Management of the Bone Deformity Caused by Congenital Cyst of the Periorbital Area: Analysis of the Surgical Technique and a Short-term Outcome
March 31, 2023
J Diagn Treat Oral Maxillofac Pathol 2023;7: 21–32.
DOI: 10.23999/j.dtomp.2023.3.1
Under a Creative Commons license
HOW TO CITE THIS ARTICLE
Tymofieiev OO, Fesenko II, Cherniak OS, Zaritska VI, Snisarevskyi PP, Shelest OB. Management of the bone deformity caused by congenital cyst of the periorbital area: analysis of the surgical technique and a short-term outcome. J Diagn Treat Oral Maxillofac Pathol 2023;7(3):21–32. https://doi.org/10.23999/j.dtomp.2023.3.1
NATIONAL REPOSITORY OF ACADEMIC TEXTS
https://nrat.ukrintei.ua/en/searchdoc/2023U000207/
SUMMARY
The congenital periorbital cysts like dermoids/epidermoids, in rare cases, can require not only its’ excision but also correction/camouflage of the caused bone deformity. This management can require virtual surgical planning, osteotomy, and placement of the custom-made patient implant. In this report, the ultrasonography (USG) was proved as a highly effective imaging for the presurgical verification of the mass’s structure and establishment of the clinical diagnosis. The multi-slice computed tomography (MSCT), even on a two-slice MSCT machine, provided high-quality three-dimensional reconstruction of the area of bone deformation caused by the cyst and allowed for accurate surgical planning. A 20-year-old male patient with a congenital periorbital epidermoid cyst that led to the deformation of the lateral orbital rim was treated using the soft tissue volume-increasing technique for the correction of bone deformation following cyst removal. Analysis of the terminological diversity related with dermoid/epidermoid cysts is presented. Early diagnostics and management of congenital periorbital cysts can decrease the visual, orbital, and esthetic complications, as well as the need to perform bone reconstructive surgeries or other corrective surgical procedures.
INTRODUCTION
Epidermoid and dermoid cysts are relatively rare congenital cysts that develop because of a malformation of the ectoderm.1,2 A recent study (2019) proves that the transformation of a radiological epidermoid cyst into a pathological dermoid cyst is possible.3 But not vice versa.3
Pushker and colleagues (2020) emphasize that most of the periorbital cysts were found in relation to fronto-zygomatic suture.4 Their retrospective observational study of 280 cases of epidermoid/dermoid cysts summarized that in 75.35 percent of patients (i.e., majority of cases) with periorbital and orbital cyst the adjacent bony changes were noted.4 Thus, the management in such cases can require not only excision of the cyst, but also correction of the bone defect or deformity5,6.
We found no data in the English-language literature that describe the management of the lateral orbital rim deformity, caused by a congenital epidermoid cyst, as we report in our case. A 20-year-old male patient with a congenital periorbital cyst that led to the bone deformation was treated using the soft tissue volume-increasing technique for the correction of bone deformation noted after cyst removal. Analysis of the technique and short-term outcome is presented.
CASE AND SURGICAL TECHNIQUE
A 20-year-old Caucasian man was referred to the Center of Maxillofacial Surgery and Dentistry in May 2015 with a mass in the left periorbital area (Fig 1). According to the patient’s father, the presence of a subcutaneous neoplasm was noted immediately at birth. After that, painless slow growth was gradually noted. The mass was painless and “dough like” on palpation7,8. No punctum common for the punctum-associated cyst9 was visualized.
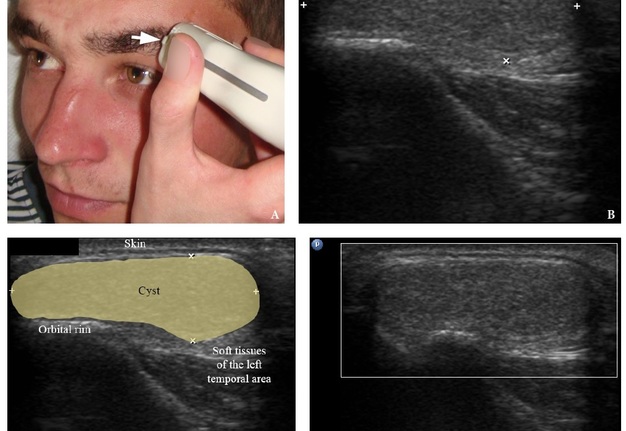
USG was performed (model HD11 XE, Koninklijke Philips N.V., Eindhoven, The Netherlands) by two doctors of ultrasound diagnostics (O.S.C., her experience in head and neck USG is 16 years; I.I.F., his experience in USG is 9 years) using a 12-3 MHz linear transducer (probe). The gray scale USG in a longitudinal direction of the mass (Fig 2) showed a well-demarcated lesion measured 2.95 ×1.02 cm and located above the bony surface of the left orbital rim. Content was heterogeneous and no signs of posterior acoustic enhancement was noted. The color Doppler USG showed no vascularity within or in the walls of this cystic lesion.
