State of the Art Simultaneous Bilateral Segmental Mandibular Reconstruction using a Single Fibula Transplant: Discussion of the Surgical Steps
March 31, 2019
https://doi.org/10.23999/j.dtomp.2019.3.2
J Diagn Treat Oral Maxillofac Pathol 2019;3:76−103.
Under a Creative Commons license
HOW TO CITE THIS ARTICLE
Hanna TC, Kraus DH. State of the art simultaneous bilateral segmental mandibular reconstruction using a single fibula transplant: discussion of the surgical steps. J Diagn Treat Oral Maxillofac Pathol 2019;3(3):76−103.
Contents: Summary | Introduction | Case and Discussion | Conflict of Interest | Role of Co-Authors | Fundings | References (41)
Summary
During last 22 years the different reports have shown successful using of vascularized single fibular transplant for a simultaneous bilateral segmental mandibular reconstruction. The surgeries were performed in cases of bilateral mandibular defects of different origin: 1) bilateral infected pseudoarthrosis, 2) bilateral squamous cell carcinoma of the mandible, 3) bilateral ossifying fibroma, 4) osteoradionecrosis that caused mandibular defects, and 5) traumatic mandibular defects. We present a case of a 60-year-old patient who was referred to our clinic with osteoradionecrosis of bilateral mandible, which was reconstructed using a single fibula flap. A 6-month follow-up images are presented.
This is the first report of a bilateral mandibular angle functional reconstruction with a single fibula free vascularized flap. Its particular vascularization allows not only osteotomies but also ostectomy of a middle shaft.5
—Hervé Reychler et al, 1997
Belgium
Introduction
Using of the free fibula flaps in mandibular reconstruction was popularized by Hidalgo in 1989.1, 2, 3, 4 Reychler et al5 in 1997 reported a first result of a bilateral mandibular angle functional reconstruction with a single fibula free vascularized flap. For almost twenty-two years, from 1997 to 2019, the different authors reconstructed bilateral defects on the mandible according to next etiologies:
