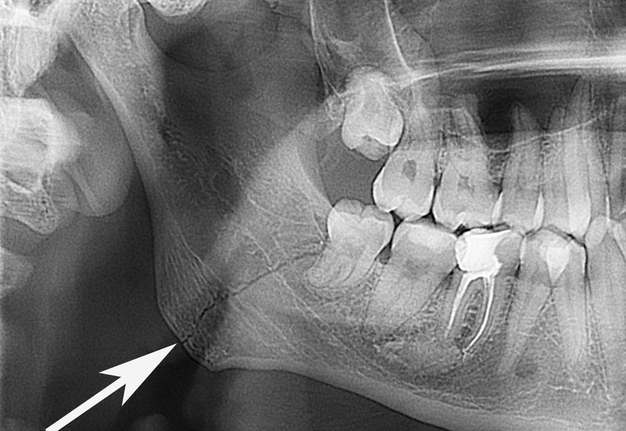
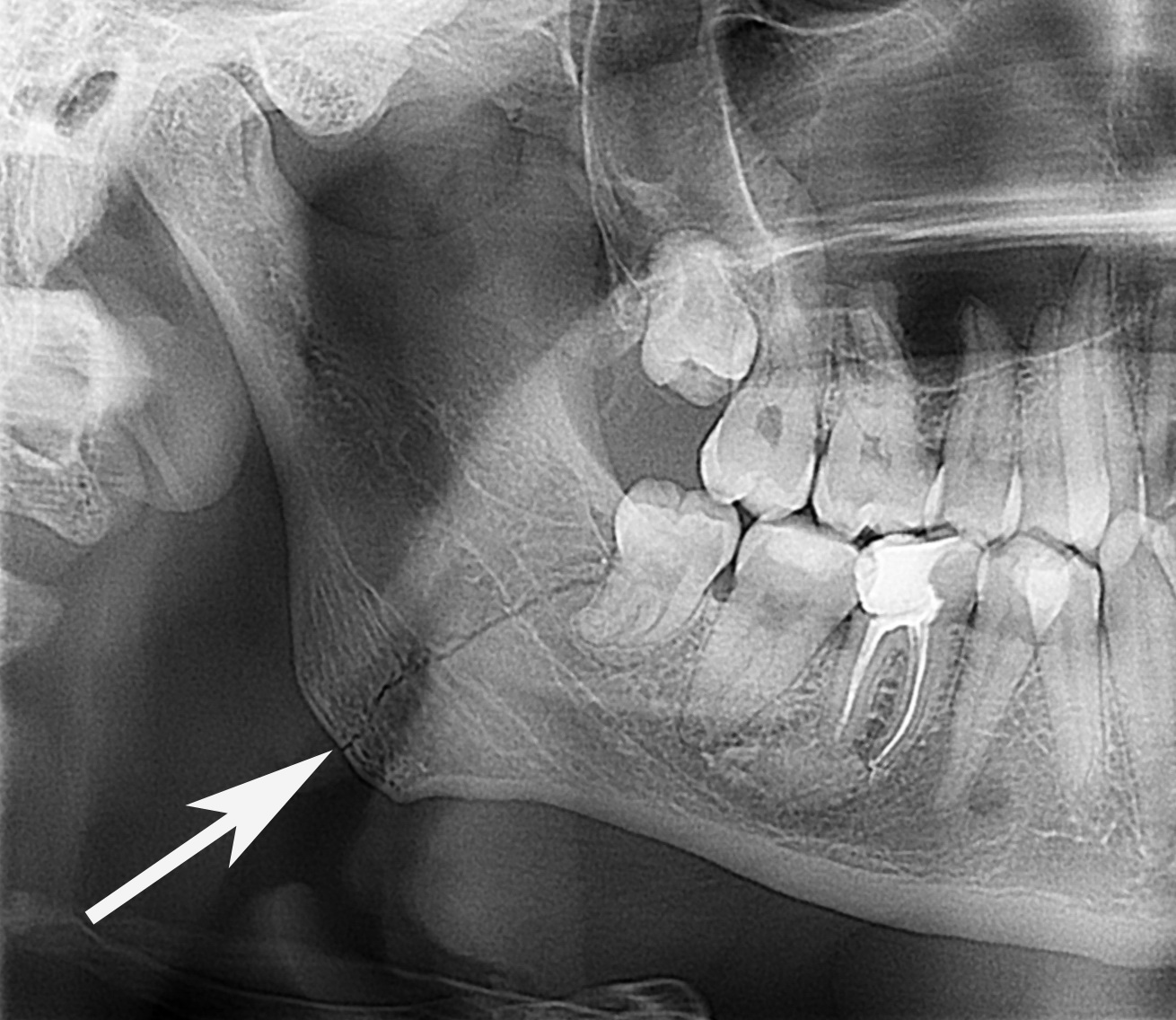
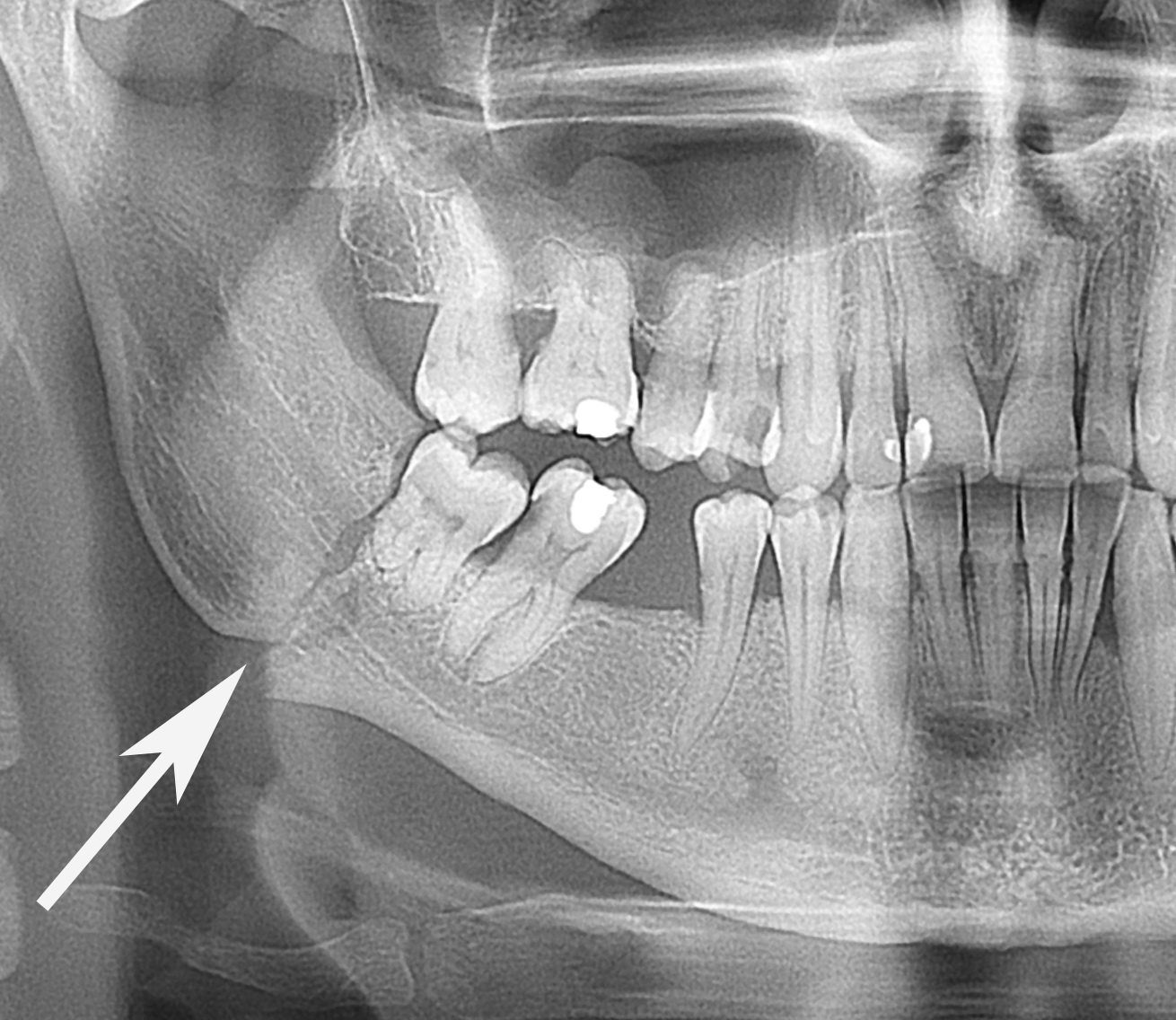
The panoramic images of the mental fractures with different degrees of dislocation of bone fragments are shown in Figures 9-11.
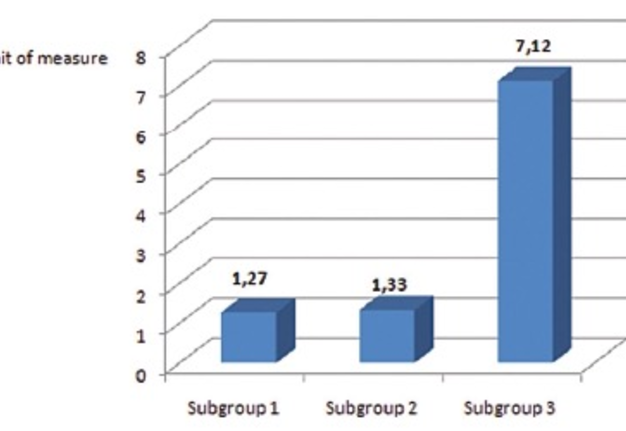
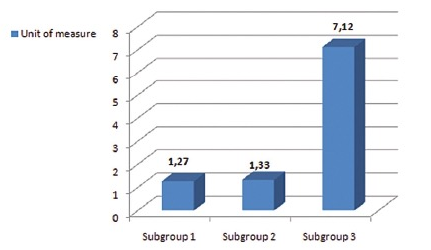
The periotestometry results for the teeth in the mental mandibular fracture gap in subgroups 1 and 2 were the following: 1.27 ± 0.42 un. (р > 0.05) and 1.33 ± 0.51 un. (р > 0.05). The obtained results did not differ from those of in healthy people. In the 3rd examined subgroup, the results of the periotestometry were increased (р < 0.001) compared to the other subgroups and normal values and were equal to 7.12 ± 0.26 un. (Fig 12).