FIGURE 2. Position of the linear probe (A). Arrow labels the probe’s bump (i.e., its side and side of the ultrasound image at the screen). The longitudinal gray scale USG of the congenital epidermoid cyst in the left periorbital region (B, С). USG shows a well-demarcated lesion located above the bony surface of the left lateral orbital rim and measured 2.95 ×1.02 cm (indicated by ‘+’ and ‘×’ calipers). The heterogeneous content is separated from the surrounding tissues by a thin cystic membrane. No signs of posterior acoustic enhancement are noting. The color Doppler USG (D) shows no vascularity within or in the walls of the cyst. The “P” letter at the upper left corner of the sonogram indicates on the probes’ sides (corresponds to the probe bump). The “depth” of the cropped sonograms is 3.0 cm. Printed with permission and copyrights retained by I.I.F. and O.S.C.
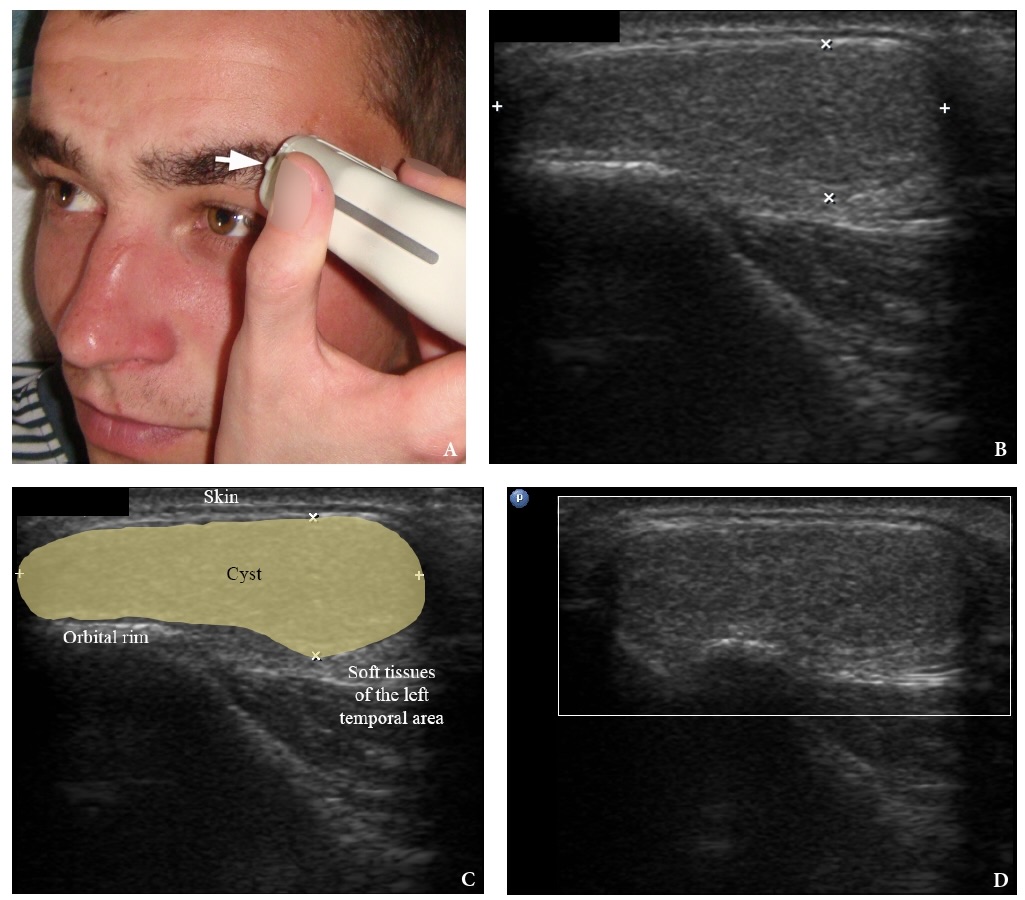
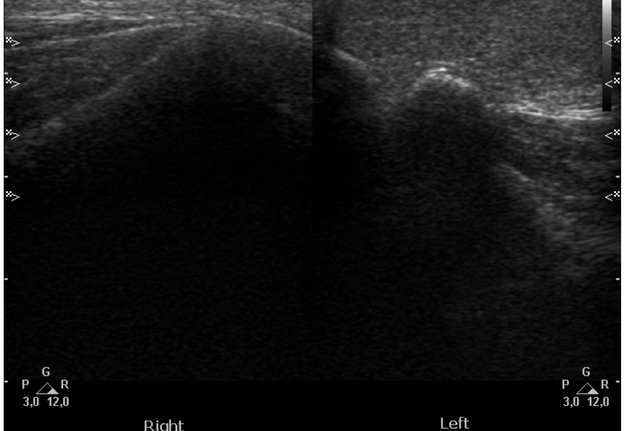
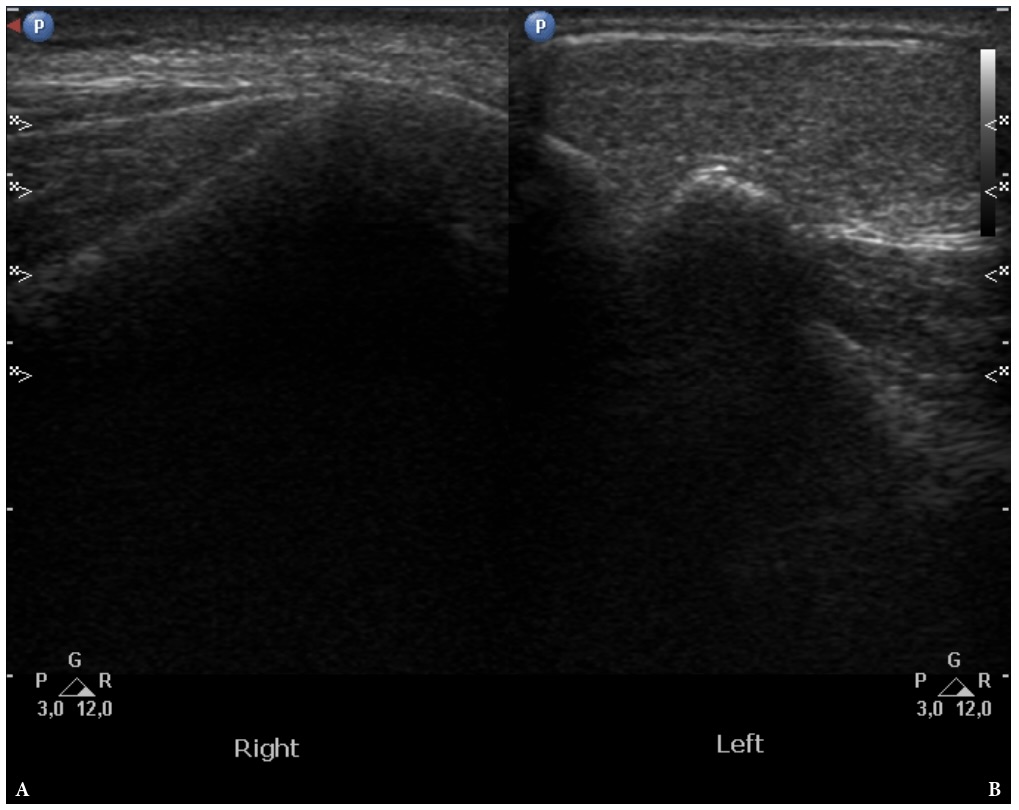
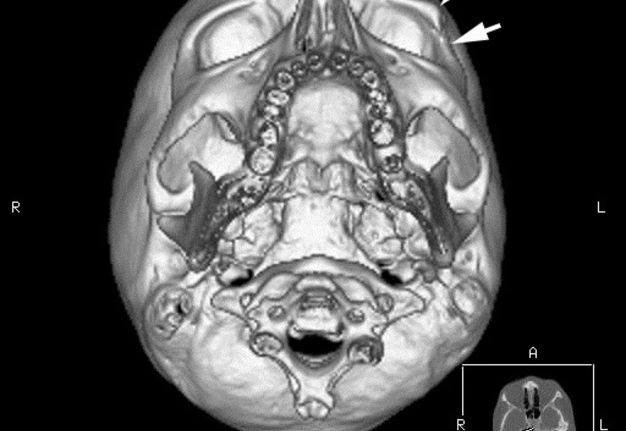
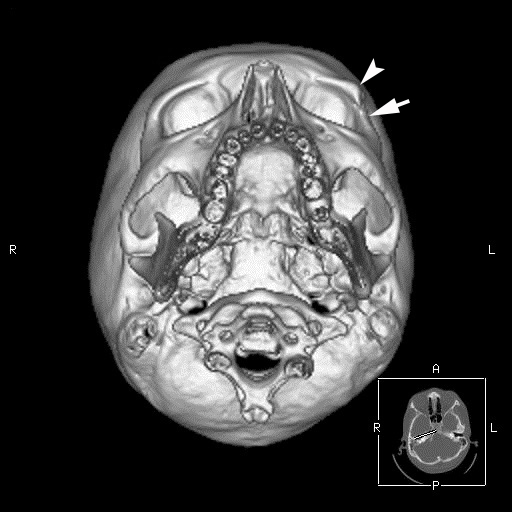
Comparison of the grayscale sonograms obtained from the right (healthy) and left (affected) periorbital sides is presented in Figure 3. A non-contrast multi-slice computed tomography (MSCT) performed on General Electric CT machine (HiSpeed Dual, Boston, Massachusetts, United States) revealed bone deformity of the left lateral orbital rim in area of zygomaticofrontal suture, under the congenital cyst (Fig 4). The MSCT showed bone depression in area of cyst’s “bed” and a bony rise in the superior part of the bone adjacent to the “bed.”
