Gigantic Dentigerous Cysts Associated with the Ectopic/Impacted Upper Third Molars: Computed Tomography Analysis of Nasolacrimal Duct and Osteomeatal Complex Obstructions and Review of Literature
May 29, 2020
https://doi.org/10.23999/j.dtomp.2020.5.1
J Diagn Treat Oral Maxillofac Pathol 2020;4:79−94.
Under a Creative Commons license
HOW TO CITE THIS ARTICLE
Babkina TM, Shekera OG, Storozhchuk YO, Telukha KI, Nozhenko OA, Fesenko II, Zaritska VI, Snisarevskyi PP. Gigantic dentigerous cysts associated with the ectopic/impacted upper third molars: computed tomography analysis of nasolacrimal duct and osteomeatal complex obstructions and review of literature. J Diagn Treat Oral Maxillofac Pathol 2020;4(5):79–94.
Contens: Summary | Introduction | Case 1 | Case 2 | Discussion | Conclusions | Role of co-authors | Term of consent | Fundings | Acknowledgments | References (40)
INSTITUTIONAL REPOSITORY
https://ir.kmu.edu.ua/handle/123456789/714
SUMMARY
We report the cases with giant dentigerous cysts (synonym: follicular cysts) of the maxillary sinus which caused ophthalmologic, neurologic, and nasal disturbances.
Case 1: A 44-year-old female with osteomeatal complex obstruction and severe headaches due to giant dentigerous cyst associated with impacted upper left wisdom tooth. An air-fluid level and middle turbinate compression with intact lower turbinate became the characteristic features of the case which reviewed in the publications.
Case 2: A 60-year-old woman with complete acquired nasolacrimal duct and osteomeatal complex obstruction due to gigantic dentigerous cyst.
It’s a first ever reported case when the cyst originated from ectopic upper third molar and led to the permanent left eye epiphora and left side nasal obstruction.
In both cases the consecutive pre-operative cone-beam computed tomography is presented and comparison of attenuation coefficient of the cystic content is analyzed.Management of the cases is described, surgical techniques and literature is reviewed; 1-year follow-up period is highlighted.
INTRODUCTION
Nasolacrimal duct obstruction (NLDO) is a congenital or acquired pathologic condition usually manifesting with epiphora (synonyms: tearing, watering eye) due blockage of tear outflow though the nasolacrimal duct.1 Partial and complete NLDO are distinguished.2 Among causes of NLDO are: dacryolith (synonym: lacrimal stone)2 formation, trauma, and growing neoplasms.3
Traumatic etiology of NLDO can be established after nasoorbito-ethmoidal fractures,4 medial maxillectomy,5 secondary to maxillofacial hardware placement,3 etc. Among malignant neoplasm which led to the NLDO, a undifferentiated sinonasal carcinoma was reported,6 among benign – giant radicular7 and dentigerous cysts8-12.
Moreover, a NLDO caused by a canine apex was presented.13 The main symptom of the NLDO is “epiphora” which is commonly described as a tearing or watering eye.
Dentigerous cysts (synonym: follicular cysts)14 belong to the odontogenic group of cysts in which they count 18.1 percent of cases.15 The term “dentigerous cyst” was proposed by English surgeon and pathologist James Paget in 1853 and literally means “tooth bearing cyst.”16
Its synonym “a follicular cyst” is also very popular for it explains that cystic wall arises from the follicle of a tooth that has failed to erupt.14,17 Among all number of dentigerous cyst, only 30% of them occur in the maxilla.18 From the maxillary dentigerous cyst cases the majority was noted around the impacted canines and far less had arisen from the follicles of the impacted/ectopic upper third molars, among which the bilateral cases are also reported.17
To our knowledge, 6 cases in the English language literature have described the NLDO caused by growing dentigerous cyst.8-12 But none of them reported the NLDO following growth of dentigerous cyst which originated from the ectopic upper third molar`s follicle.