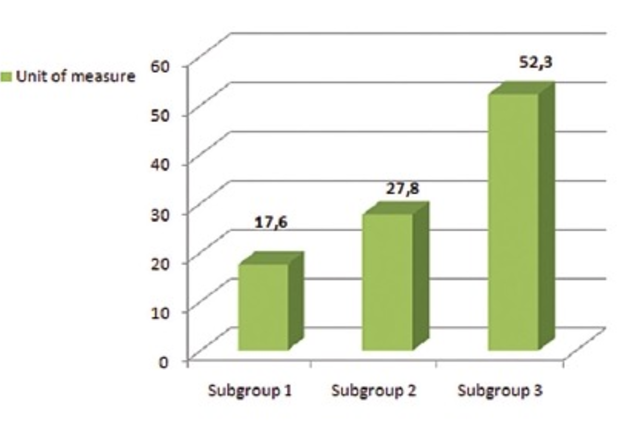
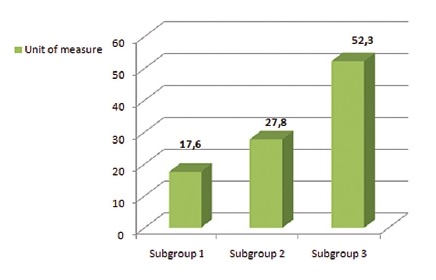
In subgroup 1, the pulp vitality of the teeth was preserved and was equal to 17.6 ± 5.4 un. In subgroup 2, the pulp vitality of the teeth differed to some extent (there was no significant difference compared to the norm) and was equal to 27.8 ± 6.8 un. In subgroup 3, the results of the pulp vitality were within the upper margin of normal values – 52.3 ± 8.6 un. (Fig 13). It should be noted that there were no pulp response in the premolar teeth located in the gap of the damaged bone in 3 patients with the mandibular fractures in the 3rd examined subgroup.
At six month and one year after the received trauma, the pulp vitality of the previously examined teeth (in fracture gap) had normalised and was 28.1 ± 6.7 un. (р > 0.05) and 25.3 ± 8.9 un. (р > 0.05), respectively. The periotestometry results in these periods were normal and were equal to 1.22 ± 0.55 un. (р > 0.05) and 1.57 ± 0.48 un. (р > 0.05), respectively.
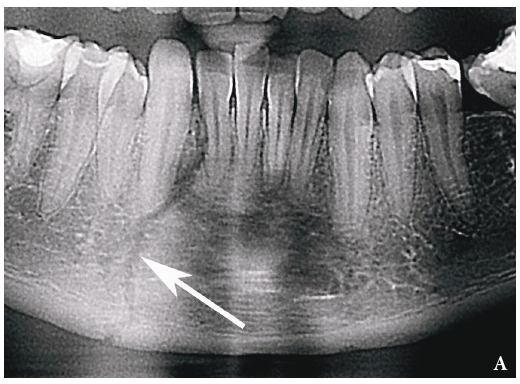
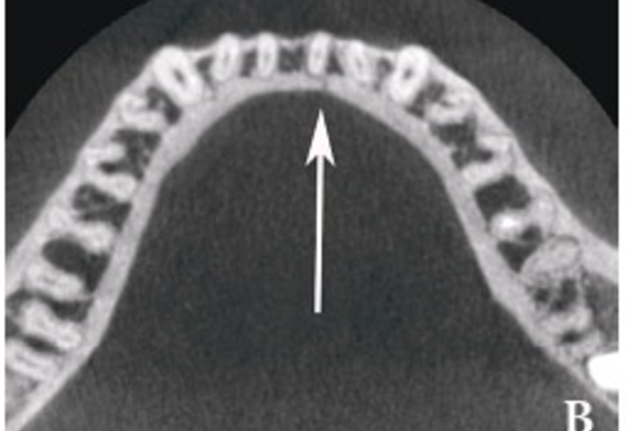
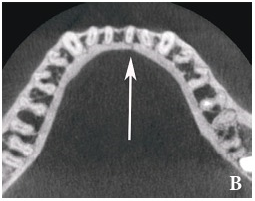
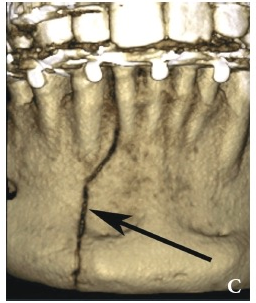
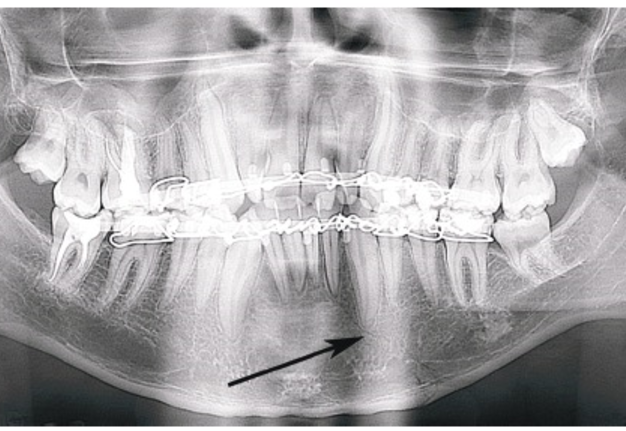
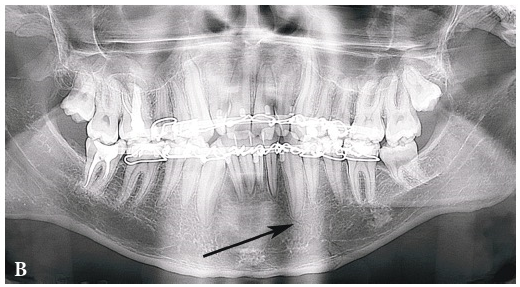
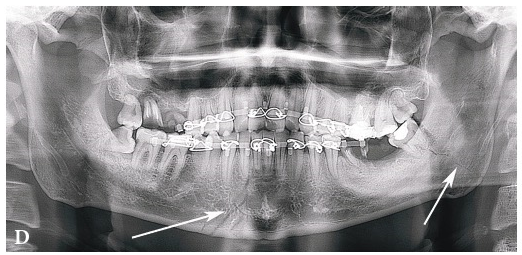
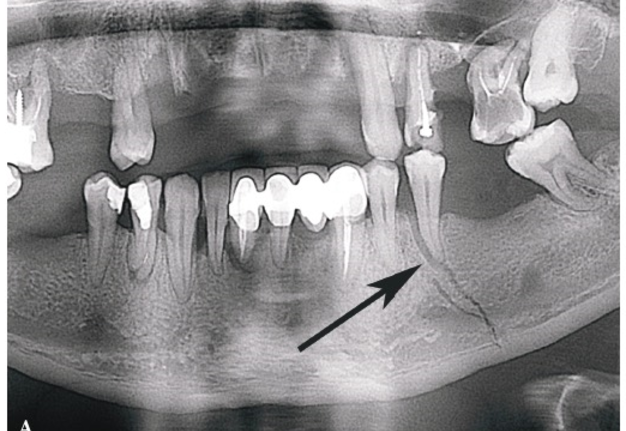
The monitoring of patients with mental mandibular fractures at six months and one year after the injury has shown that the healing of the damaged bone of the jaw did not went smoothly, i.e. there were inflammatory complications. All inflammatory complications have been observed in the 3rd examined subgroup. Two teeth in the posttraumatic period had undergone medical treatment because of recrudescence of chronic periodontitis. One patient from group 3, subgroup 3 had the osteal abscess (the abscessed tooth has been extirpated on the 5th day after the injury) and two patients developed the posttraumatic osteomyelitis of the lower jaw in the mental section after they were discharge from the hospital (Fig 14). The abscessed teeth were extracted after the posttraumatic osteomyelitis had developed. In patients with inflammatory complications of the bone and mandibular soft tissues developed upon hospitalisation, the pulp response of the tooth in the fracture gap was negative, i.e. the indices of the pulp vitality exceeded the maximum accepted norm for the canines and premolars in 1.5-2 times.
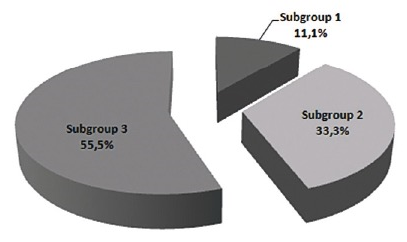
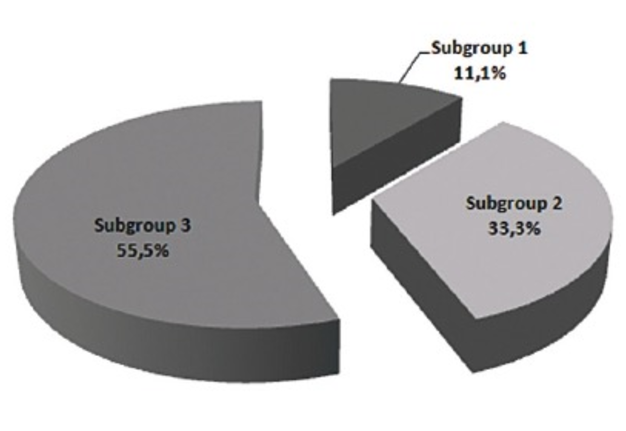
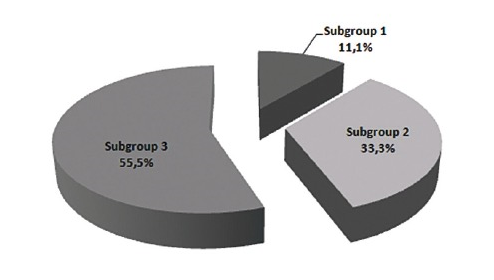
The mandibular bone fracture has been diagnosed in 18 cases (9.7%). Such a location of the fracture was found in 10 cases (there were 2 unilateral fractures and 8 bilateral fractures). In cases when the mandible was injured, the fractures were classified as follows depending on the dislocation degree of the bone fragments in mandibular bone (Fig 15): group 1 (11.1%) − damage of hard tissue which looks like 'a fine thread or hairline' could be found in the X-ray images, group 2 (33.3%) had a minimum dislocation and group 3 (55.6%) had a significant displacement.