FIGURE 3. The gray scale sonograms compare right (A) and left (B) periorbital sides. Image B shows the cystic lesion covering the left lateral orbital rim from the external surface. The “depth” of sonograms is 5.0 cm. The “P” letters at the upper left corners of the sonograms indicate on the probe sides (corresponds to the probe bump). Three capital letters (P, G, and R) in the lower left corner of the sonograms mean penetration, gain, and resolution. Two numbers (3,0 and 12,0) mean: 3,0 MHz (i.e., 3.0 MHz), minimum frequency of linear probe; 12,0 MHz (i.e., 12.0 MHz), maximum frequency of linear probe. Printed with permission and copyrights retained by O.S.C. and I.I.F.
FIGURE 4. Three-dimensional MSCT scan shows deformity of the left lateral orbital rim in area of zygomaticofrontalsuture. Arrow labels a bone depression in area of cyst’s “bed” and arrowhead indicates on a bony rise in the superior part of the bone adjacent to the “bed.” R, right side; L, left side; A, anterior side; P, posterior side. Printed with permission and copyrights retained by I.I.F.
The problem with this deformity was that the cyst simultaneously led to bone depression in a lower part of the rim and a bone rise in its upper part. According to the classification of bone defects caused by congenital cysts, presented by Sathananthan and colleagues (1993), such bone deformation can be classified as abnormal shape.5
It was decided to apply the method of increasing the volume of soft tissues due to stimulation of granulation tissue growing in the wound. The surgery was performed under the local potentiated anesthesia (2.0 mL of Dexalgin® inject [Laboratorios Menarini S.A., Barcelona, Spain] intramuscularly 40 minutes before surgery and 2.2 mL of 4% Ultracaine® D-S forte [Aventis Pharma Deutschland GmbH, Frankfurt, Germany], using an anesthetic solution in cartridges [1.7 mL per cartridge] infiltrated locally). Excision of cystic lesion was performed through 3.0-cm skin incisiondone along the tail of the left eyebrow. The cyst was removed without breaking the integrity of its wall, thus avoiding its contents entering the wound.
A double perforated tubular drainage (in which two tubes were sewn together), self-made from a dropper system, was inserted between the sutures. This step was done for preventing the deep and superficial layers of the wound from sticking together. This step allowed to create the space for granulation tissue and stimulate its growth. The double tubular drainage was gradually pulled up from the wound and trimmed to better hold it in the wound with sterile gauze on the patch. The drain was removed on the third day after the operation due to its gradual displacement by soft tissues from the wound.
