Anterior Maxillary Distraction − a Boon to Treat Cleft Maxillary Hypoplasia
June 30, 2017
https://doi.org/10.23999/j.dtomp.2017.2.3
J Diagn Treat Oral Maxillofac Pathol 2017;1:65–8.
Under a Creative Commons license
HOW TO CITE THIS ARTICLE
Richardson S, Selvaraj D, Krishna S. Anterior maxillary distraction − a boon to treat cleft maxillary hypoplasia. J Diagn Treat Oral Maxillofac Pathol 2017;1(2):65−8.
ABSTRACT
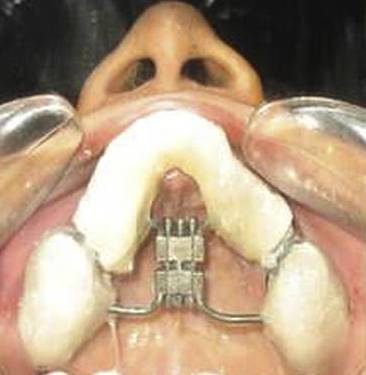
We describe our experience of using anterior maxillary distraction for the correction of cleft related maxillary hypoplasia. Clear historical overview and meticulous description of the surgical technique are given. The technique is described step-by-step from the type of incision to the prosthetic rehabilitation. An advantage of anterior maxillary distraction over the other conventional techniques is reasoned. The paper is illustrated both the view of intra-oral tooth-borne screw appliance and four representative cases. This technique provides excellent well-predicted result and can be widely recommended in anterior maxillary distraction.
Introduction
Age-old techniques like Le Fort I osteotomy and Le Fort I distraction have been used for correction of cleft related maxillary hypoplasia [1]. In 2003, Dolanmaz first used the anterior segmental maxillary distraction technique [2]. Since then it has become a very useful technique for correction of cleft related maxillary hypoplasia. The greatest advantage of anterior maxillary distraction over the other aforementioned conventional techniques is that since only the anterior portion of the maxilla is being moved forward, there is no worsening effect on velopharyngeal closure [3, 4].
Surgical and Prosthetic Techniques
The appliance (Fig 1) can be placed intra-operatively as advocated by Gunaseelan or it can be placed prior to operation as practiced by the author. This prevents cement failure. The procedure takes place under general anesthesia with oral endotracheal intubation. A maxillary vestibular incision is made from first molar to another molar. The mucoperiosteum is reflected to expose the maxillary bone up to the infraorbital foramen. A buccal linear osteotomy cut is made on both sides at a similar level with a 701 bur under copious irrigation above the level of the root apices from the pyriform rim to the predetermined distraction site between the premolars and molars parallel to the occlusal plane. Lateral nasal osteotomes are used to cut the lateral nasal wall from the pyriform rim at the same level of the buccal cut on both sides. Care is taken to protect the nasal mucosa. The nasal septum is then transected at its base just beyond the distraction site using a guarded septal osteotome. Vertical interdental cuts are made between the second premolar and first molar through the buccal cortex using a bur. These are then deepened using spatula osteotomes. This is followed by palatal osteotomy using a curved osteotome with very gentle force because using tactile sensation for guidance. The palatal bone is not cut completely to avoid damage to the periosteum. Luxation on both sides is performed using gentle force to fracture the anterior maxilla. The completion of the osteotomy cut is confirmed by activation of the distractor screw intraoperatively and symmetrical movement on both sides was confirmed. Closure of the vestibular incision was then performed using a 3-0 Vicryl suture. Activation of the screw starts typically on the fifth postoperative day and at the rate of four turns twice a day. This advances the maxilla by 0.72 cm per day.
After completion of distraction, the maxilla is left for consolidation for 12-14 weeks. Thereafter the appliance is removed and prosthetic rehabilitation for the gap created is done by fixed partial denture (FPD)/dental implants.
Conclusions
This technique improves dental arch crowding, advances the maxilla and improves the profile of the patient and is also better for the speech of the patient [5].
Funding
None.
Conflict of Interests
The authors declare no conflict of interest.
Role of Author and Co-authors
Sunil Richardson (concept of the paper and writing).
Dhivakar Selvaraj (material collection and writing).
Shreya Krishna (editing).
Ethical Approval
Approval was obtained from the Medical Ethics Committee of the Rajas Dental College and Hospital.
Patient Consent
Written patient consent was obtained to publish the clinical photographs.
References (5)
- Wang XX, Wang X, Li ZL, Yi B, Liang C, Jia YL, Zou BS. Anterior maxillary segmental distraction for correction of maxillary hypoplasia and dental crowding in cleft palate patients: a preliminary report. Int J Oral Maxillofac Surg 2009;38:1237. Crossref | Medline | Google Scholar
- Dolanmaz D, Karaman AI, Ozyesil AG. Maxillary anterior segmental advancement by using distraction osteogenesis: a case report. Angle Orthodon 2003;73:201−5. Crossref | Medline | Google Scholar.
- Richardson S, Agni NA, Selvaraj D. Anterior maxillary distraction using a tooth-borne device for hypoplastic cleft maxillas − a pilot study. J Oral Maxillofac Surg 2011;69:e542−e548. Crossref | Medline | Google Scholar
- Richardson S, Seelan NS, Selvaraj D, Khandeparker RV, Gnanamony S. Perceptual speech assessment after anterior maxillary distraction in patients with cleft maxillary hypoplasia. J Oral Maxillofac Surg 2016;74:1239.e1−1239.e9. Crossref | Medline | Google Scholar .
- Richardson S, Selvaraj D, Khandeparker R, Seelan NS, Richardson S. Tooth-borne anterior maxillary distraction for cleft maxillary hypoplasia: our experience with 147 patients. J Oral Maxillofac Surg 2016;74:2504.e1−2504.e14. Crossref | Medline | Google Scholar .