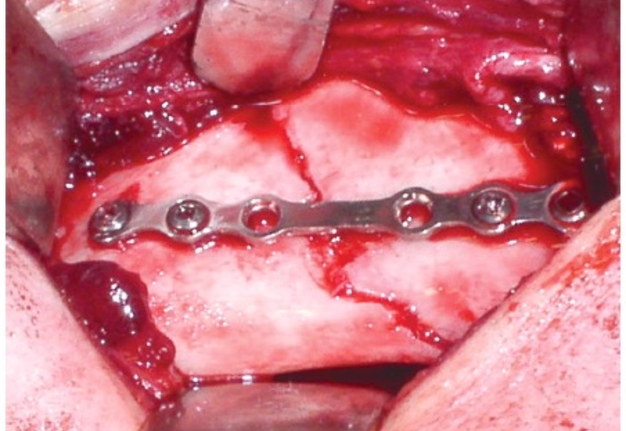
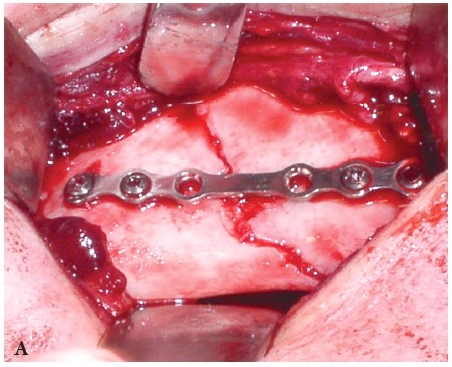
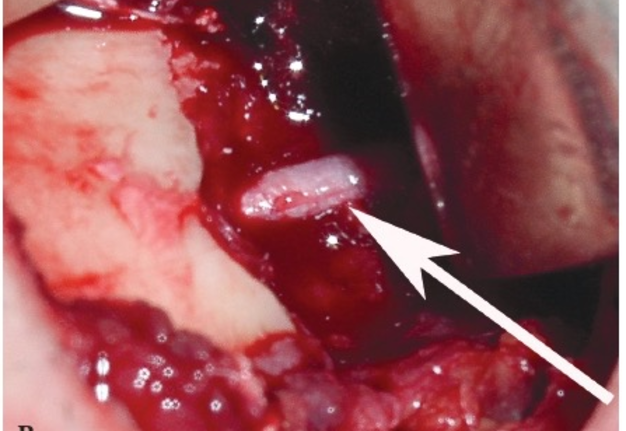
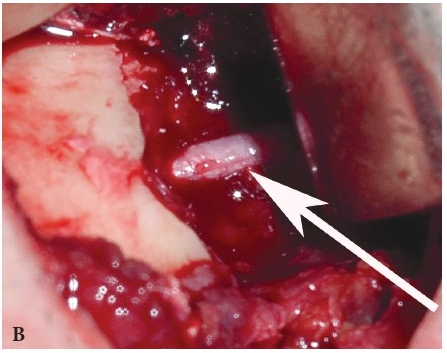
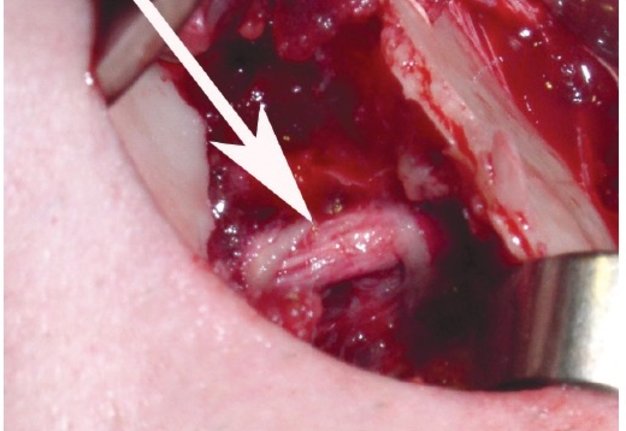
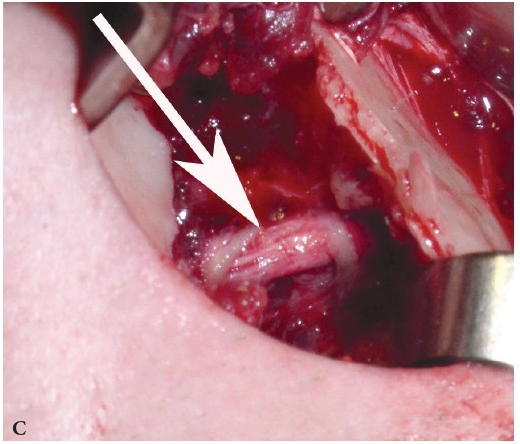
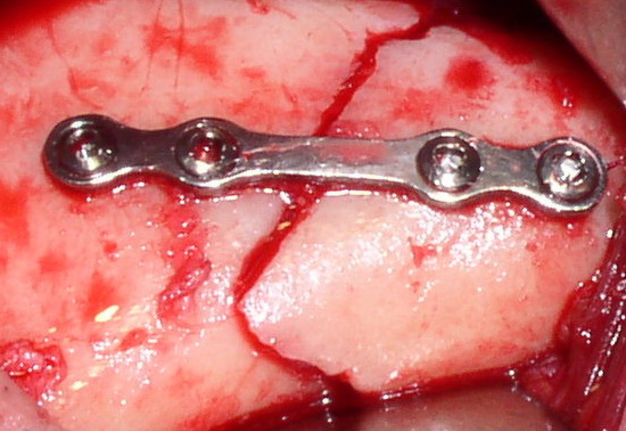
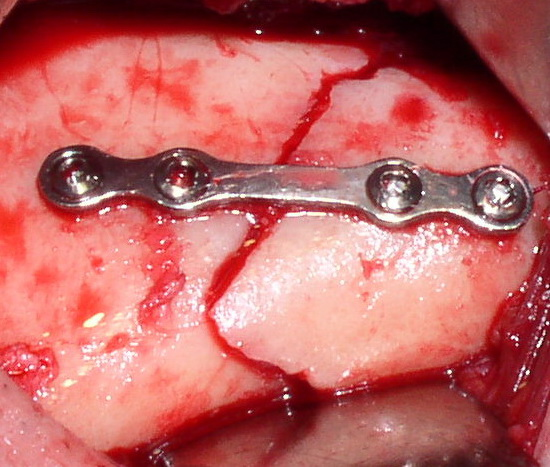
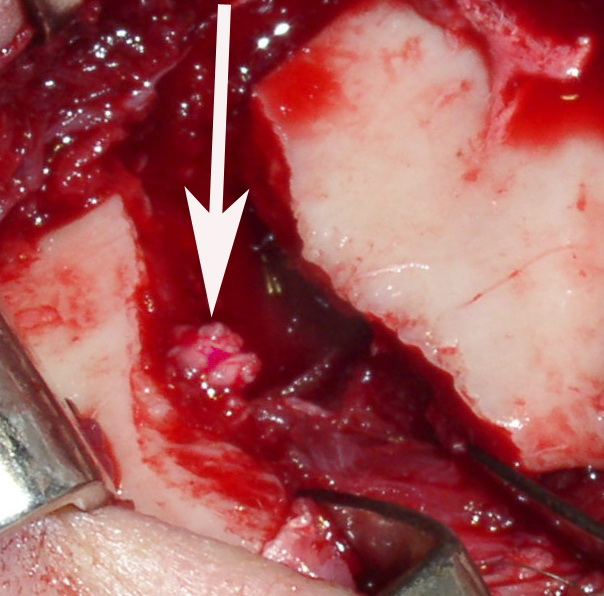
4 patients with the mandibular fractures underwent osteosynthesis of the mandible in the first days after their hospitalisation (Fig 16A). Depending on the clinical symptoms, there has been found a sprain of inferior alveolar nerve in the zone of the mandibular bone injury in 2 cases (Fig 16B) and the incomplete rupture of this nerve in 2 other cases (Fig 16C).
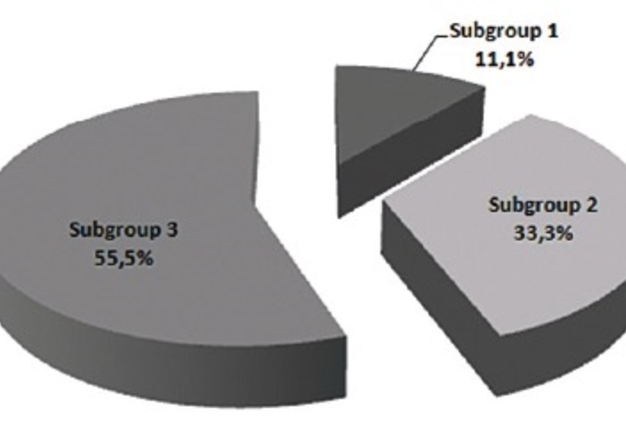
Depending on the contact area between the tooth in the fracture gap and periodontium, the fractures were distributed as follows: the teeth in the fracture gap contacted with the periodontium along its whole length in 11.1% of cases (subgroup 1); in 33.3% of cases, the teeth in the fracture gap should be assigned to subgroup 2, and in the 55.6% of cases subgroup 3 (Fig 17).