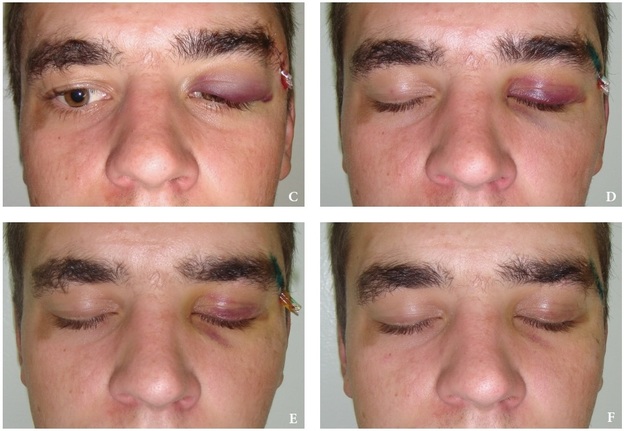
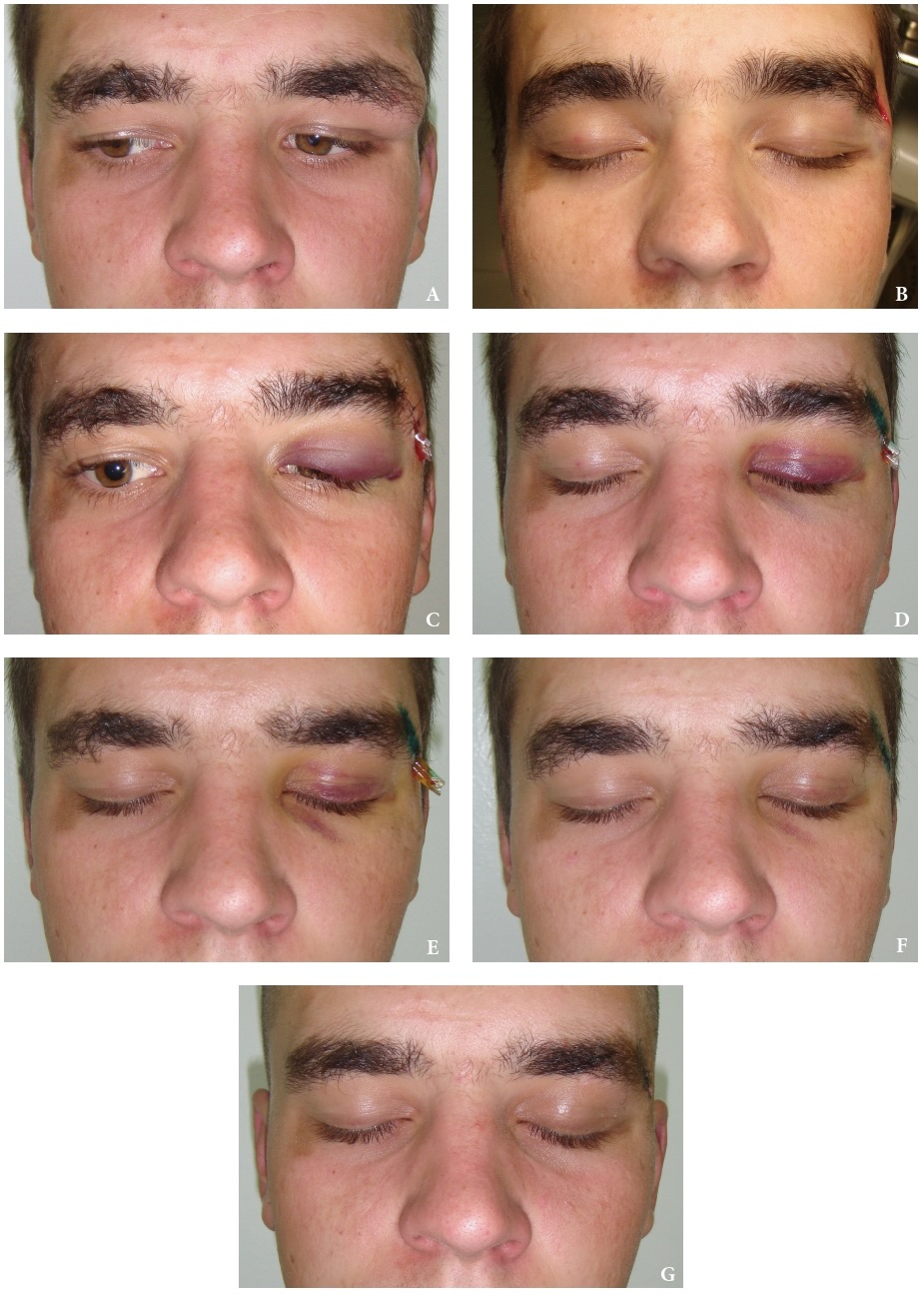
Comparison of the state of soft tissues in the preoperative period, intraoperatively, and during the next ten days is presented in Figure 5. The postoperative period was marked occasionally by the presence of a slight hemorrhage in the upper eyelid but generally passed without significant complications. At the time of our last examination of the patient on the 10th day, the patient was extremely satisfied with the aesthetic outcome. Due to the subsequent military service of the patient, we were not able to evaluate the long-term outcome of this surgical technique.
