Understanding the Head and Neck Ultrasound: From Simple to Complicated Cases: Submandibular Abscess
August 30, 2019
https://doi.org/10.23999/j.dtomp.2019.8.3
J Diagn Treat Oral Maxillofac Pathol 2019;4:198–9.
Under a Creative Commons license
HOW TO CITE THIS ARTICLE
Cherniak OS, Nozhenko OA. Understanding the head and neck ultrasound: from simple to complicated cases: submandibular abscess. J Diagn Treat Oral Maxillofac Pathol 2020;4(8):198–9.
Article
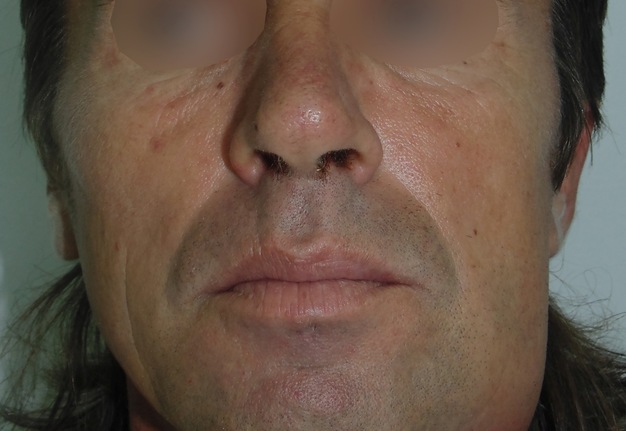
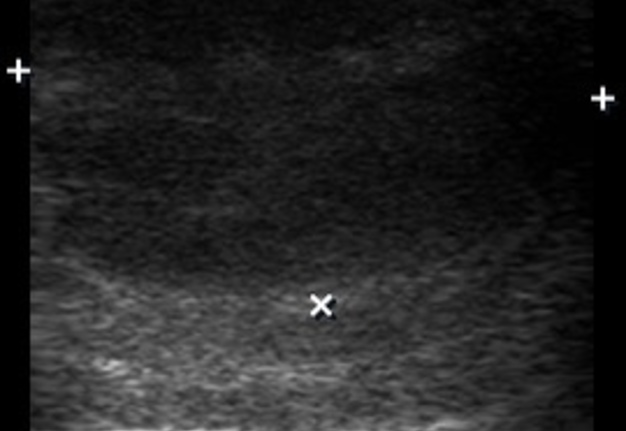
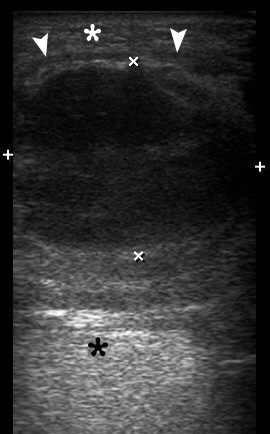
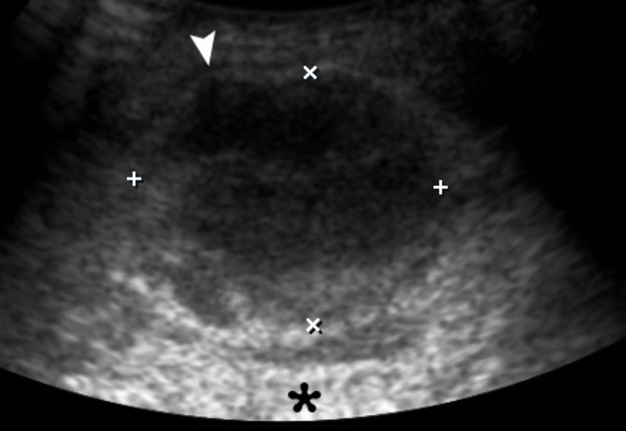
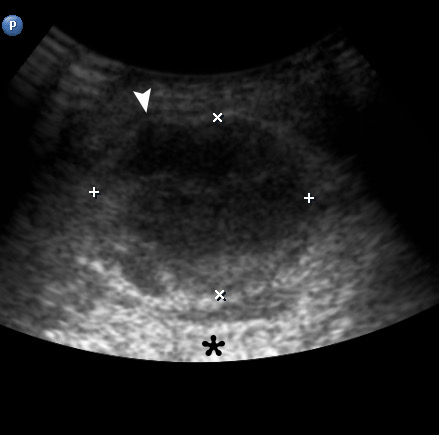
A 43-year-old man was referred to center of maxillofacial surgery and dentistry with a very painful and severe swelling in the left submandibular area, redness of the neck, fever for 1 week, and slight worsening of swallowing. According to history of patient`s complaints, 10 days ago in the area of the present swelling, several movable lesions in the depth of soft tissue were noted. Longitudinal gray scale ultrasound (US) (Panel B, US using linear probe; Panel C, US using convex probe) showed subcutaneous oedema (white asterisk), large collection of well-defiened hypoechoic fluid (indicated by ‘+’ and ‘×’ calipers) under the platysma muscle (arrowheads). Movement of the fluid during dynamic compression was noted. The usual artifact for fluid-contained objects, posterior acoustic enhancement, is indicated by black asterisks. No ultrasound signs of gas loculations in the soft tissue and fluid were found. This allows assuming the absence of gas-forming organisms. Also, the enlarged lymph nodes were noted at the left neck. The diagnosis of submandibular abscess due to non-odontogenic inflammation and suppurate fusion of the lymph nodes was established. The abscess was lanced, and drained using submandibular approach. 18 ml of purulent material was obtained. At the next morning after surgery, the patient felt significant improvement; 1 week follow-up the patient was clinically well. ■ DTJournal