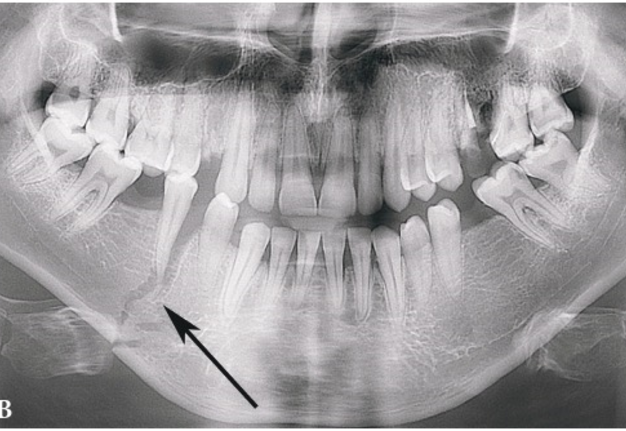
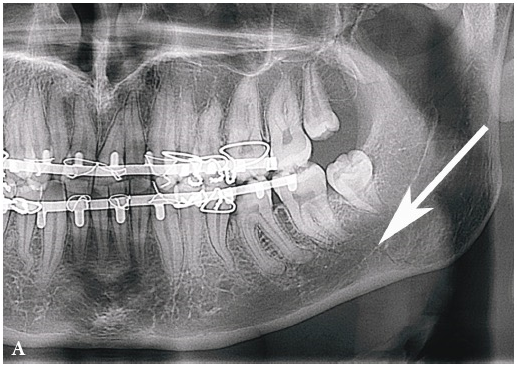
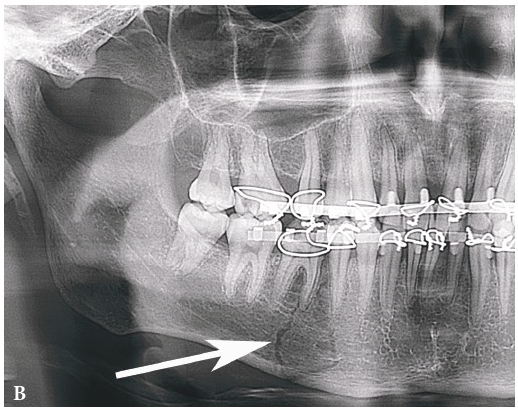
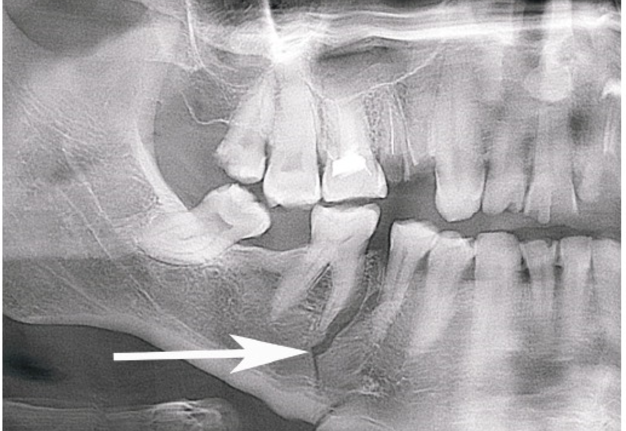
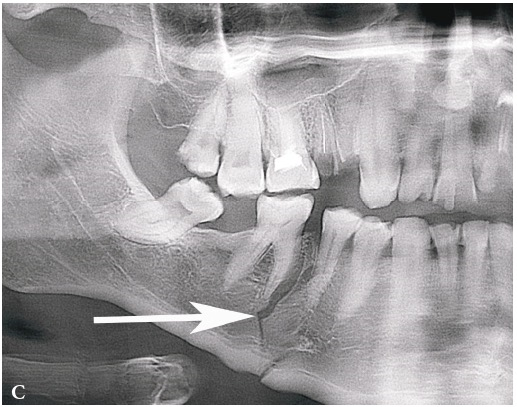
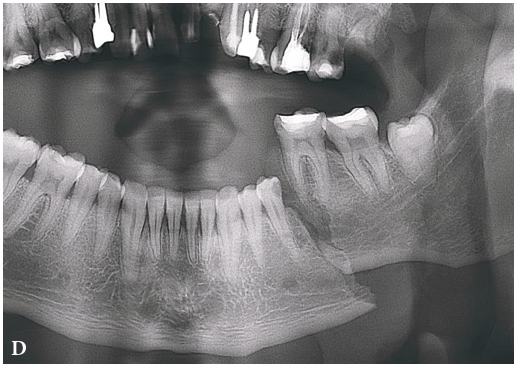
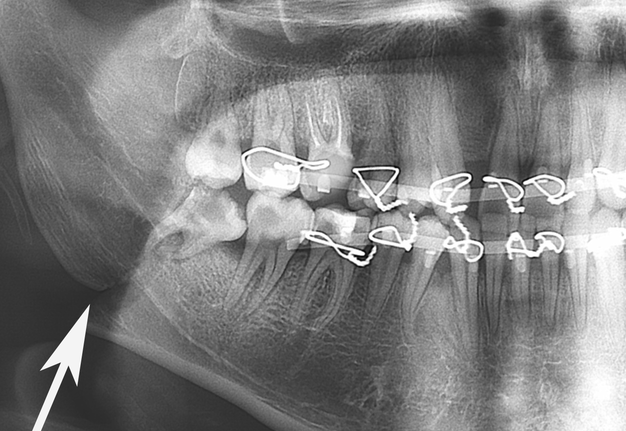
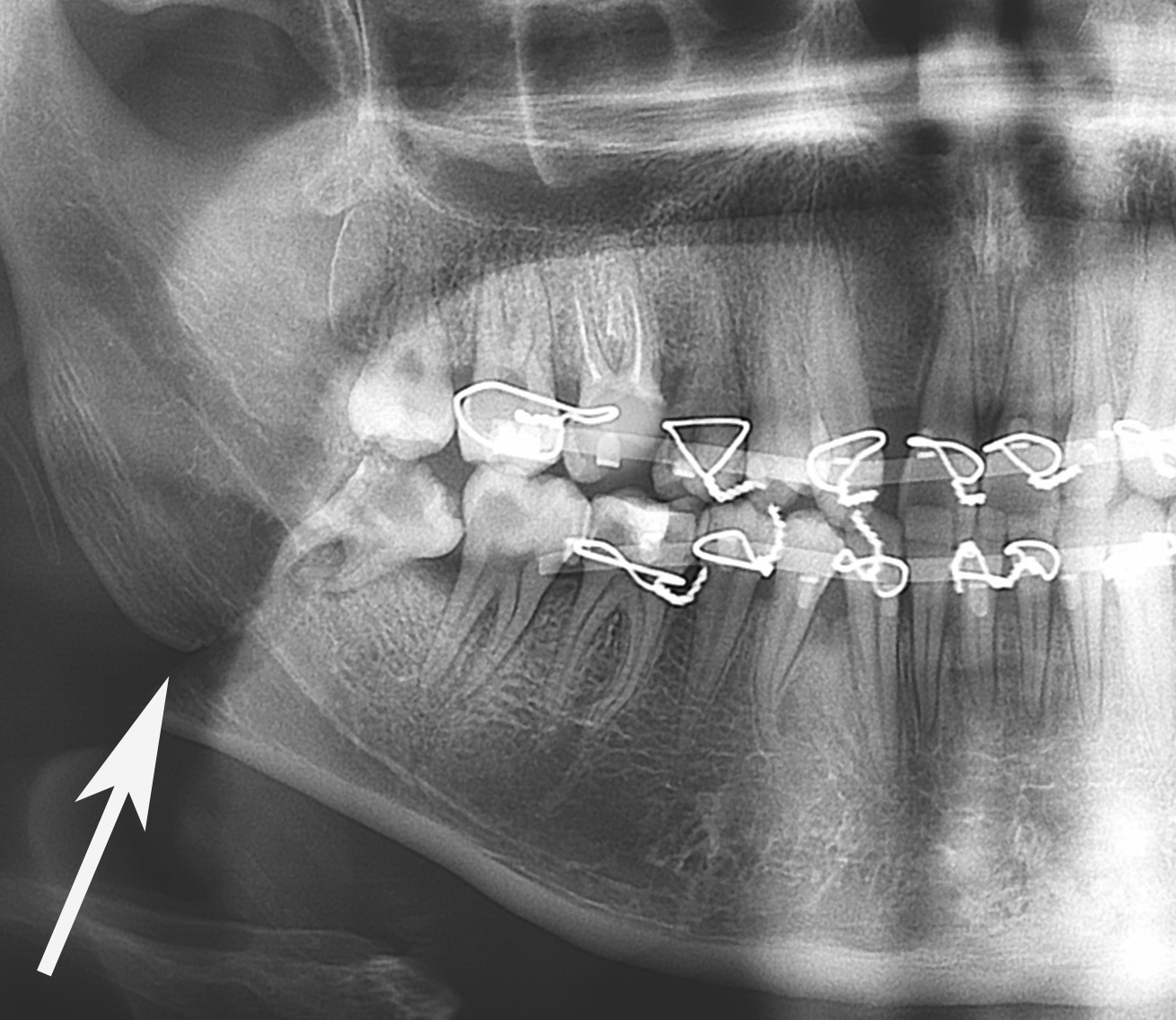
The panoramic radiographs with different degrees of fragments dislocation in the area of the lower jaw are represented in Figure 18.