So, the purpose of our paper is to highlight, compare, and analyze two cases:
1. A giant follicular cyst of the maxillary sinus in a 44-year-old female with osteomeatal complex obstruction and unusual intracystic air-fluid level.
2. A gigantic dentigerous cyst associated with ectopic upper wisdom tooth in a 60-year-old female with a complete acquired nasolacrimal
duct and osteomeatal complex obstructions and chronic left eye epiphora.
In July 2014, a 44-year-old female was referred by neurologist to the Center of Maxillofacial Surgery. The patient had a long history of headaches; and cone-beam computed tomography (CBCT)(Planmeca ProMax 3D Max, Planmeca, Finland) showed a giant dentigerous cyst associated with impacted upper left wisdom tooth (Fig 1).
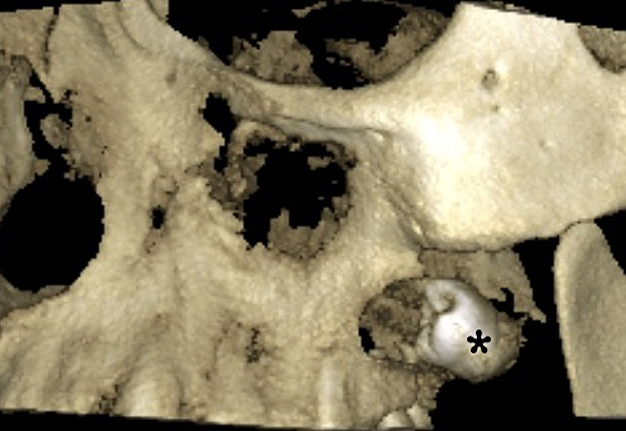
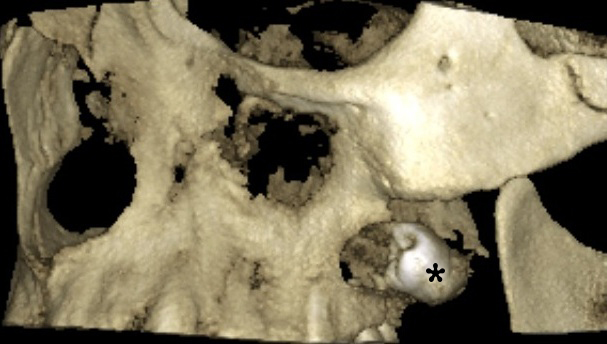
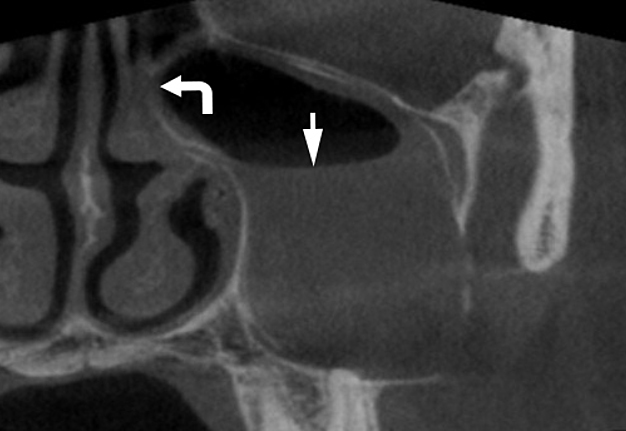
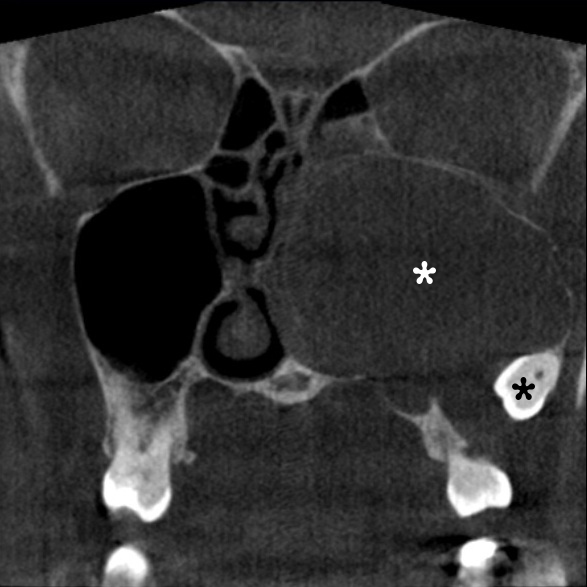
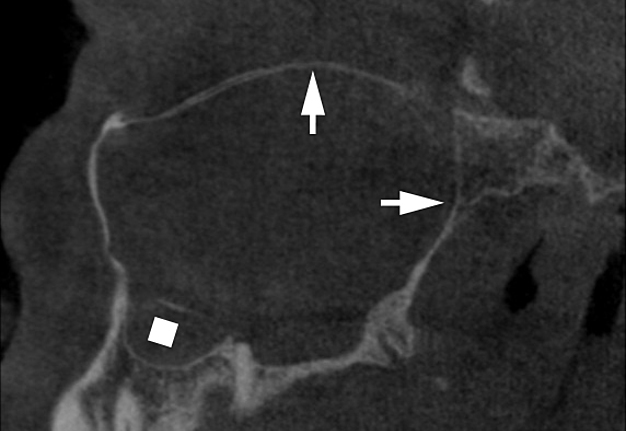
FIGURE 1A. Case 1. CBCT (A-C) of a 44-year-old female with a giant dentigerous cyst associated with impacted upper left wisdom tooth (asterisk). Notes that cyst is occupying the entire left maxillary sinus and compressed the left middle turbinate (curved arrow). Also, visualized the air-fluid level (arrow): lower and middle part of the cyst filled with a fluid content which attenuation coefficient varies from 195.2 to –20.4 HU, upper part contained air (attenuation coefficient varies from –911.8 to –790 HU). Printed with permission and copyrights retained by O.A.N.
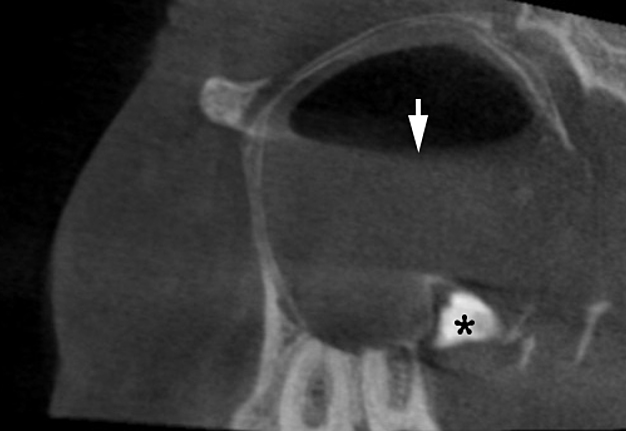
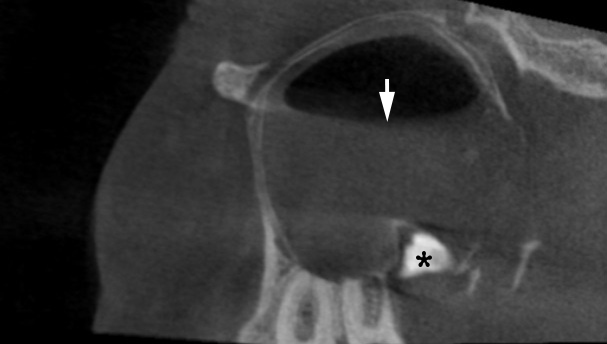
Thickness of CT slices was 0.15 mm. The cyst occupied the entire left maxillary sinus, compressed the left middle turbinate, and prolapsed to the upper left nasal meatus.
Also, the air-fluid level was visualized (Fig 1B, C): lower and middle part of the cyst was filled with a content which attenuation coefficient varies from –195.2 to –20.4 Hounsfield units (HU), upper part contained air (attenuation coefficient varies from –911.8 to –790 HU).
Attenuation coefficient measurements have been performed in 5 different areas of each type of content. In our opinion, taking into account that there was no evidence of previous intracystic infection, the presence of intracystic air component can be a result of cystic wall micro-perforation(s) in area of the left maxillary ostium.
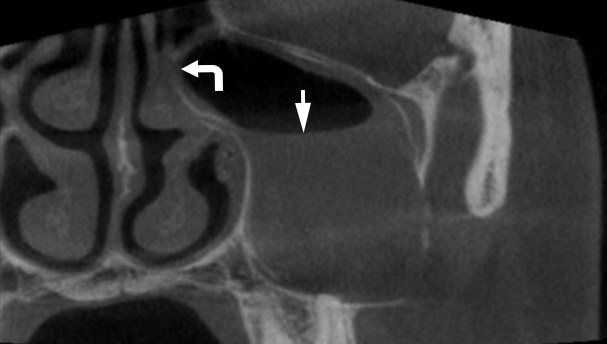
FIGURE 1B. Case 1. CBCT (A-C) of a 44-year-old female with a giant dentigerous cyst associated with impacted upper left wisdom tooth (asterisk). Notes that cyst is occupying the entire left maxillary sinus and compressed the left middle turbinate (curved arrow). Also, visualized the air-fluid level (arrow): lower and middle part of the cyst filled with a fluid content which attenuation coefficient varies from –195.2 to –20.4 HU, upper part contained air (attenuation coefficient varies from –911.8 to –790 HU). Printed with permission and copyrights retained by O.A.N.
FIGURE 1C. Case 1. CBCT (A-C) of a 44-year-old female with a giant dentigerous cyst associated with impacted upper left wisdom tooth (asterisk). Notes that cyst is occupying the entire left maxillary sinus and compressed the left middle turbinate (curved arrow). Also, visualized the air-fluid level (arrow): lower and middle part of the cyst filled with a fluid content which attenuation coefficient varies from 195.2 to –20.4 HU, upper part contained air (attenuation coefficient varies from –911.8 to –790 HU). Printed with permission and copyrights retained by O.A.N.
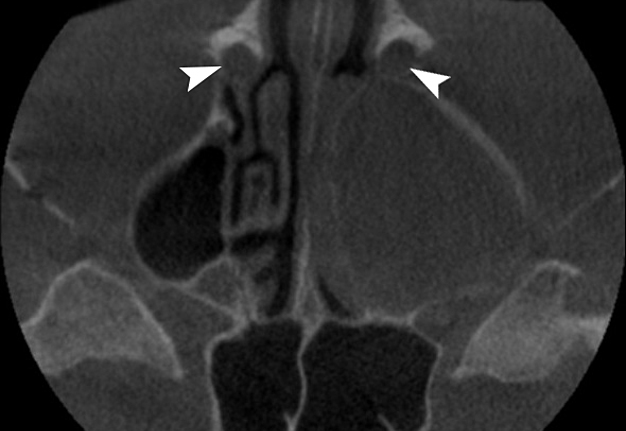
VIDEO 1 (Supplemental Video Content) shows sequence of axial CBCT scans. Slice on the 14th second of the video demonstrates the intact, opacified, oval shape nasolacrimal canals measured 0.54 × 0.31 cm (right) and 0.62 × 0.35 cm (left).