- Reychler et al, 1997 – for a bilateral infected pseudoarthrosis.5
- Bianchi et al, 2008 – because of a rare bilateral squamous cell carcinoma of the mandible.6
- Mello-Filho et al, 2008 – according to bilateral ossifying fibroma.7
- Jacobson et al, 20108 and Chen et al, 20189 – because of an osteoradionecrosis that caused mandibular defects.
- Ekanayake et al, 2013 – for a traumatic origin (shrapnel injury: a patient had 2 segmental defects with intact mandibular rami with condyles and intact mandibular symphyses).10
The goal of that report is to highlight and discuss the consecutive stages of using vascularized single fibular transplant for a simultaneous bilateral segmental mandibular reconstruction (BSMR) in a 60-year-old patient who presented with osteoradionecrosis of the bilateral mandible due to radiation injury.
Case and Discussion
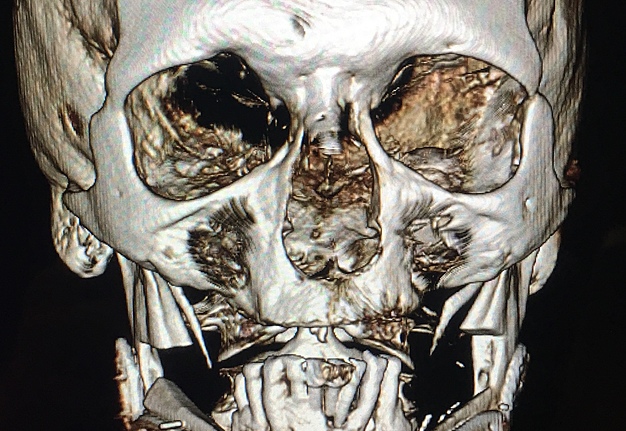
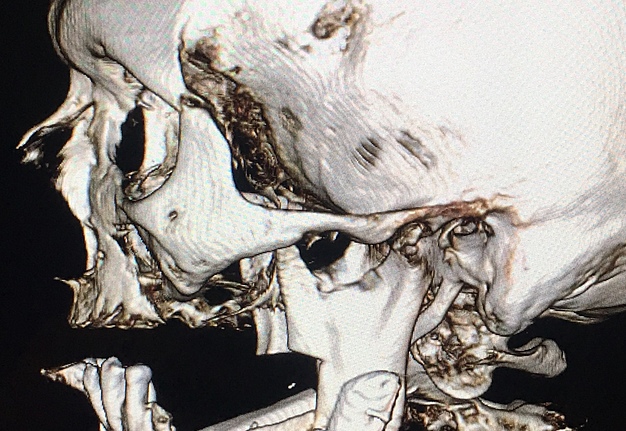
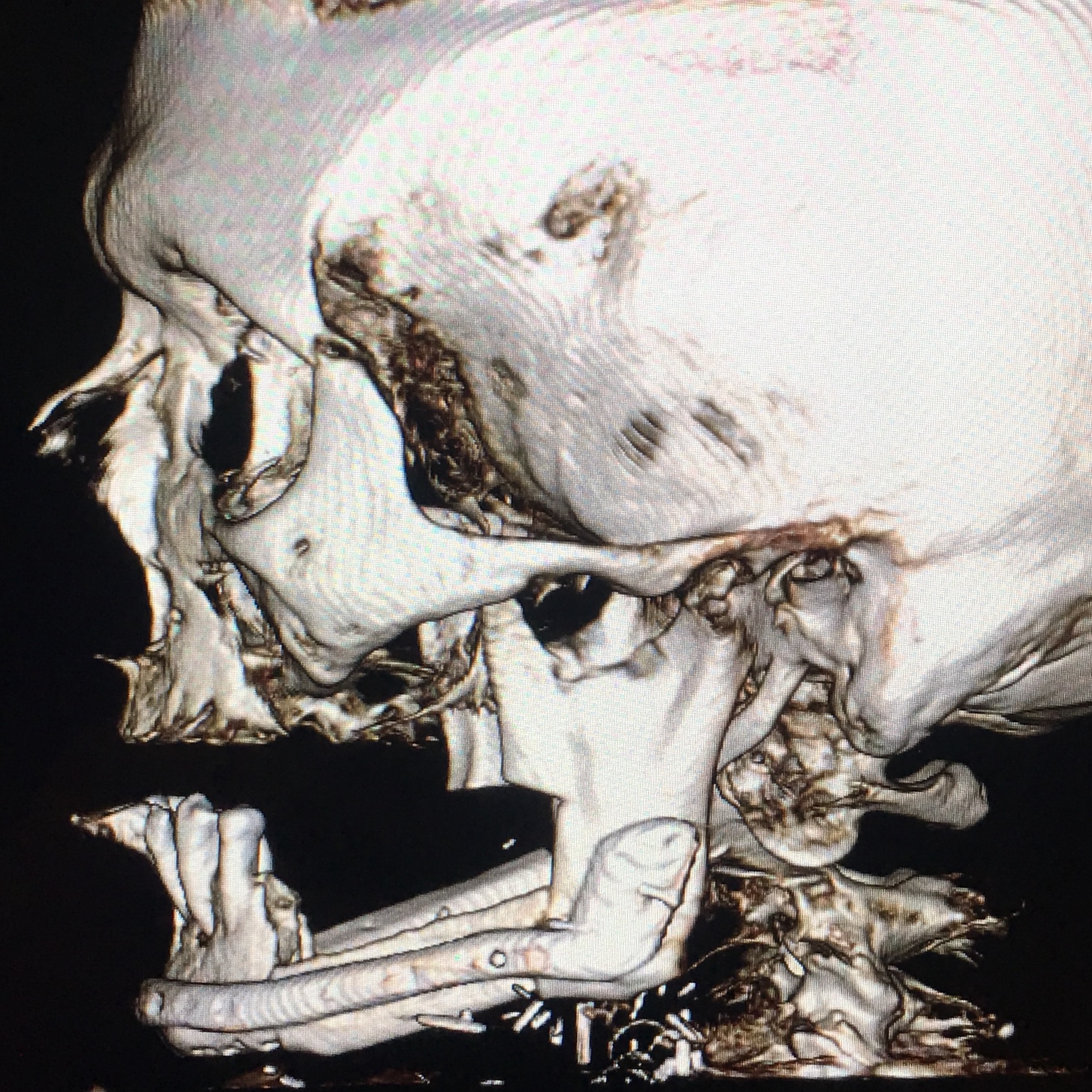
A 60-year-old white male patient referred to our Clinic with a diagnosis–osteoradionecrosis of the bilateral mandible due to radiation injury (which was done for nonsurgical cancer treatment). A perfect staging classification of osteoradionecrosis11, 12 is described by Chronopoulus et al (2018).13 In our case two isolated bilateral mandibular defects (according to Schrag et al systematization – Table 1) were expected.14
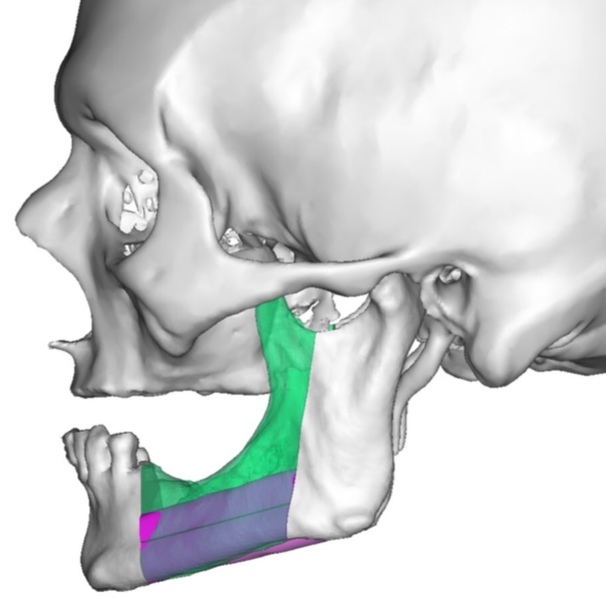
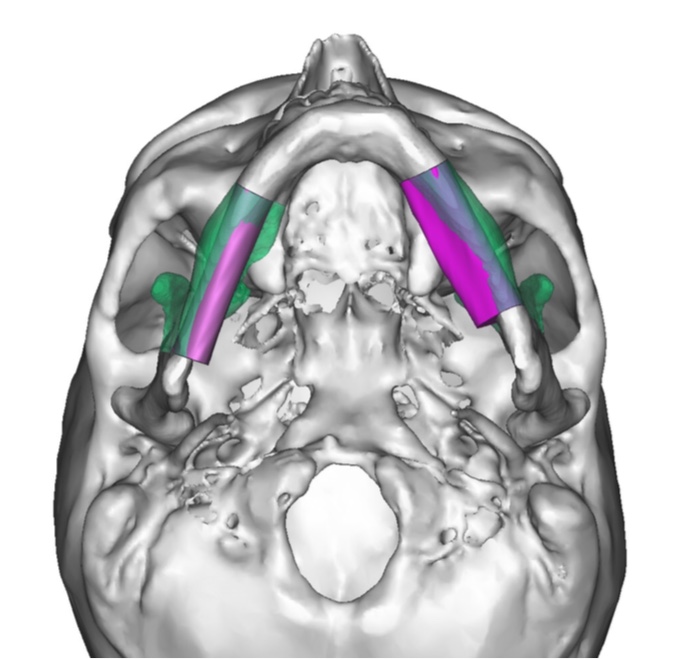
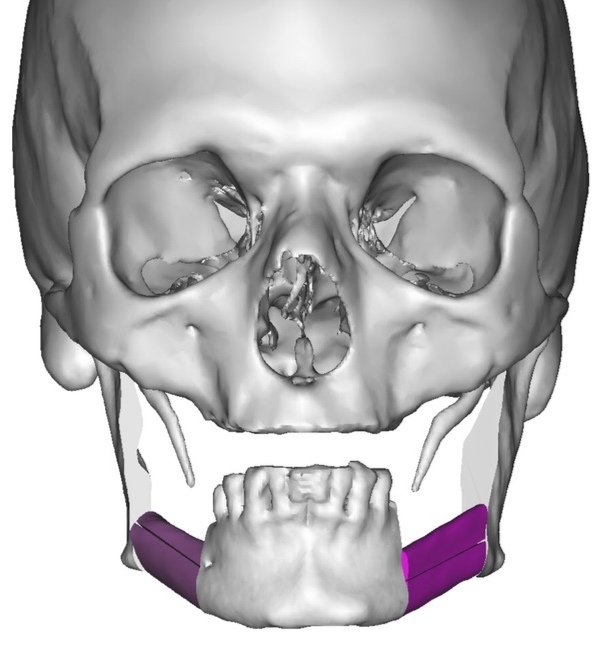
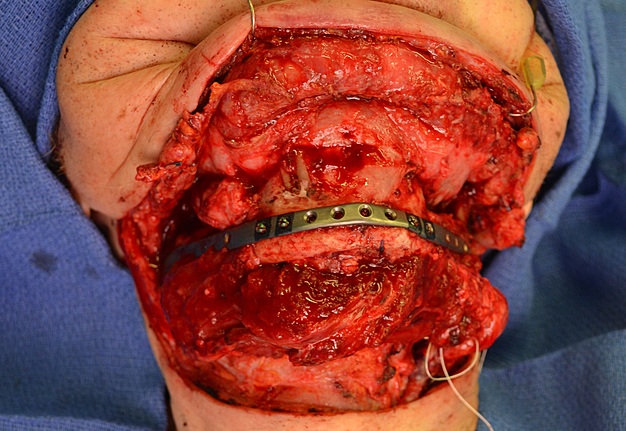