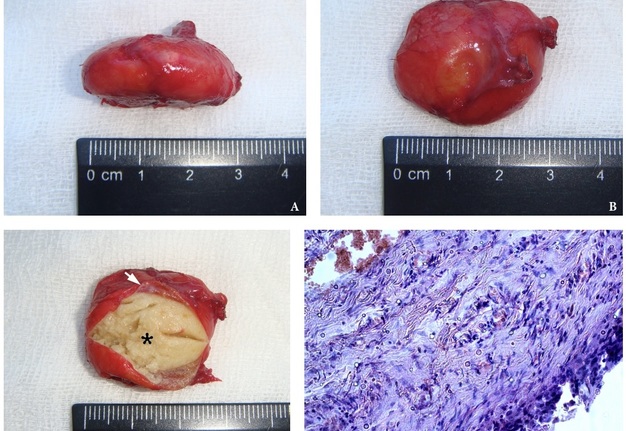
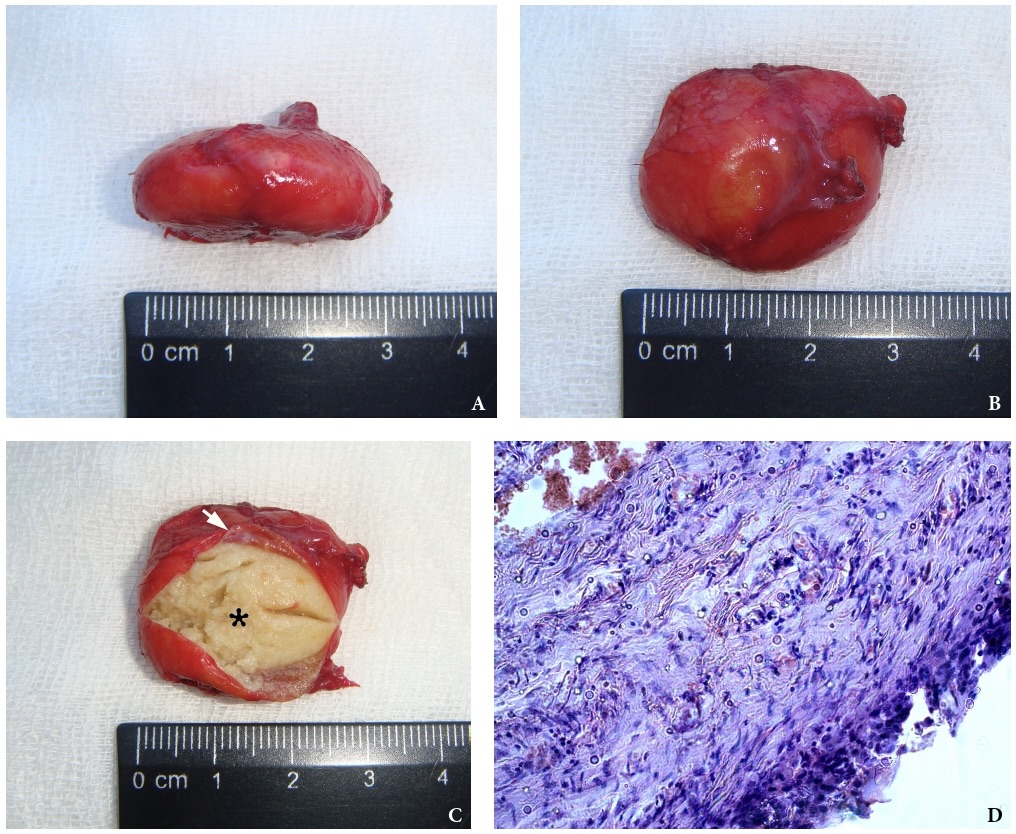
Figure 6 demonstrate the specimen (3.0 × 1.3 cm) and histopathological photograph. The presence of a thin red cystic wall and fine-grained yellowish content was noted upon the macroscopic examination of the specimen. Histopathological examination by three pathologists revealed the cyst wall lined with stratified squamous epithelium with plethoric vessels and histiocytic infiltration (i.e., inflammation). In the lumen of the cyst, the presence of desquamated dystrophic epithelium was noted. Epidermoid cyst with inflammation was established as a histopathological diagnosis by three experienced doctor-pathologists (V.I.Z., P.P.S., and O.B.S.).
FIGURE 6. Specimen of the cyst (3.0 × 1.3 cm) after its removal (A–C). Noted a thin red cystic wall (arrow) and fine-grained yellowish content (asterisk). Microphotograph (D) shows the cyst wall lined with stratified squamous epithelium with plethoric vessels and histiocytic infiltration (i.e., inflammation) (hematoxylin-eosin, original magnification ×200).Images A–C printed with permission and copyrights retained by I.I.F. Image D printed with permission and copyrights retained by V.I.Z.