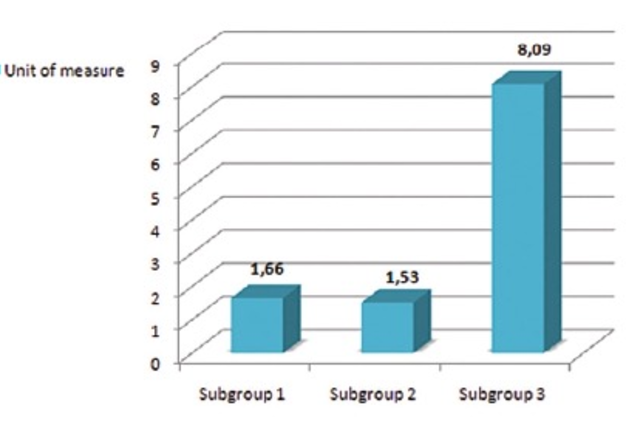
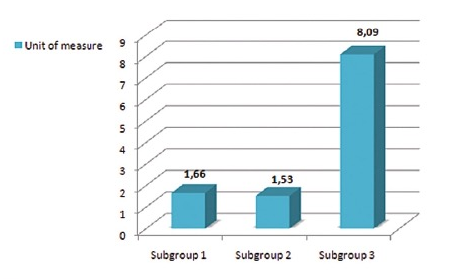
In subgroups 1 and 2, the teeth in the fracture gaps in the area of the mandible had the following periotest results: 1.66 ± 0.51 un. (р > 0.05) and 1.53 ± 0.60 un. (р > 0.05), respectively. These results did not differ significantly from that of in healthy people (arithmetic mean periotestometry results of the teeth in the lower jaw was 1.43 ± 0.35 un.). In the 3rd examined subgroup, the periotestometry results were increased (р < 0.001) compared to the other subgroups and normal values and were equal to 8.09 ± 0.31 un. (Fig 19).
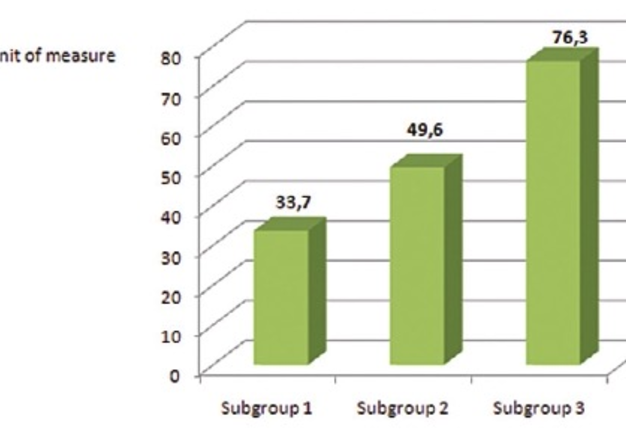
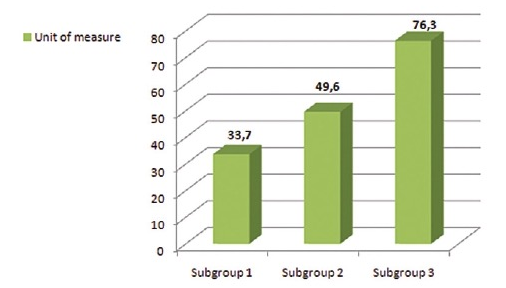
In subgroup 1, the pulp vitality of the teeth in the fracture gap of the jaw body was 33.7 ± 2.9 un. (р > 0,05). In subgroup 2, the pulp vitality of these teeth was equal to 49.6 ± 7.4 un. (р > 0.05), and in subgroup 3 (р < 0.001) it was increased and equal to 76.3 ± 9.1 un. (Fig 20). It should be noted that there was no pulp response in molar teeth in the fracture gap in 2 patients from group 3 with the mandibular fractures. From our point of view, the negative result of the pulp vitality in these cases was due to the solution of continuity of the inferior alveolar nerve in incomplete ruptures of the inferior alveolar nerve.
At six months and one year after the injury, the pulp vitality of the molars (in the fracture gap) normalised and was equal to 49.8 ± 5.7 un. (р > 0.05) and 53.2 ± 6.4 un. (р > 0.05), respectively. The periotestometry results of the molar teeth which previously were located in the fracture gap were normal in all patients at these periods and equal to 2.07 ± 0.75 un. (р > 0.05) and 1.89 ± 0.54 un. (р > 0.05).
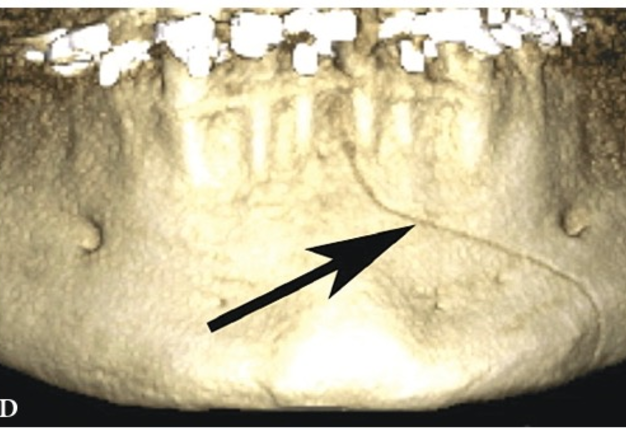
The monitoring of the patients with fractures in the body of the mandible at six months and one year after the injury has shown that there were cases when the healing of the damaged bone of the jaw had inflammatory complications. All inflammatory complications developed in the 3rd examined subgroup. The recrudescence of chronic periodontitis took place in 3 cases. In two patients with mandibular fractures (group 3, subgroup 3), the bony wound suppuraation was observed (the teeth in the fracture gap were extracted). In two cases of mandibular fractures, the posttraumatic osteomyelitis developed after the patients had been discharged from the hospital (Fig 21). In all patients with inflammatory complications developed in the bone and mandibular soft tissues after hospitalisation, the pulp response of the molar teeth which were not located in the fracture gap was negative, i.e. the indices of the vitality of the tooth pulp exceeded the maximum accepted norm for molars in 1.5-2 times.
Patients with mandibular fractures who had undergone surgical treatment (osteosynthesis) with extirpation of the tooth in the fracture gap had no post-surgical inflammatory complications.
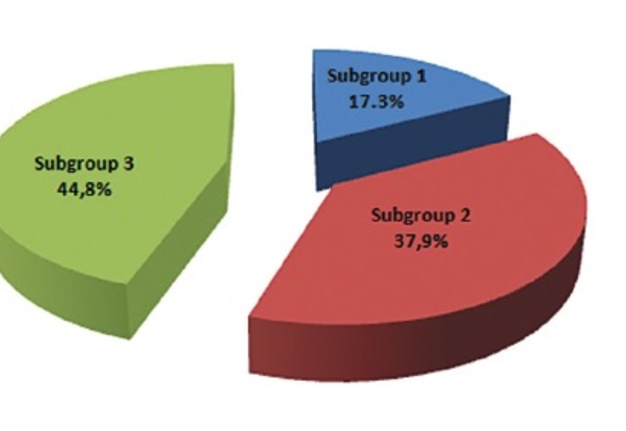
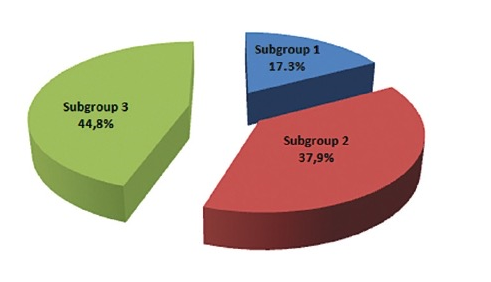
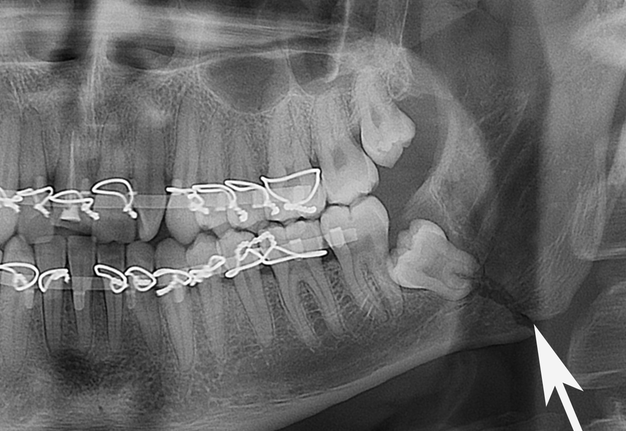
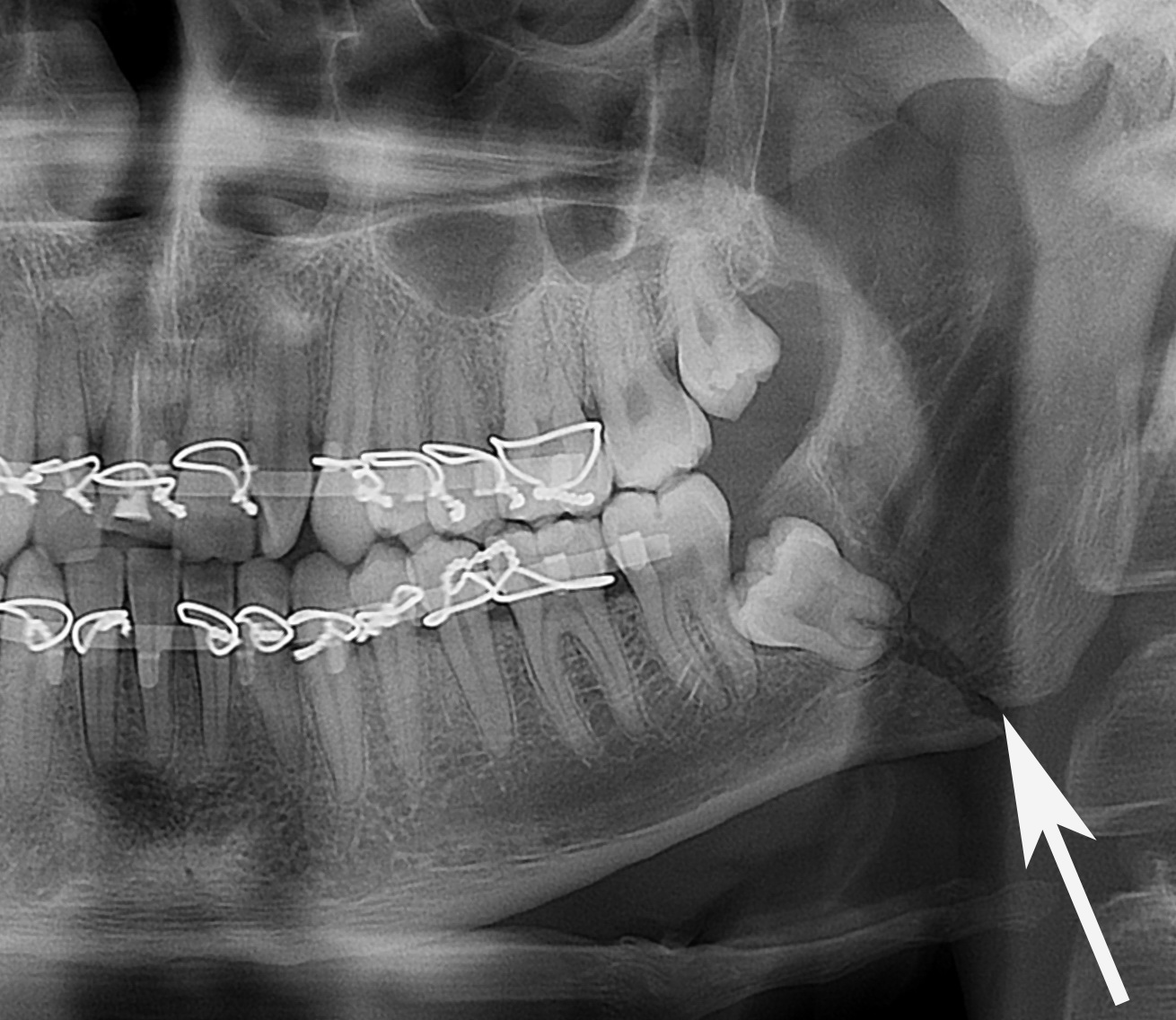
In 58 cases (31.2%), the mandibular fracture in the angle area was diagnosed. We have identified this location in 44 cases (30 patients had unilateral fractures and 14 patients had bilateral fractures). In the case of the lower jaw injuries, the fractures distribution was as follows depending on the intensity of deflection of bone fragment of mandibular angle (Fig 22): group 1 (17.3%) − damage of hard tissue which looled like a 'fine thread or hair' could be found in the X-ray images, group 2 (37.9%) had a minimal dislocation and group 3 (44.8%) had a significant dislocation.
