May 29, 2020
https://doi.org/10.23999/j.dtomp.2020.5.2
J Diagn Treat Oral Maxillofac Pathol 2020;4:95−6.
Under a Creative Commons license
HOW TO CITE THIS ARTICLE
Shamova TO, Pavlenko RA. Post-traumatic facial and intracranial emphysema. J Diagn Treat Oral Maxillofac Pathol 2020;4(5):95–6.
Article
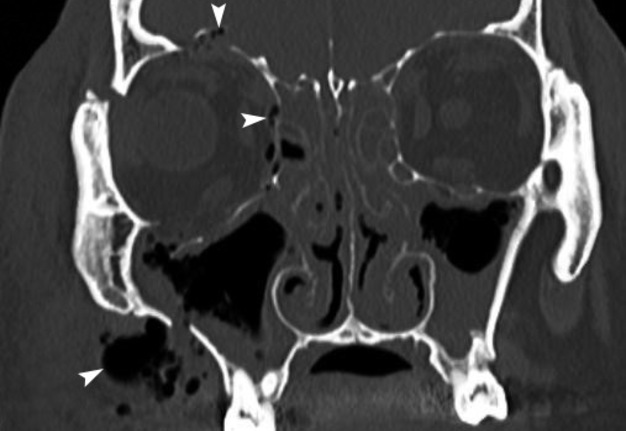
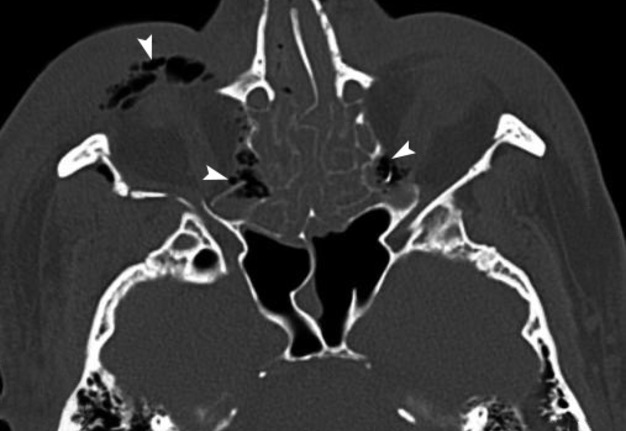
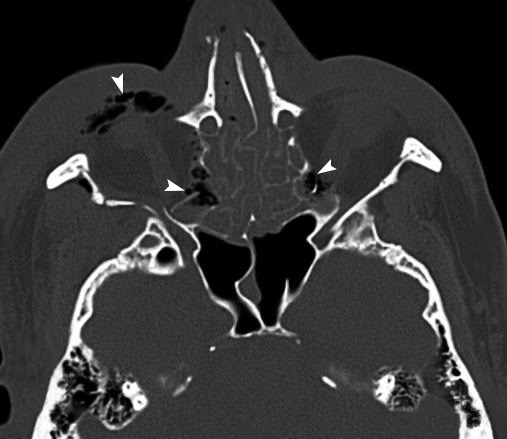
A 48-year-old male was transported to the emergency department after motor vehicle collision. Multi-slice computed tomography (CT) showed multiple facial fractures involving both maxillary sinus walls, walls (lateral, medial, upper and lower) of the right orbit, nasoethmoidal complex, right zygomaticofrontal suture, zygomaticomaxillary buttress, and pterygoid plates of sphenoid bone. Coronal (Panel A) and axial (Panel B) CT scans showed the soft tissues aeration (arrowheads) in the right buccal, periorbital, bilateral orbital regions, and intracranial. CT findings of the intracranially displaced bone fragments help in differential diagnosis between orbital emphysema and pneumocephalus (presence of air in the cranial cavity [in the subdural or intraventricular space]). Attenuation coefficient of the aerated areas varied from –872.1 to –730 Hounsfield units.
Post-traumatic emphysema (synonyms: traumatic emphysema, fracture-induced emphysema) (PTE) can follow the trauma of walls of the maxillary/frontal sinuses, naso-orbital-ethmoidal and zygomatico-maxillary complex. PTE may exacerbate due to sudden rise of pressure after sneezing or blowing the nose. Usually there is no need for some special treatment of the post-traumatic emphysema as it disappears spontaneously during a few days. Nevertheless, the development of acute cellulitis after the PTE appearance can be initiated in case of migration of infected particles from sinuses or traumatic agents (foreign bodies) with a help of air bubbles. The broad-spectrum antibiotic therapy prescribed during the fractures management will help to prevent possible emphysema-induced infection.
This case was managed by neurosurgery, oral-maxillofacial surgery; Opened reduction and internal fixation of facial fractures was done with prophylactic antibiotic coverage. Usually, conservative treatment is enough for intracranial air and its small areas can be observed and allowed to resorb. Unfortunately, he was lost to follow-up in late post-operative period. ■ DTJournal