Thickness of the cystic walls varied from 0.67 to 4.37 mm; and hyperplasia (mucosal thickening reached 4.9 mm) of the Schneiderian membrane (synonyms: mucoperiosteum, maxillary sinus membrane) 19 was noted in all areas of the sinus.
Video is available in the page of the full-text article on dtjournal.org and in the YouTube channel, available at https://youtu.be/yigKLrEQMlw. Total video`s duration: 37 seconds.
VIDEO 1. Case 1. Supplemental Video Content shows sequence of axial CBCT scans. Notes intact, opacified, oval shape nasolacrimal canals (arrowheads) measured 0.54 × 0.31 cm (right) and 0.62 × 0.35 cm (left). Also, a very rare feature, an intracystic air component (asterisk) without a history of previous infection or surgery, is visualized. Thickness of the cystic walls (dot) varies from 0.67 to 4.37 mm. Quadrate labels on hyperplasia of the Schneiderian membrane. Video is available in the page of the full-text article on dtjournal.org and in the YouTube channel, available at https://youtu.be/yigKLrEQMlw. Or just point the smartphone/tablet camera at the QR code and click on the pop-up menu “Open ... in ... .” Total video`s duration: 37 seconds. Printed with permission and copyrights retained by O.A.N.
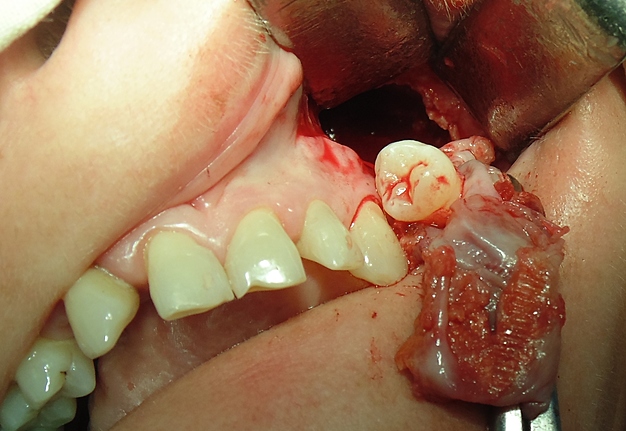
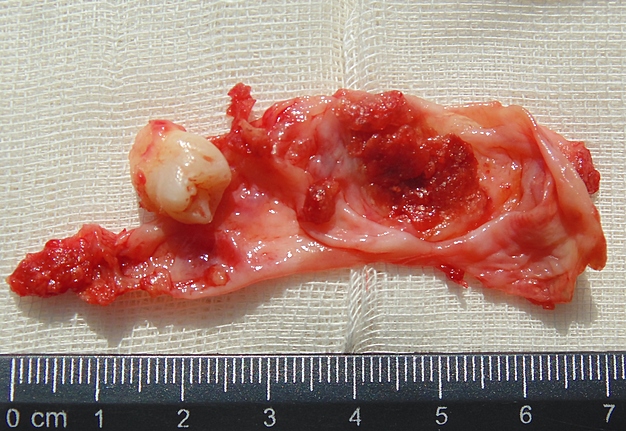
Removal of the cystic lesion with upper third molar (Fig 2A, B) was performed (Oleksandr A. Nozhenko) under nasotracheal intubation using Caldwell-Luc approach at the anterolateral aspect of the left maxillary sinus. During the enucleation of the cyst, its fluid content was evacuated.
After creation of the artificial naso-antral passage (5 × 5 mm) with the lower nasal meatus (synonyms: rhinostomy, 14 inferior meatal antrostomy 20 ) the sinus was properly irrigated.
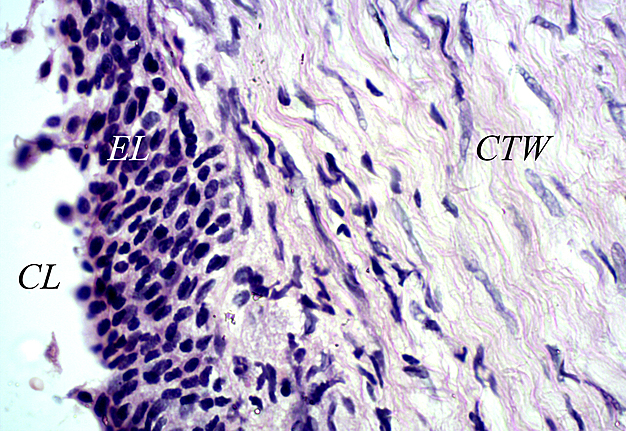
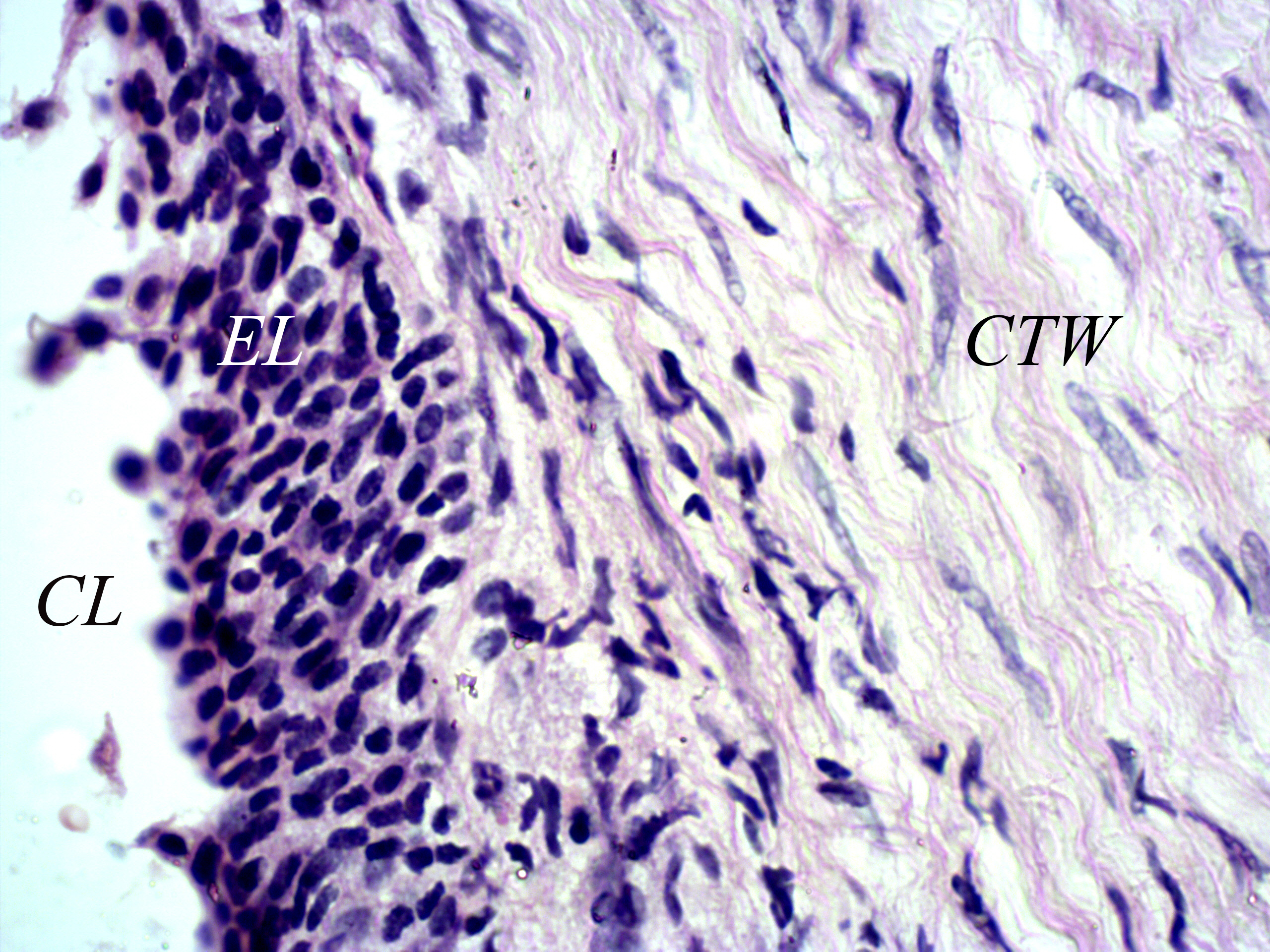
Pathohistology proved the diagnosis, revealing (Fig 2C) cystic lumen, nonkeratinized stratified squamous epithelium lining measuring three to ten cells in thickness, and connective tissue capsule (synonym: connective tissue wall 21 ). 1-year follow-up showed no data about recurrence or functional disturbances.