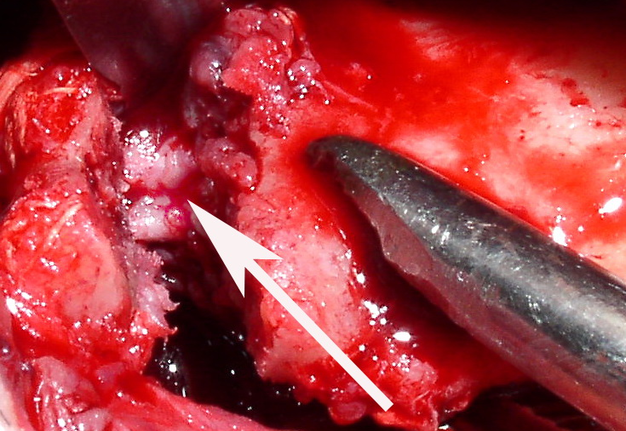
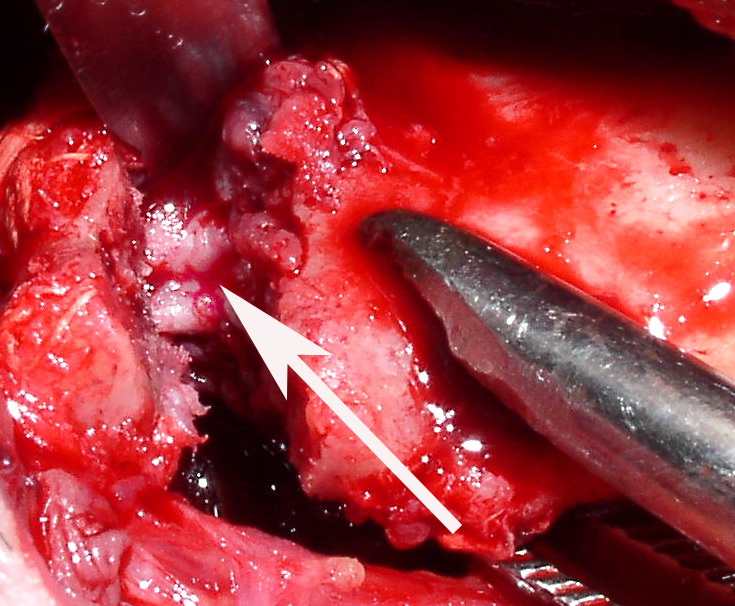
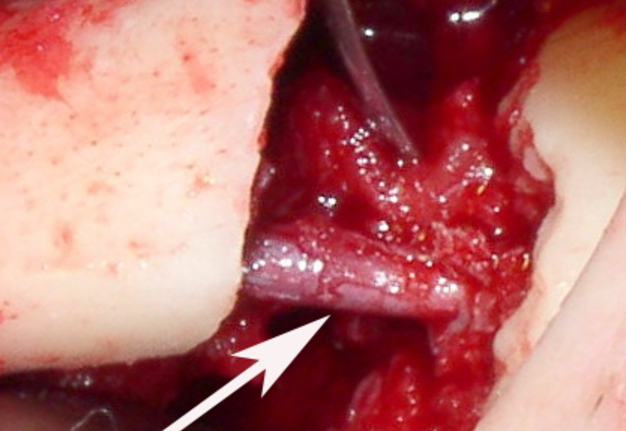
In 10 cases of the mandibular fractures, we have performed osteosynthesis of the lower jaw (Fig 16A, B). According to the clinical symptoms, in 4 of 10 patients who had been operated we found the sprain of the inferior alveolar nerve, 2 of them had the preserved vessel in the neurovascular fascicle (Fig 23C) and in another 2 cases this vessel has been ruptured (Fig 23D). 5 patients with the mandibular angle fractures had the incomplete rupture (Fig 23E), and 1 patient had the complete rupture of the inferior alveolar nerve (Fig 23F).
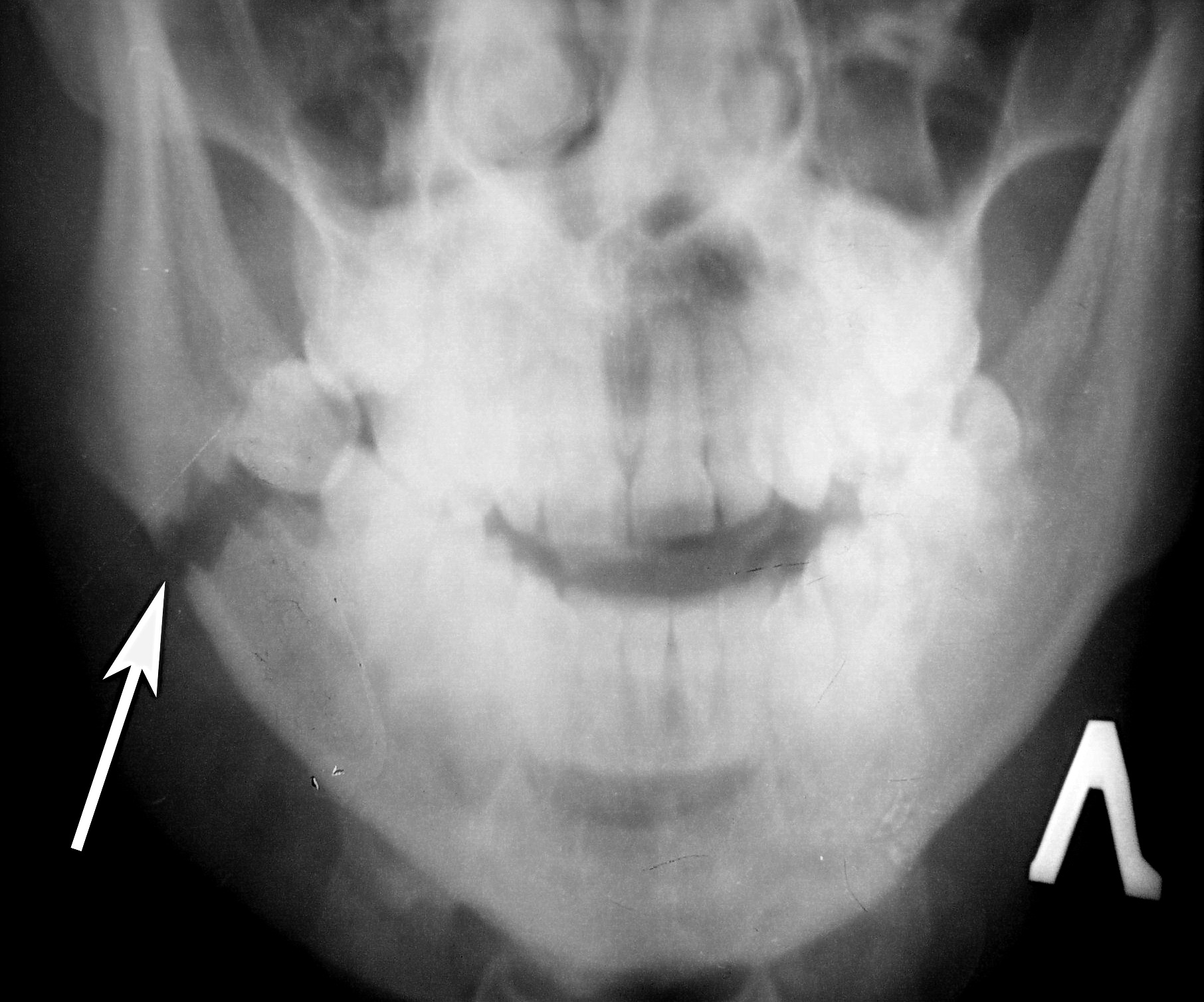
Depending on the area of contact between the tooth and periodontium in the fracture gap, the fractures in the area of mandibular angle distributed as follows: in 20.7% of cases, the teeth in the fracture gap in the body area contacted with the periodontium along its whole length s ( subgroup 1); in 34.5 % of cases, the teeth in the fracture gap should be assigned to subgroup 2, in 22.4% − to subgroup 3, and in 22.4% − to subgroup 4 (Fig 24). Upon hospitalisation, the teeth in the fracture gap were not extirpated.