A bilateral mandibular segmental reconstruction (Fig 1) with a single fibular transplant for our patient was indicated. It’s that we did so while preserving the chin. Traditionally the chin would be removed along with the other segments and muscular attachments of the tongue and lower lip, and remaining teeth, would be lost. This would severely affect speech, swallowing and esthetics. By preserving the chin we greatly preserve form function and quality of life with near base-line esthetics.
ARGUMENTS FOR VASCULARIZED BONE GRAFTS
Bae and Waters the perfectly structured arguments for different types of grafts (Table 2) made understanding of its` benefits as easy as possible.15
FIBULA FLAP ADVANTAGES & DISADVANTAGES
Shetawi and Buchbinder based on the literature and their own experience data made a clear classification of the fibula flap advantages (Table 3) and disadvantages (Table 4) in the textbook Contemporary Oral Oncology: Oral and Maxillofacial Reconstructive Surgery under editorship of Moni Kuriakose.16
VIRTUAL SURGICAL PLANNING
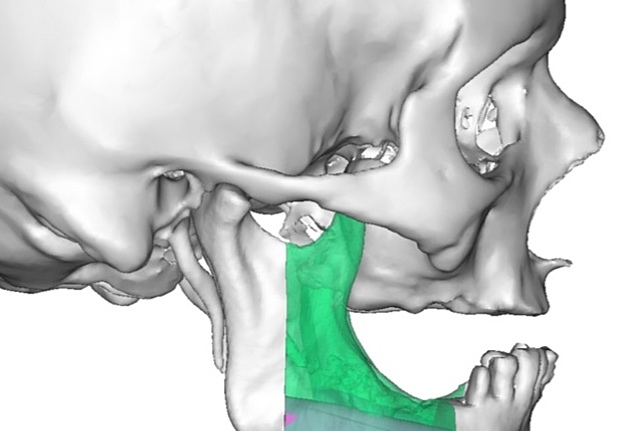
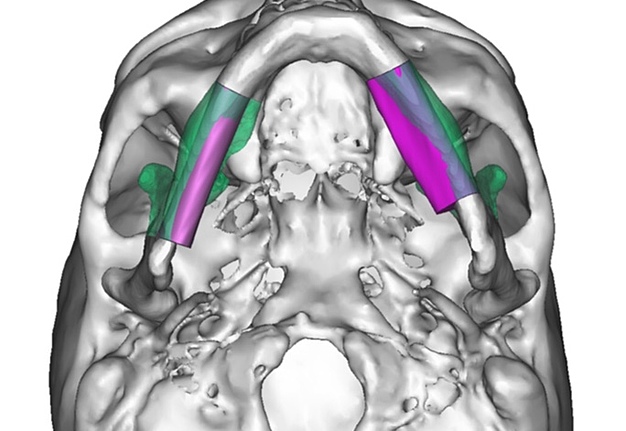
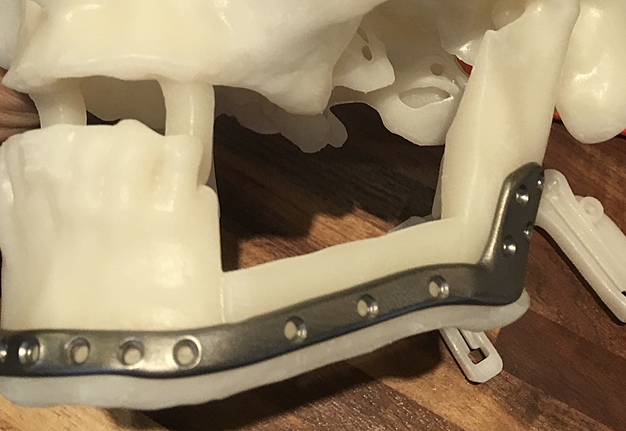
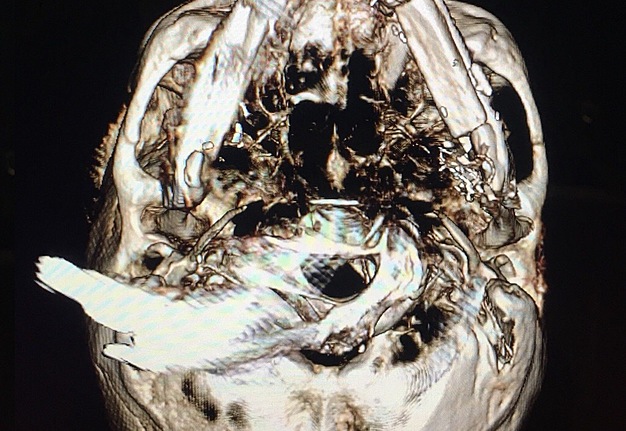
We uploaded the patient`s multislice computed tomography (CT) scans and lower limb CT angiograms to 3D Systems (Rock Hill, South Carolina, USA). The patient was planned for a bilateral mandibular osteotomy (Fig 1) – Jewer Class L bilateral defect.4, 17
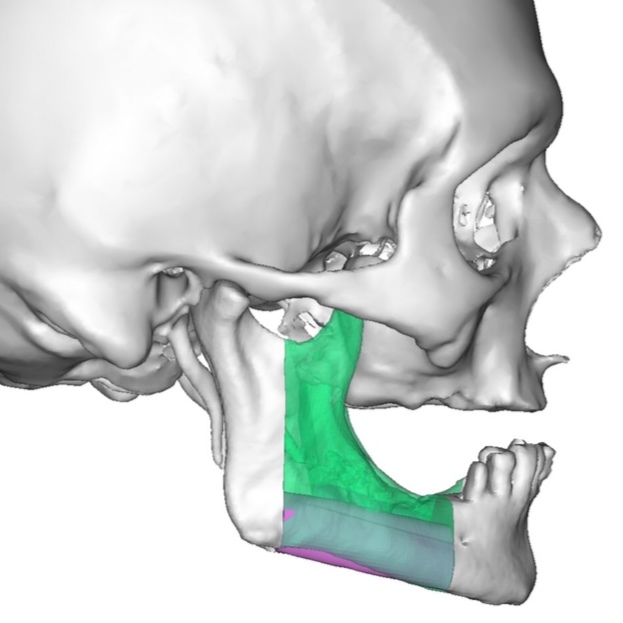
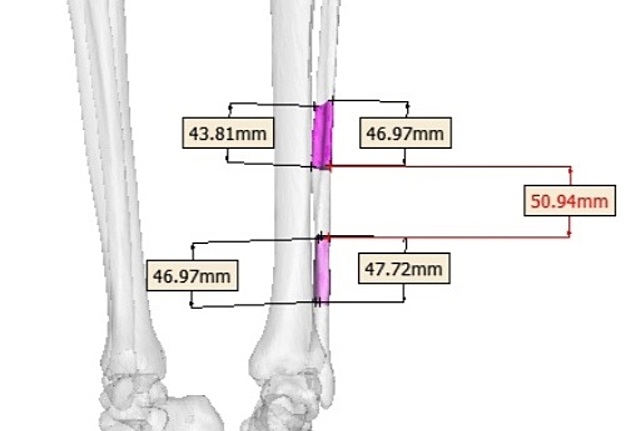
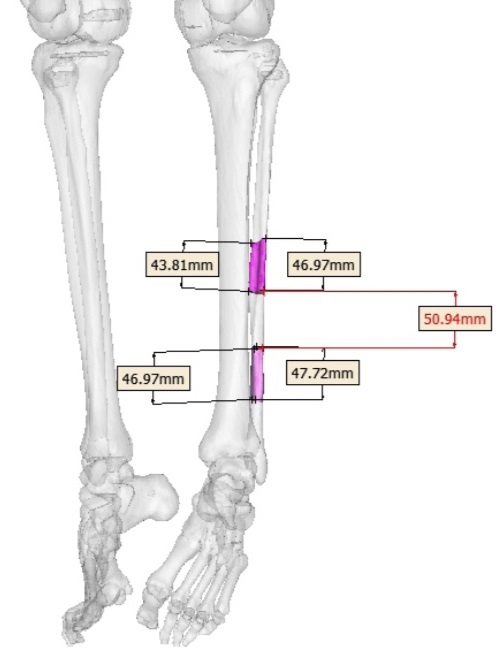
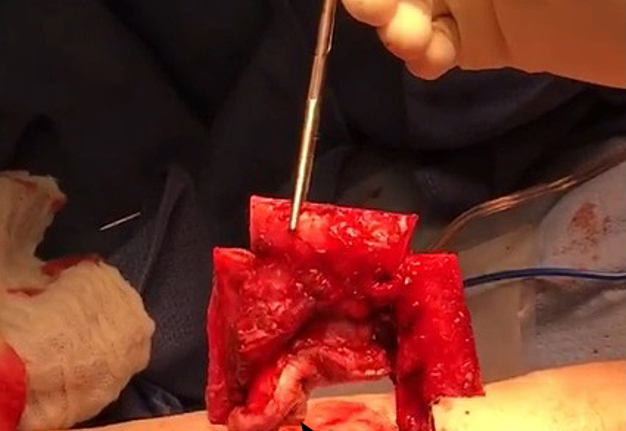
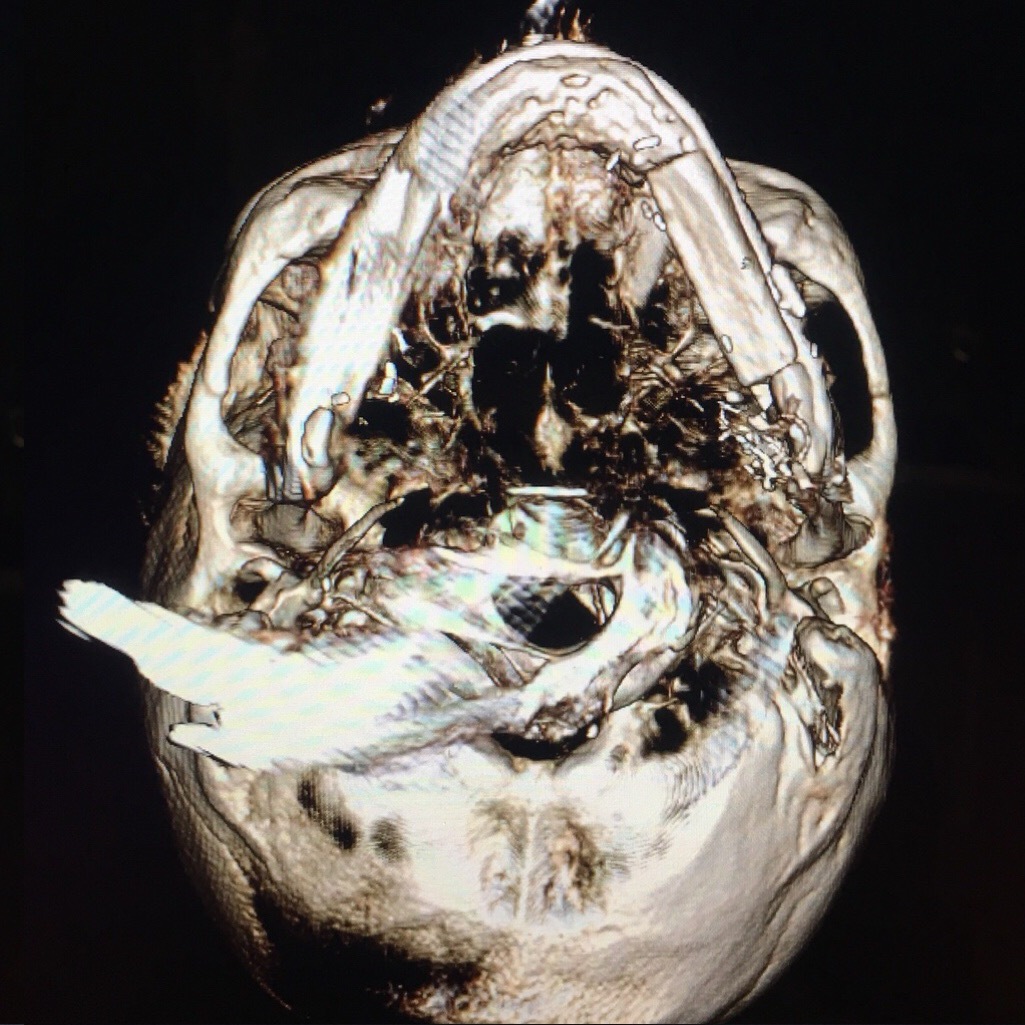
Virtual surgical planning calculated a need for total 145.63-mm left fibula bone segment (divided into 3 segments), using enough pedicle for anastomosis in the left mandibular defect. The length of fibular segments (Fig 2) was: 1) 46.97 to 47.72 mm – the lower fibula bone segment; 2) 50.94 mm – the middle segment, and 3) 43.81 to 46.97 mm – the upper fibula bone segment.