FIGURE 2C. Microscopic section shows cystic lumen (CL), nonkeratinized stratified squamous epithelium lining (EL) measuring three to ten cells in thickness, and connective tissue wall (CTW) (hematoxylin and eosin stain; magnification ×40). Fig 2A and B printed with permission and copyrights retained by O.A.N. Fig 2C printed with permission and copyrights retained by V.I.Z. and P.P.S.
In November 2016, a 60-year-old Caucasian woman was referred by a general dentist to the Department of Oral and Maxillofacial Surgery. The two major complaints were left nasal obstruction that has lasted for about the last few years and left eye tearing (i.e., epiphora) that has been going on for the last couple of months.
The patient initially consulted an ophthalmologist, but his drug prescriptions did not reduce the manifestations of tearing. After the CBCT (Planmeca ProMax 3D Max, Planmeca, Finland) the patient was consulted by a dentist. Thickness of CT slices was 0.2 mm.
The diagnosis of giant dentigerous cyst of the left maxillary sinus was established and female was redirected to the inpatient clinic for further surgical treatment. The patient had no comorbidities.
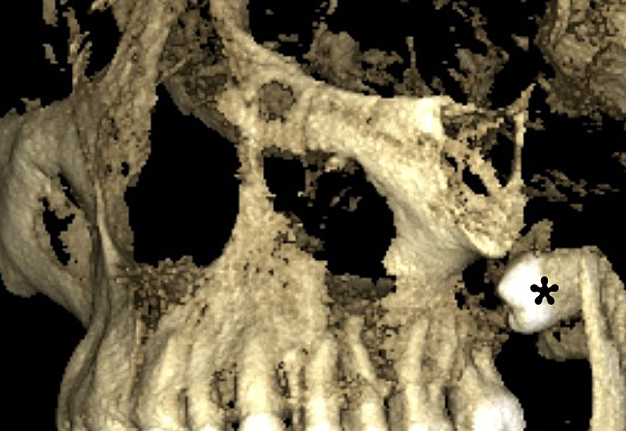
Three-dimensional CBCT showed ectopic position of the upper left third molar (Fig 3).
CBCT revealed a gigantic radiolucent unilocular cystic lesion measuring 4.18 × 3.22 cm on coronal scans (Fig 4A) and 4.2 × 3.94 cm on axial scans (Fig 4B) in the cyst`s largest dimension.
The cystic lesion filled the entire left maxillary sinus. The lesion`s content attenuation coefficient varies from –282.1 to –181.6 HU, which suggested that lesion contains fluid. No signs of intracystic aeration were noted.
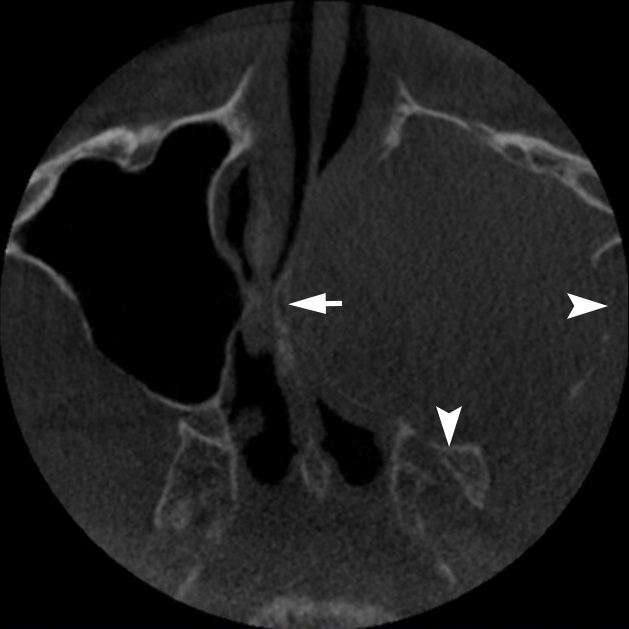
FIGURE 4B. Case 2.On axial scan the lesion measured 4.2 × 3.94 cm expanding to the level of nasal septum, deforming (arrow) and displacing it and the medial wall of the sinus to the contralateral sinus direction. Lateral and posterior wall of the left maxillary sinus were also expanded by cyst outwards (arrowheads). Printed with permission and copyrights retained by I.I.F.
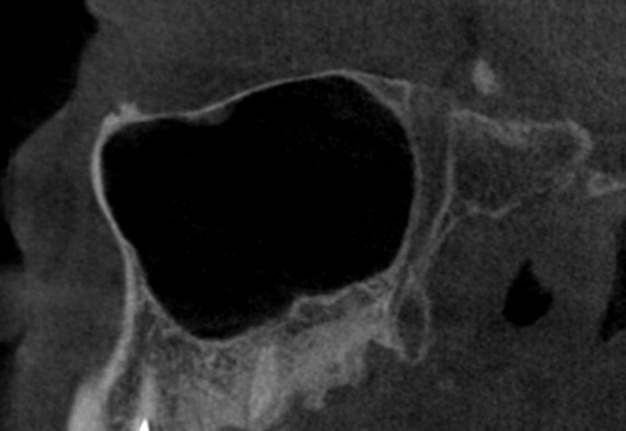
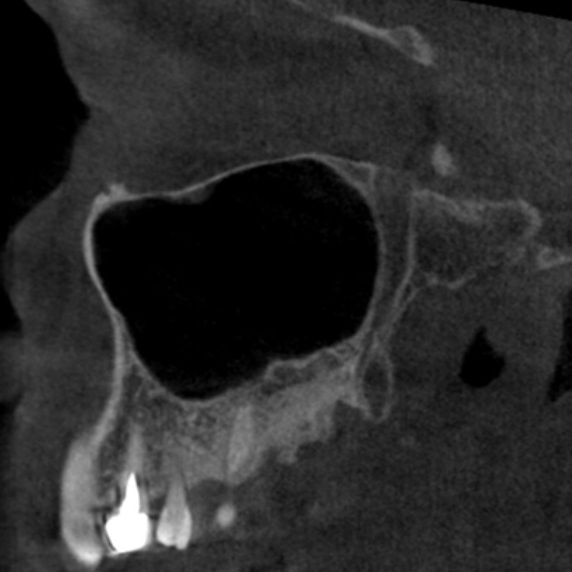
Cyst`s expansion to the level of nasal septa, its and the medial wall of the sinus deformation and displacement to the contralateral sinus direction were noted. Lateral, posterior, inferior, and superior walls of the left maxillary sinus were also expanded by the cyst outwards (Fig 5).