DISCUSSION
Terms such as dermoid and epidermoid cysts have a lot of terminological confusion. This confusion on the one hand is associated with the localization of these neoplasms, and on the other with the reasons for their appearance. Considering such definitions as heterotopia, teratoma, and choristoma described by Lee and Roland (2013)9 it’s worthy to mention that both congenital cysts, dermoid and epidermoid, belong to choristomas (Heo and colleagues, 2012)10. Smirniotopoulos and Chiechi (1995) presented important analysis of some theories about the origins of dermoids and epidermoids and their embryologic development.1
In the radiological, surgical, and histopathological literature, there is terminological diversity and slight confusion in attempting to describe epidermoid cysts (as congenital lesions). In some literature sources, epidermoids are termed as epidermal cysts.10
Shear and Speight (2007) termed dermoid and epidermoid cyst as developmental cysts which are distinct cystic entities from two types of keratinous cysts of the skin— epidermal traumatic type and trichilemmal (pilar) type.7
Some authors in the East European states term dermoid and epidermoid cysts as dermoid(epidermoid) cysts (i.e., using parentheses and thus emphasizing the similarity of these cysts).2
Balasundaram and colleagues (2019) stated, as both epidermoid and dermoid cysts have the same pathogenesis, that these cysts should be better named in the pathological literature as epidermoid/dermoid (i.e., using forward slash), and not as separate entities.3
Ximena Wortsman (2018) describe epidermal cyst as dermal and/or hypodermal cysts composed of epidermal elements that include a granular layer and keratinous material.12 The author describes the next synonyms for the epidermal cyst—epidermoid cyst, keratinous cyst, inclusion cyst, and infundibular cyst.12 Moreover, the author reported that sebaceous cyst is a misnomer because it does not have a sebaceous origin.12
Dermoids are lined by epithelium and differ from epidermoids in that they contain some evidence of epithelial appendages.13,14 Ibrahim and colleagues (2011) divided dermoid cysts into complex and simple dermoid.13,14 Scientists emphasize that simple dermoids contains only skin components, and complex dermoids contain mesodermal elements.13,14
Huang and colleagues (2011) use only the term epidermal cysts (but divided into congenital and acquired) to describe both congenital (i.e., congenital epidermoid cysts) and acquired cysts (i.e., which resulted from occlusion of the pilosebaceous unit or implantation of viable epidermal cells in the dermis or subcutis).15
In the recent studies we propose to apply the term punctum-associated cyst11,16 for the description of the acquired epidermal cyst which is also termed as atheroma (Peter Jecker, 2019)17 and sebaceous gland cyst (what is misnomer).
From a surgical point of view, no matter what terms such congenital cysts as epidermoid/dermoid cysts are called, their treatment is the same surgical excision. But, in case of punctum-associated cyst11,16 (atheroma)2, the partial excision of the overlying skin is recommended.
Studies reported that the most common locations of the dermoid cysts, as remnant cysts, are the tail of the eyebrow or upper eyelid.12 The same was with the case in this report of congenital epidermoid cyst. Our opinion is that when interviewing the patient or relatives, it is important to immediately determine whether it is a congenital or acquired cyst. The detailed scheme presented in the work of the Erich and Johnsen (1953) of possible head and neck locations of dermoids/epidermoids may be useful for practicing specialists in making a preliminary diagnosis.14 Their data evidenced that orbital/periorbital dermoids/epidermoids18,19 note in 49.5 percent of head and neck cases.14
Such two methods of diagnosis as USG and MSCT made it possible to accurately verify epidermoid in the presented case and establish the volume of bone deformation. USG proved its usefulness not only in cases of large20–22 but also in the case of a very small superficial congenital developmental anomaly of the head and neck region23. Rappaport and colleagues (2023) emphasized that in the case of superficial epidermoid localization the ultrasound technique can confirm the diagnosis.24
Many authors tried to summarize the typical ultrasound pictures characteristic of both congenital epidermoids/dermoids and acquired epidermal cysts.25–33 And the presented ultrasound pictures of cysts differ significantly in different literature sources. Considering the case of a congenital epidermoid presented by us, we consider it expedient to conduct a comparative study of sonograms of a much larger group of patients with a similar pathology. Also, we consider it expedient to photograph the contents of the cyst after its removal and incision of the specimen. Because macroscopically, the congenital epidermoid cysts and acquired epidermal cysts (i.e., punctum-associated cysts) have a distinctly different color of the cystic content. Just as the color of their wall is different.
The surgical technique that was presented in this case can be used only as a first stage or in cases where the patient does not have health insurance that would cover the manufacture of custom implant since this technique only slightly camouflages the area of deformation. In any case, it is more appropriate to use virtual surgical planning (Franz and colleagues, 2019) and the patient specific implant (Aldana and colleagues, 2020; Arango and colleagues, 2021; Habib and Yoon, 2021)34–37.
Analyzing the reconstructive options for the superior-lateral orbital limb area, it is worth to understand the bone cement and Leibinger plate way of reconstruction (Heo and colleagues, 2012).10 The authors applied this management strategy for the gigantic epidermoid cyst (9.8 × 5.2 × 4.0 cm) of the periorbital/orbital region in a 62-year-old female.10
Analyzing the short-term outcome in the presented periorbital case, it is worth noting that from the front view the aesthetic outcome is much more acceptable compared to the inferior view (Fig 7).