PREOPERATIVE TRACHEOTOMY: PRO & CONTRA
Lapis et al (2015) in the study “Factors in successful elimination of elective tracheotomy in mandibular reconstruction with microvascular tissue” (Table 5) reported that mandibular resection and reconstruction can be performed safely without elective tracheotomy but only in a selected group of patients.18
Statopoulus and Stassen emphasize that secure airway is critically important in the intraoperative and early postoperative period for patients undergoing head and neck cancer surgery.28 A volume of the surgery upon bilateral mandibular reconstruction is similar with head–neck cancer surgery. So, it’s extremely important to secure the airway before initiated the reconstruction`s surgical steps.
Shetawi and Buchbinder are recommending having temporary tracheostomy during 5-7 days of postoperative period with a purpose to avoid airway compromise.16
Radiation therapy in the medical history of our patient counted this factor as unfavorable according to Lapis et al classification (Table 6) of potential factors influencing the decision to eliminate elective
tracheotomy in head neck reconstruction.18 So, the reasoned decision to perform preoperative tracheotomy was done.
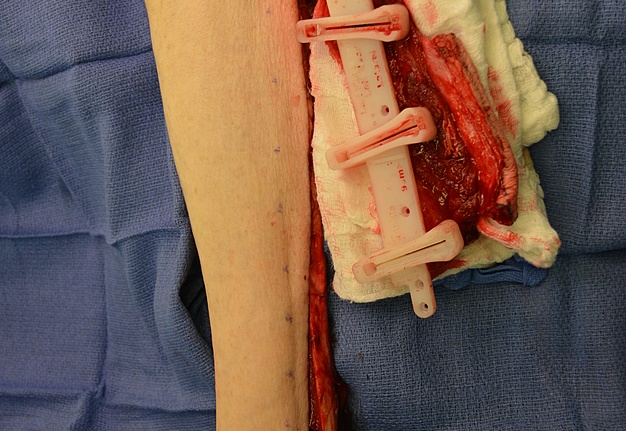
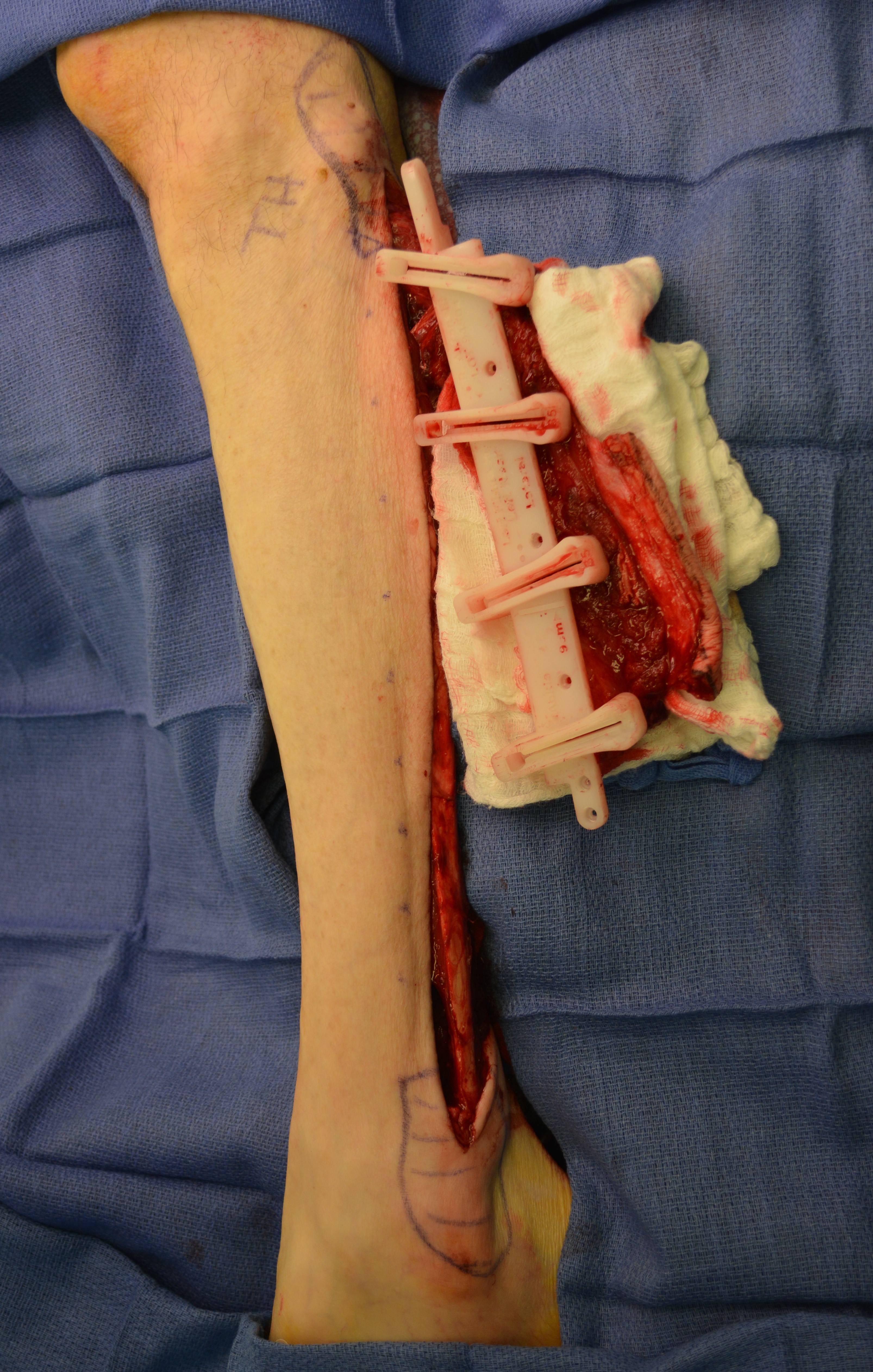
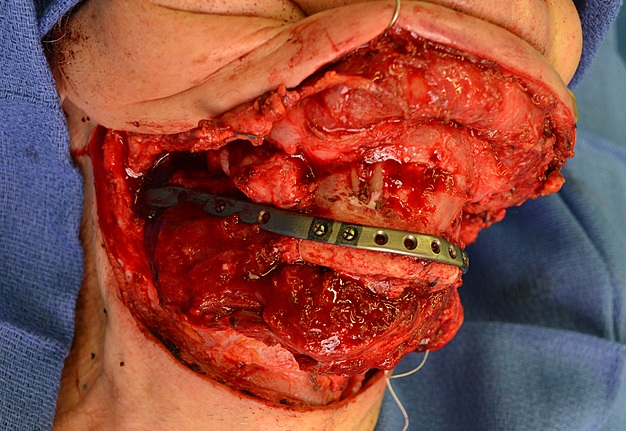
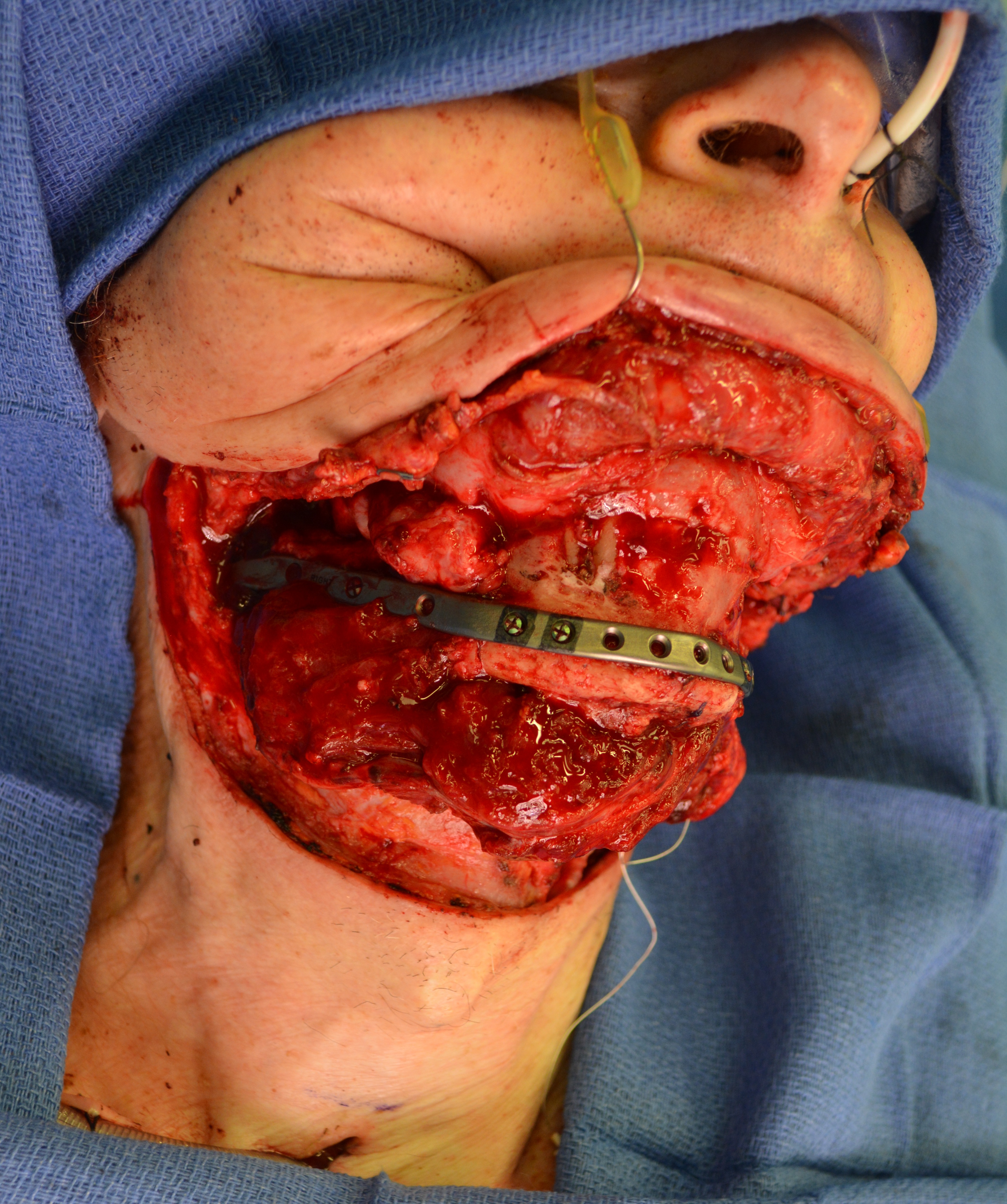
The fibula harvesting and segmental mandibular reconstruction using reconstruction plate (Fig 3) were preceded by conventional open tracheotomy, intubation, and feeding tube insertion.