FIGURE 5B. Case 2. Comparison of sagittal CBCT scans of the left sinus, all walls of which are expanded by a giant dentigerous cyst. Demonstrates a significant deformation (arrows) of posterior and upper wall of the left sinus causing elevation of the orbital floor. Quadrate labels thickening of the sinus mucosa. Printed with permission and copyrights retained by I.I.F.
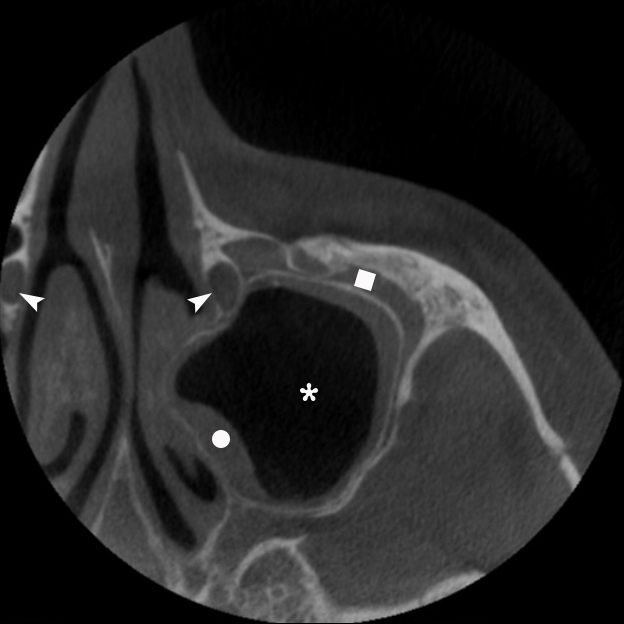
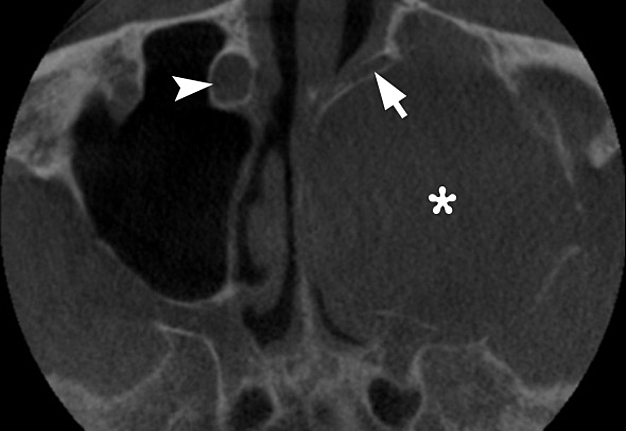
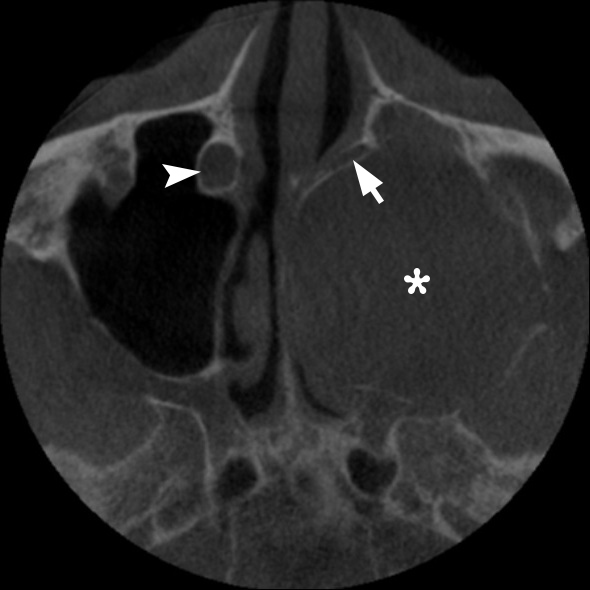
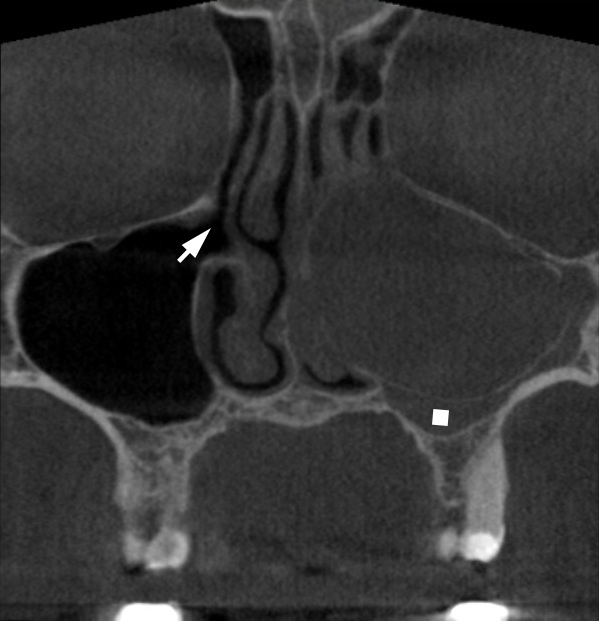
Analysis of axial CT scans along the entire length of the left nasolacrimal duct (from fossa of the lacrimal sac to the inferior nasal meatus) 22 clearly demonstrated complete compression of the bony canal with duct at the level of its middle and lower parts (VIDEO 2) (Supplemental Video Content).
An axial CT scan at the level of upper part of nasolacrimal canals demonstrated intact, opacified, 23 oval shaped nasolacrimal ducts measured 0.44 × 0.42 cm (right) and 0.52 × 0.36 (left).
Scan at the level of middle part showed complete compression of the left nasolacrimal canal with duct. A right nasolacrimal duct is still intact opacified oval shaped and measured 0.7 × 0.52 cm.
Video is available in the page of the full-text article on dtjournal.org and in the YouTube channel, available at https://youtu.be/z5TcFup312w. Total video`s duration: 45 seconds.
VIDEO 2. Case 2. Scans at the level of middle and lower parts showed complete compression of the left nasolacrimal canal with duct (arrow) by the cyst (asterisk); a right nasolacrimal duct (arrowhead) is still intact, opacified, oval shaped and measured 0.7 × 0.52 cm. Video is available in the page of the full-text article on dtjournal.org and in the YouTube channel, available at https://youtu.be/z5TcFup312w. Or just point the smartphone/tablet camera at the QR code and click on the pop-up menu “Open ... in ... .” Total video`s duration: 45 seconds. Printed with permission and copyrights retained by I.I.F.
VIDEO 3 (Supplemental Video Content) showed that left osteomeatal complex is not recognizable due to severe obstruction and deformation by the gigantic cyst. Video is available in the page of the full-text article on dtjournal.org and in the YouTube channel, available at https://youtu.be/8LgYyjh1Tok. Total video`s duration: 54 seconds.