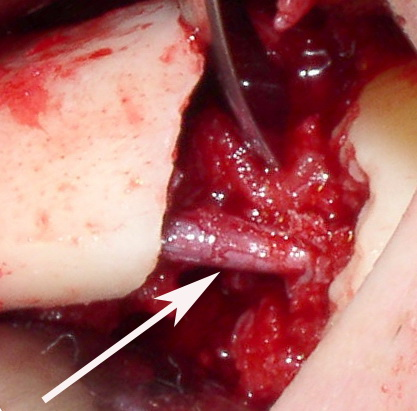
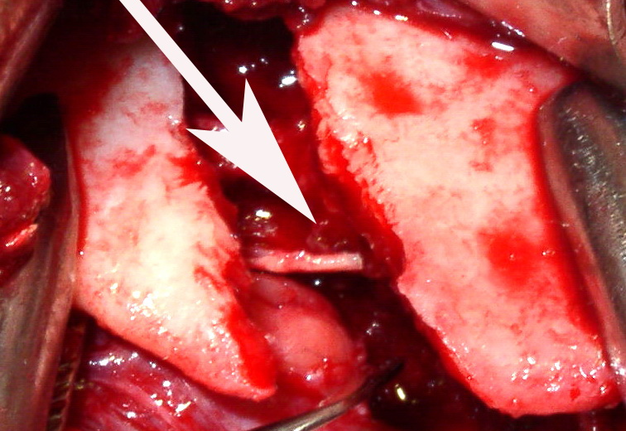
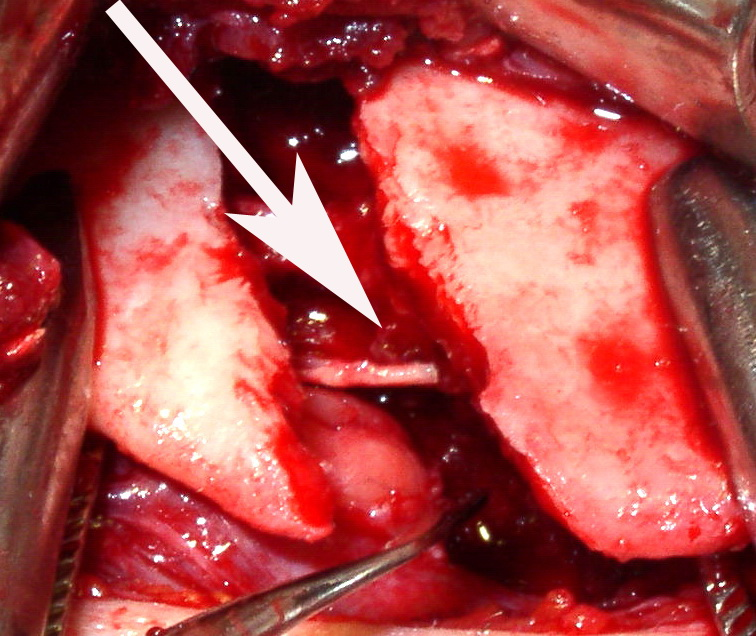
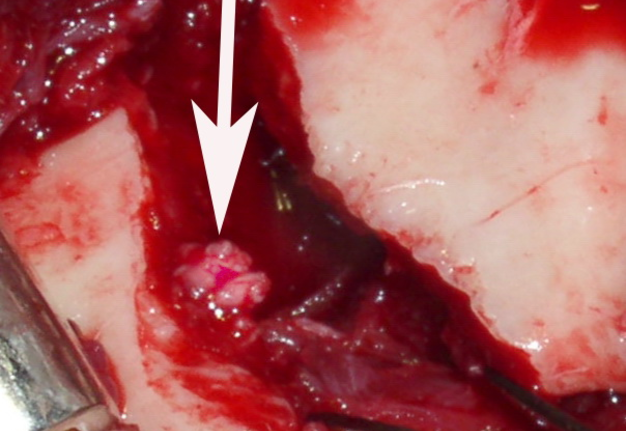
FIGURE 23A. The panoramic image of the patient after the osteosynthesis of the left angle of the mandible with the titanium miniplate, done with intraoral method (A). Stage of osteosynthesis of the mandible made by extraoral method (B). The appearance of the stretched inferior alveolar nerve and preserved vessel in the neurovascular bundle (arrow) (C). Stretching of the inferior alveolar nerve (arrow) after the rupture of the vascular bundle (D). Incomplete (E) and complete (F) rupture of the inferior alveolar nerve (arrow).
FIGURE 23B. The panoramic image of the patient after the osteosynthesis of the left angle of the mandible with the titanium miniplate, done with intraoral method (A). Stage of osteosynthesis of the mandible made by extraoral method (B). The appearance of the stretched inferior alveolar nerve and preserved vessel in the neurovascular bundle (arrow) (C). Stretching of the inferior alveolar nerve (arrow) after the rupture of the vascular bundle (D). Incomplete (E) and complete (F) rupture of the inferior alveolar nerve (arrow).
FIGURE 23C. The panoramic image of the patient after the osteosynthesis of the left angle of the mandible with the titanium miniplate, done with intraoral method (A). Stage of osteosynthesis of the mandible made by extraoral method (B). The appearance of the stretched inferior alveolar nerve and preserved vessel in the neurovascular bundle (arrow) (C). Stretching of the inferior alveolar nerve (arrow) after the rupture of the vascular bundle (D). Incomplete (E) and complete (F) rupture of the inferior alveolar nerve (arrow).
FIGURE 23D. The panoramic image of the patient after the osteosynthesis of the left angle of the mandible with the titanium miniplate, done with intraoral method (A). Stage of osteosynthesis of the mandible made by extraoral method (B). The appearance of the stretched inferior alveolar nerve and preserved vessel in the neurovascular bundle (arrow) (C). Stretching of the inferior alveolar nerve (arrow) after the rupture of the vascular bundle (D). Incomplete (E) and complete (F) rupture of the inferior alveolar nerve (arrow).
FIGURE 23E. The panoramic image of the patient after the osteosynthesis of the left angle of the mandible with the titanium miniplate, done with intraoral method (A). Stage of osteosynthesis of the mandible made by extraoral method (B). The appearance of the stretched inferior alveolar nerve and preserved vessel in the neurovascular bundle (arrow) (C). Stretching of the inferior alveolar nerve (arrow) after the rupture of the vascular bundle (D). Incomplete (E) and complete (F) rupture of the inferior alveolar nerve (arrow).
FIGURE 23F. The panoramic image of the patient after the osteosynthesis of the left angle of the mandible with the titanium miniplate, done with intraoral method (A). Stage of osteosynthesis of the mandible made by extraoral method (B). The appearance of the stretched inferior alveolar nerve and preserved vessel in the neurovascular bundle (arrow) (C). Stretching of the inferior alveolar nerve (arrow) after the rupture of the vascular bundle (D). Incomplete (E) and complete (F) rupture of the inferior alveolar nerve (arrow).
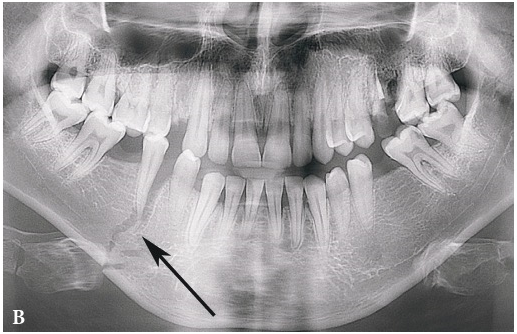
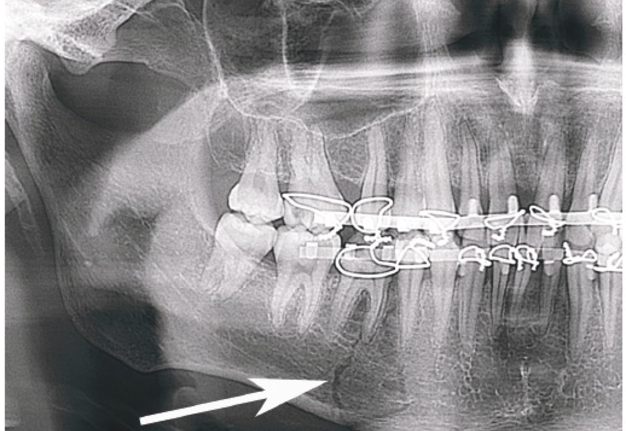
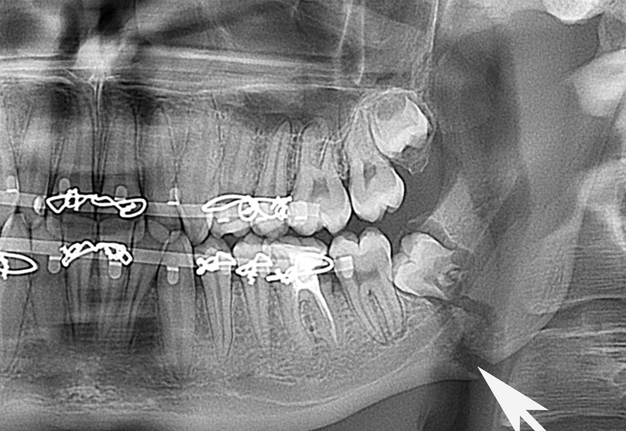
The X-ray images of the fractures with the different degree of dislocation of the bone fragments in the mandibular angle are represented by the Figure 25.