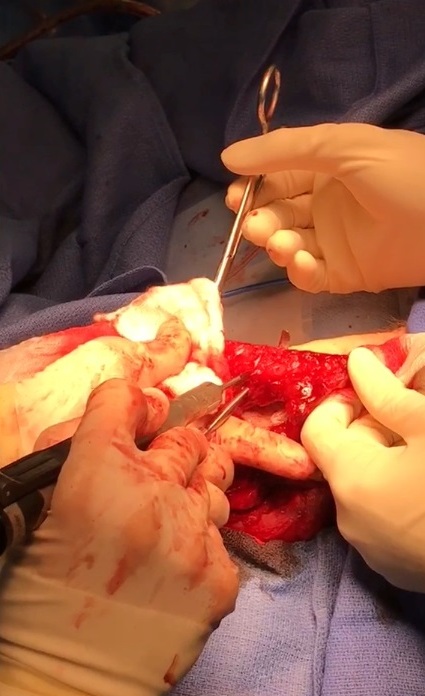
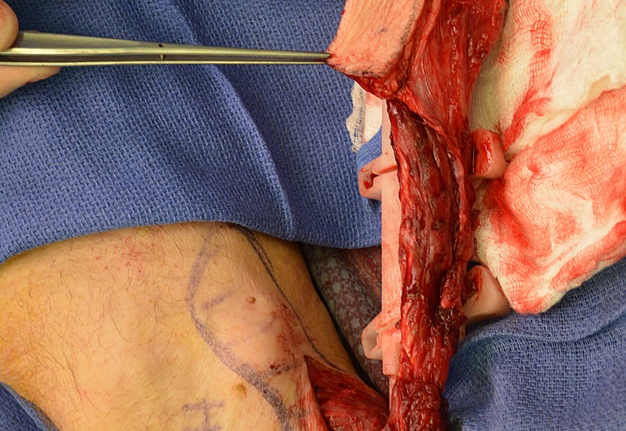
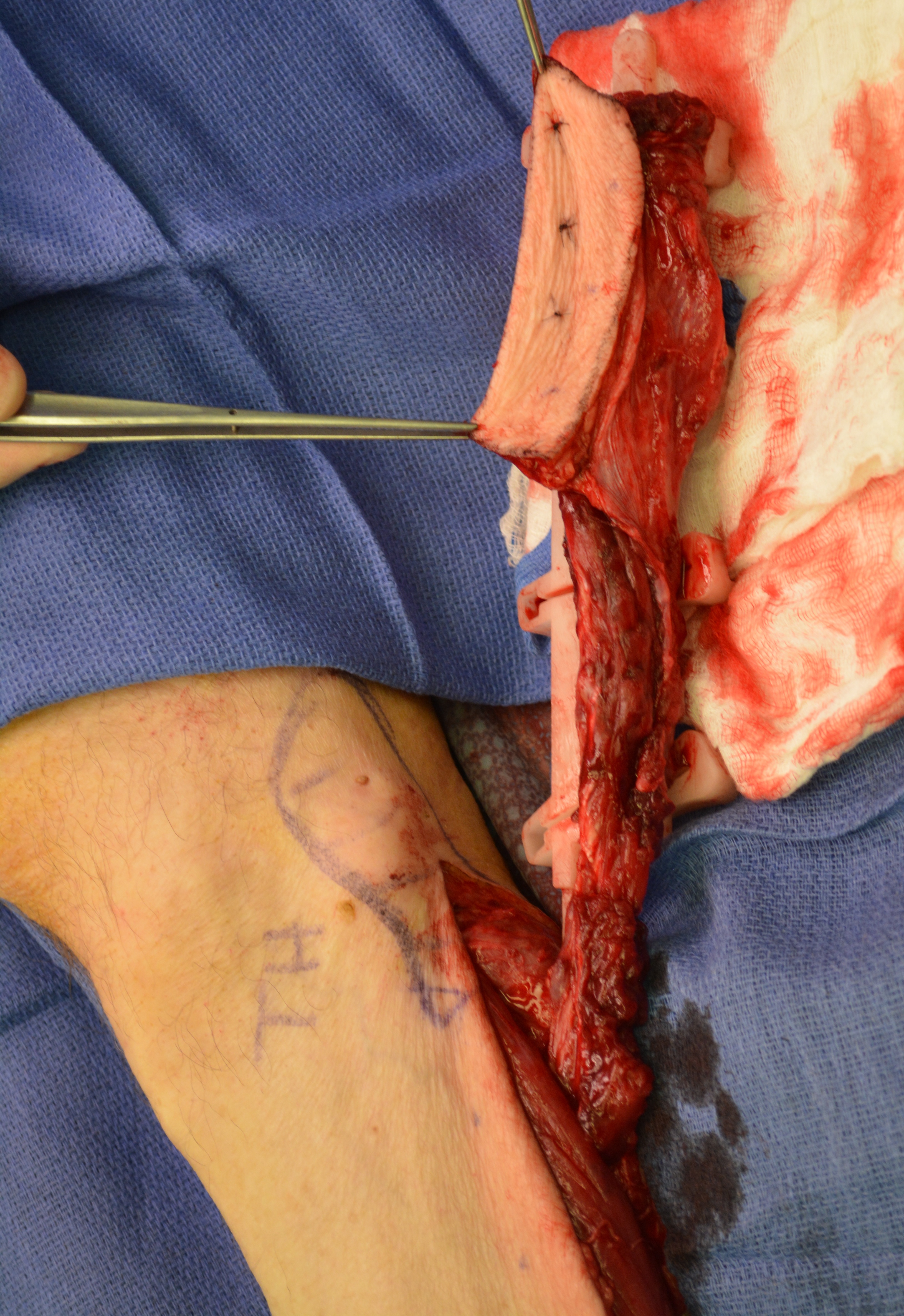
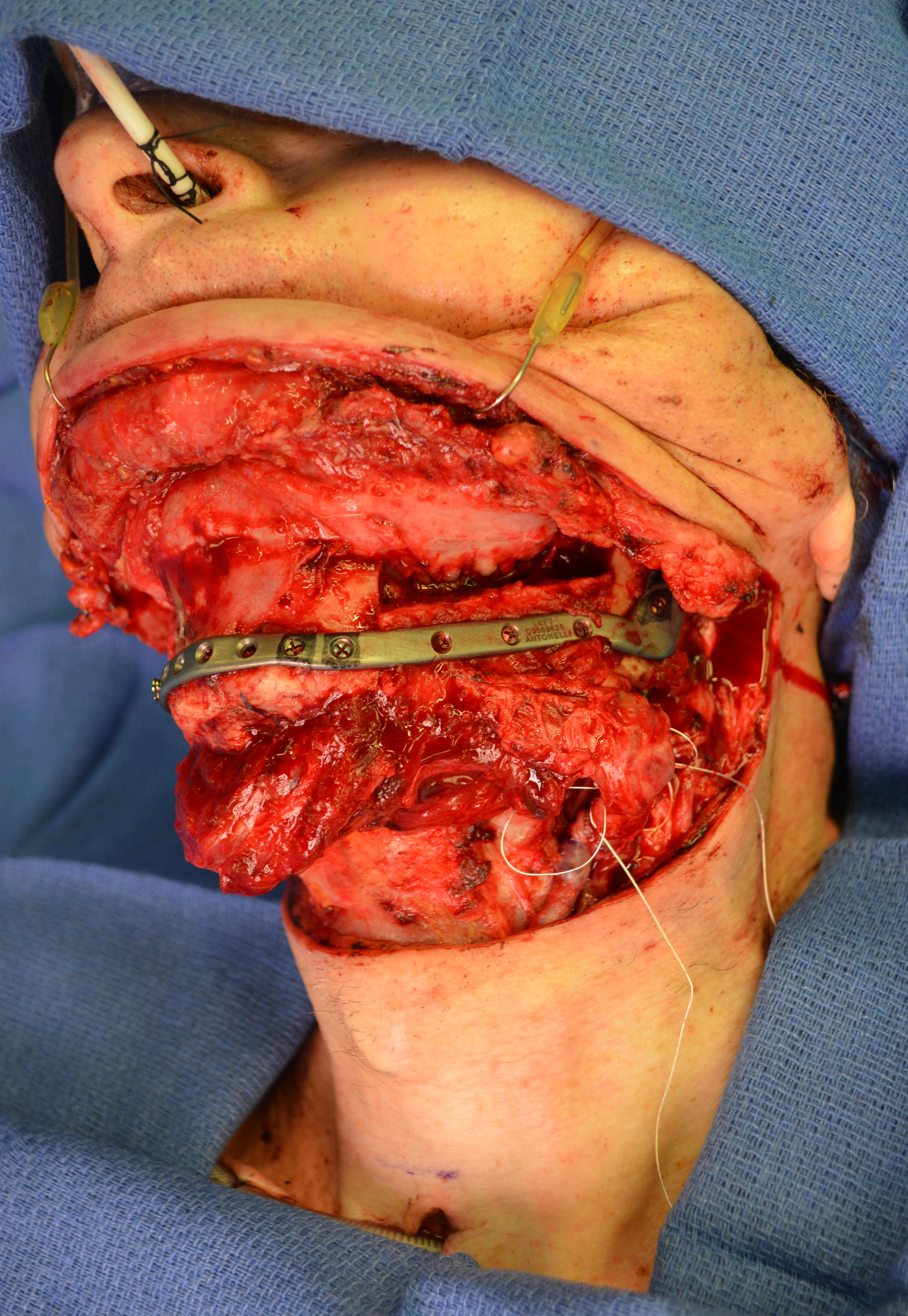
The surgery was done under general anesthesia. First, a bilateral segmental mandibular osteotomy was performed removing radiation injured bone tissue. Then, we used the fibula approach well described in the Wolff and Hölzle masterpiece Raising of Microvascular Flaps: A Systematic Approach.29 The harvesting of the fibula grafts were performed by implementing classic technique for harvesting fibula osteocutaneous transplant using CAD-CAM generated osteotomy guides (Fig 4). Video (Supplemental Video Content) demonstrates surgical stages: cutting of the fibula grafts, harvesting of the segmented grafts from left fibula. Video is available in the page of the full-text article on dtjournal.org and in the YouTube channel, available at https://youtu.be/_Tv8Cbt-HCA. Total video`s duration: 1 min 13 sec. Video includes remarks of a surgeon (Todd Hanna).
VIDEO. Supplemental Video Content demonstrates surgical stages: cutting of the fibula grafts and harvesting of the segmented grafts from left fibula. Video is available in the page of the full-text article on dtjournal.org and in the YouTube channel, available at https://youtu.be/_Tv8Cbt-HCA. Total video`s duration: 1 min 13 sec. Video includes remarks of a surgeon (Todd Hanna).
RECONSTRUCTION PLATE VERSUS MINIPLATES
Among many surgeons by 2018 there was the great number of discussions in recommendation what type of the titanium plates is better to use in cases of mandibular reconstructions. Voices from different