The cystic lesion had well-defined sclerotic borders, with exception at the inferior, posterior, and lateral walls of the sinus.
The purpose of the surgery was not only to remove the giant cystic lesion with ectopic molar but also to reestablish tear flow3 inside the entire length of left nasolacrimal duct. This aim required from a surgeon (Ievgen I. Fesenko) to remove
carefully not only the expanded “own” cortical bone around the cystic wall but also a lateral part of a compressed bony nasolacrimal canal.24
Because leaving of that thin bony layers will gave no possibility to decompress the left nasolacrimal duct. Also, the attention should be paid to careful enucleation of the cyst at the orbital floor level.
The cystic lesion had well-defined sclerotic borders, with exception at the inferior, posterior, and lateral walls of the sinus.
The purpose of the surgery was not only to remove the giant cystic lesion with ectopic molar but also to reestablish tear flow 3 inside the entire length of left nasolacrimal duct.
This aim required from a surgeon (Ievgen I. Fesenko) to remove carefully not only the expanded “own” cortical bone around the cystic wall but also a lateral part of a compressed bony nasolacrimal canal. 24
Because leaving of that thin bony layers will gave no possibility to decompress the left nasolacrimal duct. Also, the attention should be paid to careful enucleation of the cyst at the orbital floor level.
Additionally, the CT proved the compression of the left greater palatal canal by a cyst what made impossible to use that route for maxillary nerve block (synonym: palatine route of pterygopalatine anesthesia) 25 during the surgery.
A surgery was done under local anesthesia (maxillary nerve block using tuberal route, infraorbital nerve block, and infiltration anesthesia) and sedation.
Caldwell-Luc approach was created at the anterolateral wall of the maxillary sinus after performing combined incision, horizontal vestibular anteriorly and crestal posteriorly. Avoiding ectopic molar migration, it was removed in a first stage. And the cyst with expanded cortical bone was removed in a second stage (Fig 6).
Brown color liquid flowed out of the cystic cavity and was aspirated. Histopathological report confirmed the diagnosis of dentigerous cyst. The recovery period was uncomplicated. Two weeks after surgery the patient noted no signs of left eye epiphora.
VIDEO 3. Case 2. Supplemental Video Content shows coronal CT scans. Right osteomeatal complex shows no signs of obstruction. Right maxillary sinus ostium is labeled by arrow. Left osteomeatal complex is not recognizable due to severe obstruction and deformation by a gigantic cyst. Thickening of Schneiderian membrane labeled by quadrate. Video is available in the page of the full-text article on dtjournal.org and in the YouTube channel, available at https://youtu.be/8LgYyjh1Tok. Or just point the smartphone/tablet camera at the QR code and click on the pop-up menu “Open ... in ... .” Total video`s duration: 54 seconds. Printed with permission and copyrights retained by I.I.F.
Comparison of the dentigerous cysts in patient 1 and 2 is highlighted in the Table 1.
DISCUSSION
Osteomeatal complex (synonym: ostiomeatal complex) 26 obstruction is a common complication of different pathologic conditions in maxillary sinus.
After scrupulous analysis of English literature, the combination of nasolacrimal duct and osteomeatal complex obstructions due to gigantic dentigerous cyst was found in 5 studies (Table 2) with 6 cases. 8-12
But in none of those cases a dentigerous cyst associated with upper impacted/ectopic third molar was presented. Study of Emanuelli et al 27 is also more than worth of attention. Despite the fact that CT data in their case shows giant dentigerous cyst of the maxillary sinus associated with ectopic upper third molar there was no mentions about epiphora. 27
Case 1 and 2 clearly support the opinion of Salman that coronal CT scans are the best to visualize and assess the osteomeatal complex and its obstruction/narrowing by the lesions. 20 But for the verification of nasolacrimal duct obstruction, among coronal and axial CT scans, according to сases 1 and 2, the axial ones are the most informative due to the oblique anatomy of the duct.
Nasolacrimal duct (NLD) (synonym: lacrimal duct) 19 is a bilateral tube-shape structure inside the nasolacrimal canal, which passes from lacrimal fossa down and opens in inferior nasal meatus. Along the canals` passage they are neighboring with maxillary sinuses (synonym: Highmore's antrums) 28 and are separated from it by just a very thin layer of bone (~0.67 mm in case 1 and ~0.79 mm in case 2).
TABLE 1. Comparison of Patient 1 and 2 with the Giant Dentigerous Cysts of the Maxillary Sinus.
| Features | Case 1 | Case 2 |
| Patient`s age/gender | 44/F | 60/F |
| Associated tooth | Impacted upper left third molar | Ectopic upper left third molar |
| Epiphora | No | Yes |
| Headaches | Yes | No |
| Chronic nasal obstruction | Yes | Yes |
| Size of the cyst in the cyst`s largest dimension on axial CT scans | 2.8 × 2.9 cm | 4.2 × 3.94 cm |
| Size of the cyst in the cyst`s largest dimension on coronal CT scans | 2.82 × 3.15 cm | 4.18 × 3.22 cm |
| Maximal thickness of the sinus membrane | 4.52 mm | 7.64 mm |
|
Does thickened mucosa fill the entire space between the sinus walls and the sclerotic border of the cyst? |
Yes | Yes |
| Osteomeatal complex obstruction | Yes | Yes |
| Appearance of nasolacrimal ducts at CT | Opacified | Opacified |
| Nasolacrimal duct obstruction | No | Yes |
| Presence of intracystic air-fluid level or partial aeration | Air-fluid level | No |
| Thickness of the cystic walls | Varies from 0.67 to 4.37 mm. | The cyst wall was not defined |
| Variation of attenuation coefficient of the cystic wall, Hounsfield units (HU) |
From –165.1 to 32.74 HU | The cyst wall was not defined |
| Variation of attenuation coefficient of the intracystic fluid component, Hounsfield units (HU) | From –195.2 to –20.4 HU | From –282.1 to –181.6 HU |
| Variation of attenuation coefficient of the intracystic air component, Hounsfield units (HU) | From –911.8 to –790 HU | No CT signs of the air component |
TABLE 2. Articles Describing the Nasolacrimal Duct Obstruction Due to Compression by Dentigerous Cyst.
| # | Tooth`s Crown Associated with Cyst |
Clinical/ Radiological Signs of Osteomeatal Complex Obstruction |
No. of Patients | Age(yr)/Gender | Year of Publication and Title of the Article |
| 1 | Ectopic right canine | Yes | 1 | 41/M | (1997) A case of a large dentigerous cyst containing a canine tooth in the maxillary antrum leading to epiphora. 8 |
| 2 | Ectopic right deciduous canine | Yes | 1 | 3/F | (2000) Nasolacrimal duct obstruction secondary to ectopic teeth. 9 |
| 2 | Right canine | Yes | 1 | 32/F | (2000) Nasolacrimal duct obstruction secondary to ectopic teeth. 9 |
| 3 | Yes | 1 | 23/M | (2003) Dentigerous cyst in the maxillary sinus: A rare cause of nasolacrimal obstruction. 10 |
|
| 4 | Yes | 1 | 11/M | (2009) A rare cause of nasolacrimal duct obstruction: dentigerous cyst in the maxillary sinus. 11 |
|
| 5 | Yes | 1 | 21/M | (2012) A case of an extensive dentigerous cyst in the maxillary sinus leading to epiphora and nasal obstruction. 12 |
|
| 6 | Yes | 1 | 60/F | (2020) Case 2 in our study “Gigantic dentigerous cysts associated with the ectopic/impacted upper third molars: Computed tomography analysis of nasolacrimal duct and osteomeatal complex obstructions and review of literature.” |
The data analysis by Czyz et al 23 revealed that patient`s position affects the appearance of nasolacrimal duct at CT.