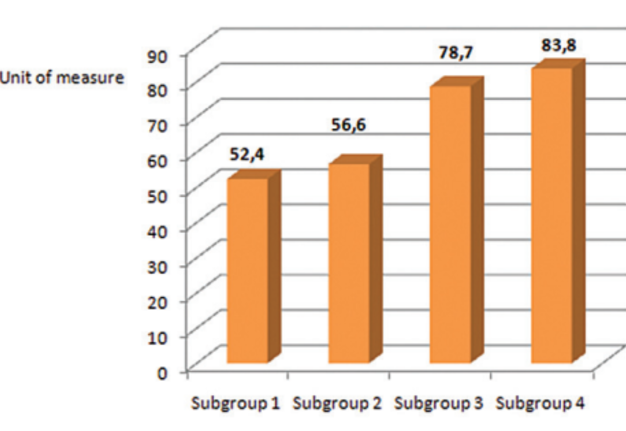
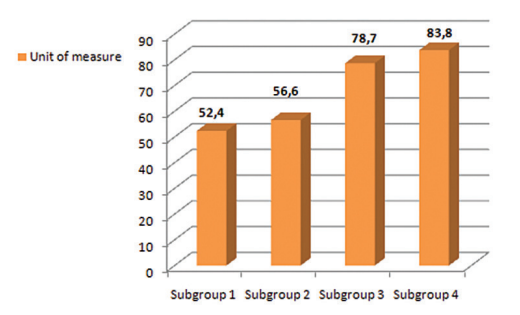
In subgroup 1, the pulp vitality of the teeth in the fracture gap in the mandibular angle was equal to 52.4 ± 6.5 un. (р > 0.05). In subgroup 2, the pulp vitality was 56.6 ± 7.1 un. (р > 0.05), in subgroup 3 it was 78.7 ± 6.8 un. (р < 0.001), and in subgroup 4 it was 83.8 ± 7.9 un. (р < 0.001) (Fig 26). It should be noted that 3 patients with the mandibular fractures from group 3 had no pulp response in molar teeth in the fracture gap. In subgroup 4, more than 50% of the examined patients (7 injured) also had no pulp response of the teeth in the fracture gap, i.e. the response was negative. From our point of view, the negative results of pulp vitality in these cases was due to the injury of the inferior alveolar nerve (the stretching, incomplete and complete rupture).
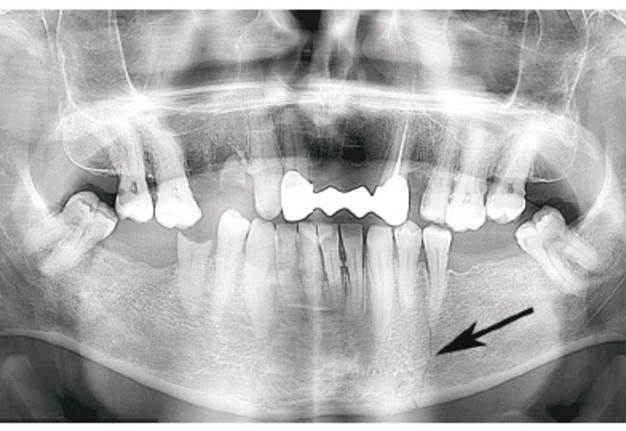
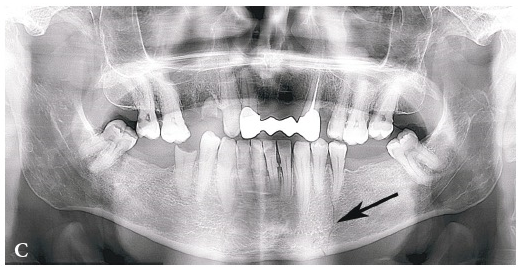
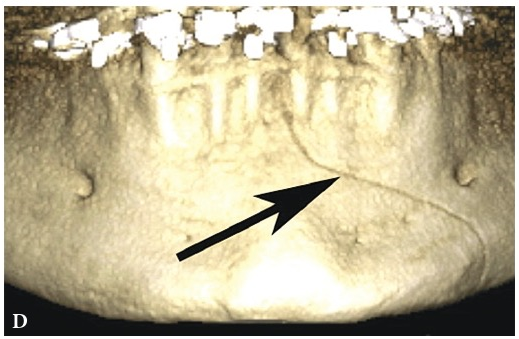
The monitoring of the patients with mandibular angle fractures at six months and one year after the injury has shown that there were some cases when the healing of the damaged bony tissue of the jaw had inflammatory complications. In patients from subgroups 3 and 4, the recrudescence of chronic periodontitis in the third molars occurred in 4 cases. The five injured persons with the mandibular bone fractures (in subgroups 3 and 4) had the bony wound suppuration (these teeth in the fracture gap have been extracted as a part of the treatment). Four patients with the mandibular angle fractures (in subgroups 3 and 4) experienced the post-traumatic osteomyelitis (Fig 27). In the patients with inflammatory complications developed in the bone and premandibular soft tissues upon hospitalisation, the pulp response of three molars in the fracture gap was negative, i.e. the indices of pulp vitality exceeded the maximum accepted norm for molars in 2 and more times.
In patients with the mandibular angle fracture who had undergone the surgical treatment (osteosynthesis) with the extirpation of the tooth in the fracture gap, the post-traumatic osteomyelitis has developed only in one case (the etiological tooth has been extracted in the postsurgical period). From our point of view, the reason for the development of this complication was the non-fulfillment of mouth cavity hygiene rules and other violations.
At six months and one year after the injury, the pulp vitality of the third molars (in the fracture gap) normalised and was 54.1 ± 7.6 un. (< 0.05) and 58.9 ± 5.9 un. (< 0.05), respectively.
Therefore, having analysed 186 cases of open mandibular fractures, we have found out that in 63 cases (33.9%) the tooth located in the fracture gap (along with the whole length of the root) fully contacted with the surrounding periodontium (group 1). In 63 cases (33.9%), there has been presented the disruption of the contact between the tooth root and periodontium in the fracture gap along the 1/3 of root length (subgroup 2). In 47 cases (25.3%), the contact between the root of the tooth in the fracture gap and periodontium was disrupted along the 1/2 of its root length (subgroup 3). In 13 cases (6.9%), the contact between the root of the tooth in the fracture gap and periodontium was disrupted along the 3/4 of its length.
It was found that the inflammable complications took place only in subgroups 3 and 4. In these examined subgroups, the pulp vitality of the tooth in the fracture gap also was declined. The results of the pulp vitality of these teeth exceeded the maximum norm for the teeth of the corresponding localisation in 1,5-2 times and more. All inflammatory complications originated in the teeth with the outlined deviances. In the case of the solution of continuity of the mandibular bone in the mental divisions, subgroup 3 included 24 fractures with inflammatory complications in 5 cases (2 − the recrudescence of chronic periodontitis, 1 − suppuration of the bony wound, 2 − posttraumatic osteomyelitis), i.e. the inflammatory complications in this subgroup evolved in 20.8% of cases. Among the injuries of the lower jaw in subgroup 3, there were 10 fractures and the inflammable complications developed in 7 cases (3 − the recrudescence of chronic periodontitis, 2 – suppuration of the bony wound, 2 − posttraumatic osteomyelitis), i.e. the inflammatory complications in this subgroup have evolved in 70.0% of cases of all injuries in this subgroup. We believe that in cases of the mandibular fractures when the contact of the tooth in the fracture gap with the surrounding periodontium was disrupted, the increased rate of the inflammatory complications was due to the extremely rare localisation of such damages. In subgroups 3 and 4, there were 26 fractures with the solution of continuity of bone in the mandibular angle. The inflammatory complications in the mandible angle were found in 13 cases (4 − the recrudescence of chronic periodontitis, 5 − suppuration of the bony wound, 4 − posttraumatic osteomyelitis), i.e. the inflammable complications in this subgroup have evolved in 50.0% of cases of all injuries in subgroups 3 and 4.
According to our examination of the patients with the open mandibular fractures, we have revealed that in more than 50% of cases, the posttraumatic inflammable complications (the recrudescence of chronic periodontitis, suppuration of the bony wound, posttraumatic osteomyelitis) developed after the mandibular fractures in the molar area when the contact between the roots of the teeth in the fracture gap and periodontium of the given teeth was disrupted along 1/2 of its length and more. The preservation of the teeth in the fracture gap when the contact between the roots of the teeth in the fracture gap and the surrounding periodontium of the given teeth is disrupted along 1/2 to and 3/4 of the root’s length creates a high risk of the inflammatory complications progression in bone and surrounding mandible soft tissues.
References (4)
-
Tymofieiev OO. Schelepno-lytseva hirurgiia [Maxillofacial surgery]. 1st ed. Kyiv: Meditsyna; 2011. p. 473−5 (in Ukrainian).
-
Timofieiev AA. Rukovodstvo po chelustno-litsevoi hirurgii i hirurgicheskoi stomatologii [Manual of maxillofacial and oral surgery]. 5th ed. Kyiv: Chervona Ruta-Turs; 2012. p. 741−6 (in Russian).
-
Timofieiev AA. Chelustno-litsevaia hirurgiia [Maxillofacial surgery]. 2nd ed. Kyiv: Meditsina; 2015. p. 498−501 (in Russian).
-
Jimson S, Reena J, Shalini J. Teeth in the line of fracture: to retain or remove? Craniomaxillofac Trauma Reconstruction 2010;3:177−184.