continents and institutions argued about superior role: 1) some of the reconstruction plate30, 31 and 2) some of the mini-plates32, 33 upon different types of defects` (Jewer et al17) mandibular reconstruction.
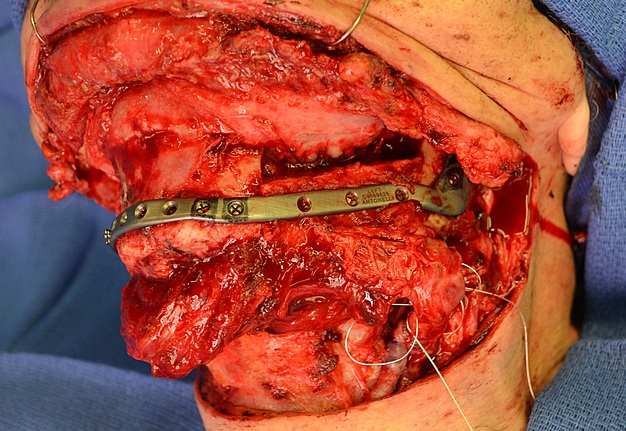
Findings of Park et al, 201834 putted a reasoned end to this question. As their precise study (8 reconstruction models with biomechanical stability analysis) support the use of a reconstruction plate for stable fixation upon mandibular reconstructions.34 The mini-plates generate substantially greater levels of stress in majority scenarios and are a less preferable option that has more percentage to fail in the long-term follow-up period.34 So, in our case we were guided by recommendations of the Korean authors.34
IMPROVING MEAN ISCHEMIA TIME
Reducing operative time is always the crucial goal upon surgical procedures. It`s become especially important in cases of using transplants. Berggren et al, 1982 in their study “The effect of prolonged ischemia time on osteocyte and osteoblast survival in composite bone grafts revascularized by microvascular anastomoses” stated that osteocytes, and the osteoblasts could completely survive up to 25 hours of ischemia.35 Despite of that fact, reducing operating time is always one of the main objectives. And reducing mean ischemia time is significantly better (up to 99 min) when using CAD/CAM comparing with conventional techniques (up to 120-180 min) (Kääriäinen et al, 2016).36
SURGICAL PROCEDURE
After resection of the radiation injured mandibular bone segments, the lateral segmental mandibular bony defects with a limited soft tissue defect were achieved. Reestablishing vascular supply to the preserved anterior mandibular segment was done by leaving the mucosal and muscular attachments (mylohyoid muscle and genioglossus muscle).