In 70 percent of CT investigations the NLD is opacified and in 30% of cases is aerated (fully/partially). 23
Also, in every particular patient the NLD can be opacified and aerated from different sides. 23
In case 1 and 2 the patient was in an upright position upon CBCT. In both cases nasolacrimal ducts were opacified. The fact that left eye epiphora disappeared two weeks after surgery indicates that surgical technique focused on decompression of the NLD proved its effectiveness and can be recommended in similar cases.
Discussing ectopic position of the wisdom tooth in patient 2 we support the opinion of Sivolella et al 17 that “when dentigerous cysts surround impacted teeth, they often displace the teeth into ectopic positions; ectopic teeth in the maxilla may be displaced into the maxillary sinus.”
Firstly, because we can hypothesize that the left wisdom tooth in case 2 initially was in impacted position and after cyst`s growth it became an ectopic tooth. Secondly, its ectopic position in the maxillary sinus is explained by the cystic growth to the gigantic size in the maxillary antrum.
Presence of intracystic air-fluid level in case 1 is completely unusual and very unique feature for the dentigerous cysts. Intrasinus air-fluid level is a common sign for: 1) acute purulent sinusitis and position of air-fluid level in the sinus depends on the patient`s position (vertical or horizontal) 14,29 and 2) blood after trauma or in patients with bleeding disorders 30 .
On CT images the collected blood is denser than inflammatory exudate or mucosal edema. 31 İmamoğlu et al 32 presented intracystic air densities suggesting infection within the dentigerous cyst. In their case the air is visualized as small solitary inclusions within fluid content and with no signs of air-fluid level. 31
Sclerotic well-defined borders of the cysts were noted on CT in both our cases but in areas of close contact between walls 33 of the maxillary sinus and sclerotic bony border of the cyst they were undistinguished due to their compression.
Contrast enhancement can be seen in the cyst wall only upon contrast enhanced multi-slice CT. 34 In the study of Zerrin et al 35 , cyst wall contrast was seen in 5 of the 9 cases. In our cases cyst`s walls are visualized on CT images in upper portion of the cyst only in case 1 due to the significant intracystic aeration. In middle and lower cyst`s portion of case 1 the walls were similarly undistinguished as in the entire cyst of case 2.
Mucosal lining of maxillary sinus is considered to be normal when is less than 4 mm. 29 It`s notable that in both cases (1 and 2) thickened mucosa filled the entire space between the sinus walls and the sclerotic border of the cysts. In case 1 maximal thickness of the Schneiderian membrane reached 4.52 mm and in case 2 – reached 7.64 mm without even minimal signs of intrasinus aeration.
Reported case of squamous cell carcinoma arisen in a mandibular dentigerous cyst in 72-year-old male 21 evidenced us for a need to remove the dentigerous cysts as soon as possible avoiding not only the functional disturbances in the area of maxillary sinus but also a possible malignization.
That is why we must carefully select a cyst marsupialization, as one of the internationally proposed types of surgery, in a very limited amount of cases. Caldwell-Luc operation is still one of the leading types of surgery in case of giant follicular cysts of the sinus. The endoscopic-assisted removal of the cyst and associated tooth has not only a variety of modifications 27,36,37 but also its performance has some limitations.
Case of Emanuelli et al 27 showed that it can be problematic, during the endoscopic surgery, to remove lateral sclerotic wall of the cyst. Two cases of Bernardi et al 38 successfully implemented both microscopic and endoscopic support for the traditional Caldwell-Luc surgery.
Thus, cystic expansion into the nasal cavity, the pterygo-maxillary area, the ethmoidal and the orbital regions can cause morphological, functional, nervous and inflammatory complications. 38
Among 6 published cases with nasolacrimal duct obstruction caused by dentigerous cysts, in 4 cases the cysts originated from canines, in one case was not established the tooth number which was turned by the crown into the cavity of the cyst, and in another one the dentigerous cyst has arisen around the supernumerary tooth. 8-12
In contrast to the cysts on the mandible where they grow mesio-distally, 39 on the maxilla they easily prolapsed into maxillary sinus where they can asymptomatically reach gigantic sizes. Similarly to other studies focused on unique CT characteristics of jaw cysts, 40 in our cases the CBCT also proved its effectiveness in diagnosis and planning of the surgeries.
CONCLUSIONS
Summarizing, our first case represents a unique CT appearance of intracystic air-fluid level which is completely unusual for dentigerous cyst. Second case describes a first ever reported case of permanent acquired nasolacrimal duct obstruction due to compression by gigantic dentigerous cyst associated with upper third molar in an ectopic position at the moment of preoperative CT. Despite the fact that in both cases osteomeatal complex obstruction complicated the situations, the removal (with compressed lateral wall of the NLD) of giant lesions of the maxillary sinus via classic Caldwell-Luc approach allowed as well to resolve all functional disturbances successfully.
ROLE OF CO-AUTHORS
Tetiana M. Babkina (editing).
Oleg G. Shekera (editing).
Yulia O. Storozhchuk (writing and editing).
Kyrylo I. Telukha (editing).
Oleksandr A. Nozhenko (concept of the article, material collection, writing, and editing).
Ievgen I. Fesenko (material collection and writing).
Valentyna I. Zaritska (material collection and writing).
Pavlo P. Snisarevskyi (material collection).
All authors read and approved the final manuscript.
TERM OF CONSENT
No needed.
FUNDINGS
No funding was received for this study.
ACKNOWLEDGMENTS
None.
REFERENCES (40)
-
Shen GL, Ng JD, Ma XP. Etiology, diagnosis, management and outcomes of epiphora referrals to an oculoplastic practice. Int J Ophthalmol 2016;9(12):1751–5. Crossref | Medline | Google Scholar
-
Yazici B, Hammad AM, Meyer DR. Lacrimal sac dacryoliths: predictive factors and clinical characteristics. Ophthalmology 2001;108(7):130812. Crossref | Medline | Google Scholar
-
Kang JM, Kalin-Hajdu E, Idowu OO, Vagefi MR, Kersten RC. Nasolacrimal obstruction following the placement of maxillofacial hardware. Craniomaxillofac Trauma Reconstr 2020;13(1):327. Crossref | Medline | Google Scholar
-
Ali MJ, Gupta H, Honavar SG, Naik MN. Acquired nasolacrimal duct obstructions secondary to naso-orbito-ethmoidal fractures: patterns and outcomes. Ophthalmic Plast Reconstr Surg 2012;28(4):242–45. Crossref | Medline | Google Scholar
-
Glatt HJ, Chan AC. Lacrimal obstruction after medial maxillectomy. Ophthalmic Surg 1991;22(12):757–8.
-
Liang BCC, Chau Y, Lam DSC, Chan NR. Undifferentiated sinonasal carcinoma with nasolacrimal duct obstruction. Arch Ophthalmol 2004;122(2):290–3. Crossref | Medline | Google Scholar
-
Baer ST, Drysdale A, Moore-Gillon V. Giant radicular cyst in the maxillary antrum presenting with chronic epiphora. J Laryngol Otol 1988;102(4):365–7.