TAILORING OF THE FLAP & OSTEOTOMIES
We used a CAD-CAM generated osteotomy guides to perform a precise guided fibular wedge osteotomies. Each fibula segment should not be cut smaller than 3 cm (Schrag et al, 2006).14
SEGMENTS INSETTING
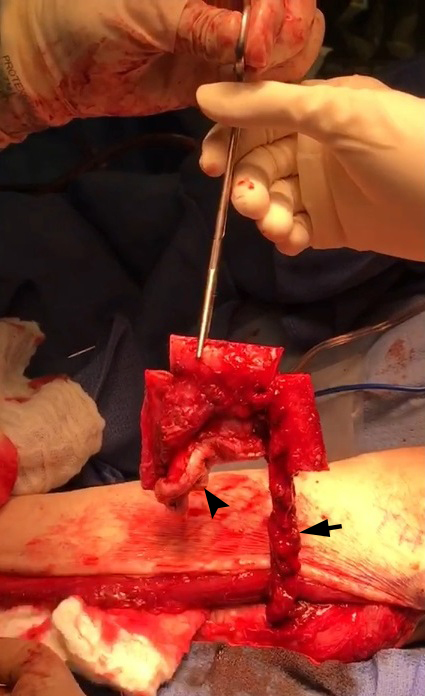
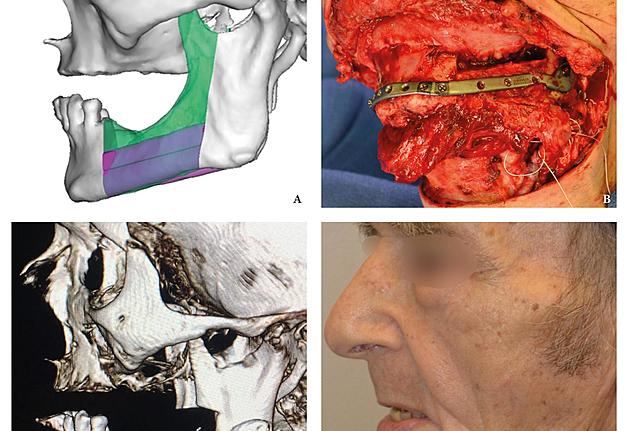
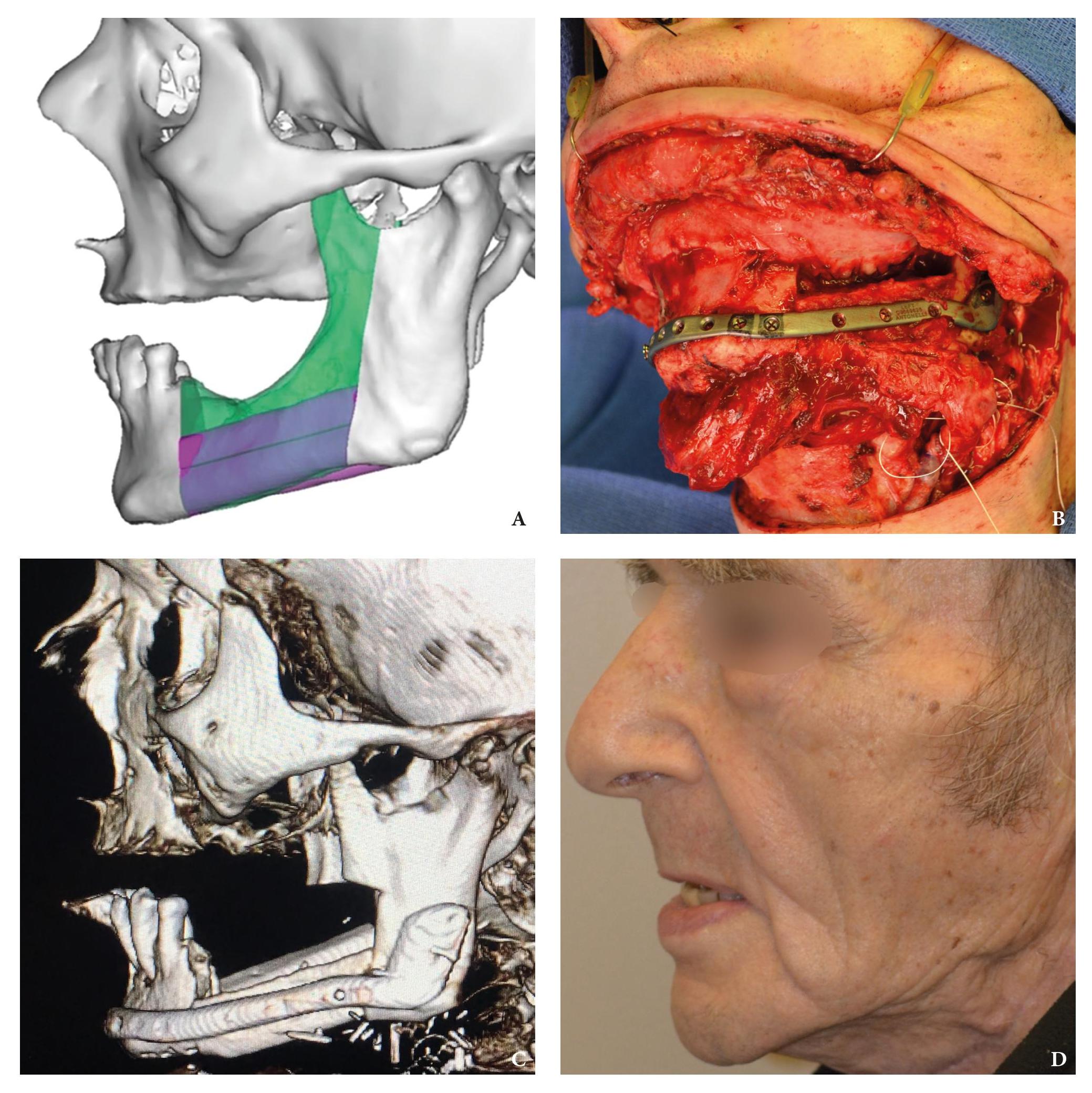
Inferior fibular bone segment was inlayed to the right-side mandibular defect (Fig 5A) and superior fibular bone segment was inlayed to the oppositeside defect (Fig 5B). The reconstruction plate was placed at the defects, along the inferior border of the both mandibular rami and symphysis (Fig 5C). Three bicortical screws were used on the right rami, 3 screws – on the left rami, and 4 screws – on the symphyseal bone fragment. But the fibula grafts were fixed to the plate using only monocortical screws to avoid vascular pedicle injury.16
RECIPIENT & DONOR VESSELS PREPARING
Shetawi and Buchbinder in the chapter Mandibular Reconstruction16 emphasize, that importance of the recipient vessel exploration cannot be ignored according to the next requirements:
1. To plan the type of free flap.
2. To plan the orientation of the flap during inset.
3. To plan the need for interpositional vein grafts.
ARTERIAL & VENOUS ANASTOMOSIS
After completing the step of insetting we start to perform next steps, making: 1) arterial anastomosis and 2) venous anastomosis. Both are performed using circumferential 9-0 or 10-0 nylon sutures. A brisk pulsatile bleeding is a right sign of a correctly performed arterial anastomosis.16 Tension or kinking is contraindicated upon laying the pedicle.
Shetawi and Buchbinder insist that it is possible to avoid hematoma formation or infections by making a proper drainage of the neck. According to the recommendation of the authors16 two different
drainage systems can be used:
- Open (Penrose) – is a soft, flexible rubber tube.
- Closed (Pratt; synonym: Jackson-Pratt) – is an internal vacuum drain connected to a grenadeshaped bulb via plastic tubing.
In our case in the postoperative period we used Penrose drainage in submental region and the Pratt bilateral suction drains (Fig 6).
BASAL & ALVEOLAR BONE RECONSTRUCTION
The fact that the fibula segments` hight is not enough to reconstruct simultaneously the basal and alveolar bone dictate us to choose one of the next techniques, which allows to restore alveolar bone hight:
- To inset fibula segment 1 cm above the mandibular inferior border.16
- Symphyseal reconstruction is a perfect area to use double-barrel method.16
- Vertical distraction is also an option to build an alveolar hight.16 But the study of Lizio et al reported that cumulative success rate of the implants inserted into distracted fibula segment at the end of follow-up was only 52%.37
- Onlay grafting.37
POSTOPERATIVE CARE FEATURES
The feeding tube is strongly recommended in the postoperative period with next purposes:16
- To ensure healing.
- To minimize breakdown of the wound and salivary leak.
PREVENTING COMPLICATIONS
Among possible complications in elderly patients the attention should be paid to delirium. This was the most common postoperative medical complication in 18 percent of cases in the report of Yang et al38
and 35.3 percent of cases in the study of Sugiura et al.39 Our successful case of BSMR proved the results (in seventy-three ≥80-year-old patients) of Sugiura et al39 who suggested that elderly patients tolerate
free fibula flap reconstruction. Despite of that, the authors stated that recovery of masticatory function looks difficult, even after performing free fibula flap reconstructive surgeries.39
OUTCOME EVALUATION
The present surgical report is comparable to state of the art cases in the literature (Hsu et al, 2011; Chen et al, 2018; Weitz et al, 2018).40, 9, 41 Postoperative control of reconstruction with 3D-CT showed a perfect position of the transplanted segments (Fig 7). A patient showed success, with excellent flap vitality, nice donor site healing and simple postoperative period despite of the age. 6-month follow-up (Fig 8) shows no signs of complications.
Thus, making the simultaneous bilateral segmental mandibular reconstruction a state of the art procedure is possible only in case of making its` every step (Fig 9) as perfect as possible according to the latest research data.
Conflict of Interest
The authors declare no conflict of interest.
Role of Co-Authors
The authors are equally contributed to that paper.
Fundings
No funding was received for this study.