-
Altas E, Karasen RM, Yilmaz AB, Aktan B, Kocer I, Erman Z. A case of a large dentigerous cyst containing a canine tooth in the maxillary antrum leading to epiphora. J Laryngol Otol 1997;111:641–3.
-
Alexandrakis G, Hubbell RN, Aitken PA. Nasolacrimal duct obstruction secondary to ectopic teeth. Ophthalmology 2000;107:189e–92e.
-
Bajaj MS, Mahindrakar A, Pushker N, Balasubramanya R. Dentigerous cyst in the maxillary sinus: a rare cause of nasolacrimal obstruction. Orbit 2003;22(4):28992. Crossref | Medline | Google Scholar
-
Ray B, Bandyopadhyay SN, Das D, Adhikary B. A rare cause of nasolacrimal duct obstruction: dentigerous cyst in the maxillary sinus. Indian J Ophthalmol 2009;57(6):4657. Crossref | Medline | Google Scholar
-
Akyol UK, Salman IA. A case of an extensive dentigerous cyst in the maxillary sinus leading to epiphora and nasal obstruction. J Emerg Med 2012;43(6):1004–7.
Crossref | Medline | Google Scholar -
Giordano Resti A, Bertazzoni G, Trimarchi M. Nasolacrimal duct obstruction secondary to dental impaction. Eur J Ophthalmol 2014;24(4):611–3. Crossref | Medline | Google Scholar
-
Tymofieiev OO. Manual of maxillofacial and oral surgery [Russian]. 5th ed. Kyiv: Chervona Ruta-Turs; 2012.
-
Jones AV, Craig GT, Franklin CD. Range and demographics of odontogenic cysts diagnosed in a UK population over a 30-year period. J Oral Pathol Med 2006;35(8):500–7.
-
Paget J. Dentigerous cysts. Lectures on tumours. Vol. 2. London: Wilson and Ogilvy; 1853. Google Scholar
-
Sivolella S, Ricci S, Busca M, Stellini E, Valente M. Maxillary dentigerous cyst and ectopic third molar. Oral Surg 2014;7(S1):728.
-
Sharma S, Chauhan JS. Bilateral ectopic third molars in maxillary sinus associated with dentigerous cyst–a rare case report. Int J Surg Case Rep 2019;61:298–301. Crossref | Medline | Google Scholar
-
Shin DE. Anatomical variations from the point of view of the periodontist. In: Iwanaga J, Tubbs SR, editors. Anatomical variations in clinical dentistry. 1st ed. Cham: Springer International Publishing; 2019. Google Scholar
-
Salman SD. The abnormal ostiomeatal complex and sinusitis. Am J Rhinol 1992;6(1):29–32. Google Scholar
-
Maxymiw WG, Wood RE. Carcinoma arising in adentigerous cyst: a case report and review of the literature. J Oral Maxillofac Surg 1991;49(6):639–43. Crossref | Medline | Google Scholar
-
Groell R, Schaffler GJ, Uggowitzer M, Szolar DH, Muellner K. CT-anatomy of the nasolacrimal sac and duct. Surg Radiol Anat 1997;19:189–91. Medline | Google Scholar
-
Czyz CN, Bacon TS, Stacey AW, Cahill EN, Costin BR, Karanfilov BI, Cahill KV. Nasolacrimal system aeration on computed tomographic imaging: effects of patient positioning and scan orientation. Clin Ophthalmol 2015;9:469–73. Crossref | Medline | Google Scholar
-
Lee H, Ha S, Lee Y, Park M, Baek S. Anatomical and morphometric study of the bony nasolacrimal canal using computed tomography. Ophthalmologica 2012;227(3):1539. Crossref | Medline | Google Scholar
-
Tymofieiev OO, Fesenko II. Anesthesia in oral and maxillofacial surgery. 1st ed. Kyiv: OMF Publishing; 2016.
-
Jude R, Horowitz J, Loree T. Ectopic molars that cause osteomeatal complex obstruction. J Am Dent Assoc 1995;126(12):16557. Crossref | Medline | Google Scholar
-
Emanuelli E, Borsetto D, Brunelloc G, Sivolella S. Endoscopy-assisted removal through combined lower and middle meatotomies of an ectopic upper third molar in the sinus associated with a dentigerous cyst. Oral Maxillofac Surg Cases 2018;4(1):23–31. Google Scholar
-
Mavrodi A, Paraskevas G. Evolution of the paranasal sinuses' anatomy through the ages. Anat Cell Biol 2013;46(4):235–8. Crossref | Medline | Google Scholar
-
Eggesbø HB. Radiological imaging of inflammatory lesions in the nasal cavity and paranasal sinuses. Eur Radiol 2006;16(4):872–88. Medline | Google Scholar
-
Dym RJ, Masri D, Shifteh K. Imaging of the paranasal sinuses. Oral Maxillofac Surg Clin North Am 2012;24(2):175‐89. Crossref | Medline | Google Scholar
-
Barnes L. Surgical pathology of the head and neck. Vol. 1. 2nd ed. New York: CRC Press; 2000.
-
İmamoğlu Ç, Uzel AT, İbrahim İG, Ali İM. Computed tomography findings of a dentigerous cyst associated with an ectopic tooth in the maxillary sinus. Acta Oncologica Turcica 2019;52(3):491–4. Medline | Google Scholar
-
Misch CE. The maxillary sinus lift and sinus graft surgery. In: Misch CE, ed. Implant Dentistry. 2nd ed. St Louis: CV Mosby Co; 1999:469–470.
-
Koenig LJ. Diagnostic imaging: oral and maxillofacial. Vol. 2. 1st ed. Altona: Amirsys; 2011.
-
Zerrin E, Husniye DK, Peruze C. Dentigerous cysts of the jaws: Clinical and radiological findings of 18 cases. J Oral Maxillofac Radiol 2014;2(3):77–81.
-
Hasbini AS, Hadi U, Ghafari J. Endoscopic removal of an ectopic third molar obstructing the osteomeatal complex. Ear Nose Throat J 2001;80(9):667–70.
-
Wardani RS, Lekatompessy M, Senior BA. Modified transnasal endoscopic medial maxillectomy with inferior turbinate flap for dentigerous cyst. Oto Rhino Laryngol Indones 2015;45(2):151e–9e. Google Scholar
-
Bernardi S, Scarsella S, Fabio DD, Oliva A, Girolamo MD, Continenza MA, Cutilli T. Giant follicular cysts extended in pterygo-maxillary fossa, antro-naso-ethmoidal and orbital space associated to exophtalmos and diplopia in young patients. Oral Maxillofacial Surg Cases 2018;4(1):17e–22e. Google Scholar
-
Lee JH, Kim SM, Kim HJ, Jeon KJ, Park KH, Huh JK. Characteristics of bony changes and tooth displacement in the mandibular cystic lesion involving the impacted third molar. J Korean Assoc Oral Maxillofac Surg 2014;40(5):225–32. Crossref | Medline | Google Scholar
-
Nozhenko OA, Zaritska VI, Snisarevskyi PP, Fesenko II. Case report: multilocular type of mandibular simple bone cyst. Part 1: cone beam computed tomography (CBCT) findings, revision of the synonyms and treatment strategies. J Diagn Treat Oral Maxillofac Pathol 2018;2(4):179−85. Crossref | Google Scholar