References (41)
- Hidalgo DA. Fibula free flap: a new method of mandible reconstruction. Plast Reconstr Surg 1989;84:71–9. Medline | Google Scholar
- Qaisi M, Kolodney H, Swedenburg G, Chandran R, Caloss R. Fibula jaw in a day: state of the art in maxillofacial reconstruction. J Oral Maxillofac Surg 2016;74:1284.e1−1284.e15. Crossref | Medline | Google Scholar
- Su T, Fernandes RP. Microvascular reconstruction of the mandible: an argument for the fibula free flap. Rev Esp Cirug Oral Maxilofac 2014;36:1−8. Crossref
- Fernandes RP, Quimby A, Salman S. Comprehensive reconstruction of mandibular defects with free fibula flaps and endosseous implants. J Diagn Treat Oral Maxillofac Pathol 2017;1:6−10. Crossref
- Reychler H, Iriarte Ortabe J, Lambert F. Bilateral mandibular angle reconstruction with a single free vascularised fibula flap. Plast Reconstr Surg 1997;99:1411−4. Crossref | Medline | Google Scholar
- Bianchi B, Copelli C, Ferrari S, Ferri A, Sesenna E. Bilateral mandibular reconstruction with a single vascularised fibula flap. A case report. J Plast Reconstr Aesthet Surg 2008;61:1252−4. Crossref | Medline | Google Scholar
- Mello-Filho FV, Brigato RR, Eichenberger GC, Xavier SR, Mamede RC. Reconstruction of two defects with one fibular flap. Am J Otolaryngol 2008;29:218–21. Crossref | Medline | Google Scholar
- Jacobson AS, Buchbinder D, Urken ML. Reconstruction of bilateral osteoradionecrosis of the mandible using a single fibular free flap. Laryngoscope 2010;120:273–5. Crossref | Medline | Google Scholar
- Chen R, Zhang HQ, Huang ZX, Li SH, Zhang DM, Huang ZQ. Computer-assisted resection and reconstruction of bilateral osteoradionecrosis of the mandible using 2 separate flaps prepared from a single fibula. Oral Surg Oral Med Oral Pathol Oral Radiol 2018;126:102–6. Crossref | Medline | Google Scholar
- Ekanayake K, Thomas DG, Brennan PA. Reconstruction of a bilateral mandibular defect due to trauma using a single fibula free flap. J Oral Maxillofac Surg 2013;71:1724–8.
- Tymofieiev OO. Manual of maxillofacial and oral surgery [Russian]. 5th ed. Kyiv: Chervona Ruta-Turs; 2012.
- Tymofieiev OO, Tymofieiev OO. Osteoradionecrosis of the jaws: report of nineteen consecutive cases. J Diagn Treat Oral Maxillofac Pathol 2018;2:51−6.
- Chronopoulos A, Zarra T, Ehrenfeld M, Otto S. Osteoradionecrosis of the jaws: definition, epidemiology, staging and clinical and radiological findings. A concise review. Int Dent J 2018;68:22–30.
- Schrag C, Chang Y-M, Tsai C-Y, Wei F-C. Complete rehabilitation of the mandible following segmental resection. J Surg Oncol 2006;94:538–45.
- Bae DS, Waters PM. Free vascularized fibula grafting: principles, techniques, and applications in pediatric orthopaedics. www.orthojournalhms.org/ volume 8:1–4.
- Kuriakose MA. Contemporary oral oncology: oral and maxillofacial reconstructive surgery. 1st ed. Cham: Springer; 2017.
- Jewer DD, Boyd JB, Manktelow RT, Zuker RM, Rosen IB, Gullane PJ, Rotstein LE, Freeman JE. Orofacial and mandibular reconstruction with the iliac crest free flap: a review of 60 cases and a new method of classification. Plast Reconstr Surg 1989;84:391–403; discussion 404–5.
- Lapis PN, DeLacure MD, Givi B. Factors in successful elimination of elective tracheotomy in mandibular reconstruction with microvascular tissue. JAMA Otolaryngol Head Neck Surg 2016;142:46–51.
- Crosher R, Baldie C, Mitchell R. Selective use of tracheostomy in surgery for head and neck cancer: an audit. Br J Oral Maxillofac Surg 1997;35:43–5.
- Lin HS,Wang D, Fee WE, Goode RL, Terris DJ. Airway management after maxillectomy: routine tracheostomy is unnecessary. Laryngoscope 2003;113:929–32.
- Kruse-Lösler B, Langer E, Reich A, Joos U, Kleinheinz J. Score system for elective tracheotomy in major head and neck tumour surgery. Acta Anaesthesiol Scand 2005;49:654–9.
- Cameron M, Corner A, Diba A, Hankins M. Development of a tracheostomy scoring system to guide airway management after major head and neck surgery. Int J Oral Maxillofac Surg 2009;38:846–9.
- Coyle MJ, Shrimpton A, Perkins C, Fasanmade A, Godden D. First do no harm: should routine tracheostomy after oral and maxillofacial oncological operations be abandoned? Br J Oral Maxillofac Surg 2012;50:732–5.
- Brickman DS, Reh DD, Schneider DS, Bush B, Rosenthal EL, Wax MK. Airway management after maxillectomy with free flap reconstruction. Head Neck 2013;35:1061–5.
- Coyle MJ, Tyrrell R, Godden A, Hughes CW, Perkins C, Thomas S, Godden D. Replacing tracheostomy with overnight intubation to manage the airway in head and neck oncology patients: towards an improved recovery. Br J Oral Maxillofac Surg 2013;51:493–6.
- Meerwein C, Pezier TF, Beck-Schimmer B, Schmid S, Huber GF. Airway management in head and neck cancer patients undergoing microvascular free tissue transfer: delayed extubation as an alternative to routine tracheotomy. Swiss Med Wkly 2014;144:w13941.
- Moubayed SP, Barker DA, Razfar A, Nabili V, Blackwell KE. Microvascular reconstruction of segmental mandibular defects without tracheostomy. Otolaryngol Head Neck Surg 2015;152:250–4.
- Stathopoulos P, Stassen L. A modification of the Bjork flap in tracheostomies for head and neck cancer patients. J Stomatol Oral Maxillofac Surg 2018;119:444–5.
- Wolff K-D, Hölzle R. Raising of microvascular flaps: a systematic approach. 2nd ed. Cham: Springer; 2011.
- Wittwer G, Adeyemo WL, Turhani D, Ploder O. Treatment of atrophic mandibular fractures based on the degree of atrophy— experience with different plating systems: a retrospective study. J
Oral Maxillofac Surg 2006;64:230–4. - Bao T, He J, Yu C, Zhao W, Lin Y, Wang H, Liu J, Zhu H. Utilization of a pre-bent plate-positioning surgical guide system in precise mandibular reconstruction with a free fibula flap. Oral Oncol 2017;75:133–9.
- Mugino H, Takagi S, Oya R, Nakamura S, Ikemura K. Miniplate osteosynthesis of fractures of the edentulous mandible. Clin Oral Investig 2005;9:266–70.
- Bujtar P, Simonovics J, Varadi K, Sandor GK, Avery CME. The biomechanical aspects of reconstruction for segmental defects of the mandible: a finite element study to assess the optimisation of plate and screw factors. J Craniomaxillofac Surg 2014;42:855–62.
- Park SM, Lee JW, Noh G. Which plate results in better stability after segmental mandibular resection and fibula free flap reconstruction? Biomechanical analysis. Oral Surg Oral Med Oral Pathol Oral Radiol 2018;126:380–9.
- Berggren A, Weiland AJ, Dorfman H. The effect of prolonged ischemia time on osteocyte and osteoblast survival in composite bone grafts revascularized by microvascular anastomoses. Plast Reconstr Surg 1982;69:290–8.
- Kääriäinen M, Kuuskeri M, Gremoutis G, Kuokkanen H, Miettinen A, Laranne J. Utilization of threedimensional computer-aided preoperative virtual planning and manufacturing in maxillary and
mandibular reconstruction with a microvascular fibula flap. J Reconstr Microsurg 2016;32:137–41. - Lizio G, Corinaldesi G, Pieri F, Marchetti C. Problems with dental implants that were placed on vertically distracted fibular free flaps after resection: a report of six cases. Br J Oral Maxillofac Surg 2009;47:455–60.
- Yang R, Lubek JE, Dyalram D, Liu X, Ord RA. Head and neck cancer surgery in an elderly patient population: a retrospective review. Int J Oral Maxillofac Surg 2014;43:1413–7.
- Sugiura Y, Sarukawa S, Hayasaka J, Kamochi H, Noguchi T, Mori Y. Mandibular reconstruction with free fibula flaps in the elderly: a retrospective evaluation. Int J Oral Maxillofac Surg 2018;47:983–9.
- Hsu WK, Lo CH, Lee FH, Su WC, Lin TS, Pai H. The timing of tracheostomy extubation in head and neck cancer patients. J Oral Maxillofac Surg 2011;40:1069.
- Weitz J, Wolff KD, Kesting MR, Nobis CP. Development of a novel resection and cutting guide for mandibular reconstruction using free fibula flap. J Craniomaxillofac Surg 2018;46:1975–8.