We completely agree with Dave and colleagues (2021) who emphasize that long-term existence of dermoid/epidermoids can lead to secondary visual, orbital, and radiological effects.38 It should be supplemented that early diagnostics and management can also decrease the need to perform bone reconstructive surgeries or other corrective surgical procedures.
CONCLUSION
The surgical technique presented in this article makes it possible to camouflage small bone defects in aesthetically significant areas of the face. Ultrasonography in combination with computed tomography, which proves its effectiveness both for establishing a preoperative diagnosis and for planning the stages of an excisional biopsy with the subsequent application of a soft tissues volume-increasing technique. However, obtaining long-term results in a larger group of patients is recommended.
TERM OF CONSENT
Writing patient’s consent was obtained for publication the photos.
AUTHOR CONTRIBUTIONS
Conceptualization: Fesenko II, Cherniak OS. Sonographic data acquisition: Cherniak OS, Fesenko II. Surgical advice: Tymofieiev OO. Surgical images acquisition: Fesenko II. Histological data acquisition: Zaritska VI, Snisarevskyi PP, Shelest OB. Data analysis or interpretation: Cherniak OS, Zaritska VI. Drafting of the manuscript: Fesenko II. Critical revision of the manuscript and approval its final version: all authors.
CONFLICT OF INTERESTS
The authors declare no conflict of interest.
FUNDINGS
No funding was received for this study.
REFERENCES (38)
-
Smirniotopoulos JG, Chiechi MV. Teratomas, dermoids, and epidermoids of the head and neck. Radiographics1995;15(6):1437–55. https://doi.org/10.1148/radiographics.15.6.8577967
-
Tymofieiev OO. Manual of maxillofacial and dental surgery [Russian]. 5th ed. Kyiv: Chervona Ruta-Turs; 2012. p. 728–55.
-
Balasundaram P, Garg A, Prabhakar A, et al. Evolution of epidermoid cyst into dermoid cyst: embryological explanation and radiological-pathological correlation. Neuroradiol J 2019;32(2):92–7. https://doi.org/10.1177/1971400918821086
-
Pushker N, Meel R, Kumar A, et al. Orbital and periorbital dermoid/epidermoid cyst: a series of 280 cases and a brief review. Can J Ophthalmol 2020;55(2):167–71. https://doi.org/10.1016/j.jcjo.2019.08.005
-
Sathananthan N, Moseley IF, Rose GE, Wright JE. The frequency and clinical significance of bone involvement in outer canthus dermoid cysts. Br J Ophthalmol 1993;77(12):789–94. https://doi.org/10.1136/bjo.77.12.789
-
Cavazza S, Laffi GL, Lodi L, et al. Orbital dermoid cyst of childhood: clinical pathologic findings, classification and management. Int Ophthalmol 2011;31(2):93–7. https://doi.org/10.1007/s10792-011-9419-y
-
Shear M, Speight P. Developmental cysts of the head and neck. In: Shear M, Speight P. Cysts of the oral and maxillofacial regions. 4th ed. Johannesberg: Blackwell; 2007. p. 181–91.
-
Ashok S, Sahni P, Nayak MT. Periorbital epidermoid cyst in an elderly male. Med J D Y Patil Univ 2014;7:388–91. https://doi.org/10.4103/0975-2870.129006
-
Lee KH, Roland PS. Heterotopias, teratoma, and choristoma. In: Kountakis SE, editor. Encyclopedia of otolaryngology, head and neck surgery. Berlin, Heidelberg: Springer; 2013. p. 1057–1218. https://doi.org/10.1007/978-3-642-23499-6_642
-
Heo MS, An JH, Yang JW. Giant epidermal cyst of the periorbital area. J Craniofac Surg 2012;23(1):e10–e12.https://doi.org/10.1097/scs.0b013e3182420766
-
Fesenko II, Snisarevskyi PP, Zaritska VI. Infected punctum–associated cyst mimicking erysipelas. J Diagn Treat Oral Maxillofac Pathol 2021;5(2):15–9. https://doi.org/10.23999/j.dtomp.2021.2.1
-
Wortsman X. Ultrasound of common non-vascular benign cutaneous lesions. In: Wortsman X, editor. Atlas of dermatologic ultrasound. Cham: Springer International Publishing AG; 2018. p. 35–84. https://doi.org/10.1007/978-3-319-89614-4
-
Ibrahim M, Hammoud K, Maheshwari M, Pandya A. Congenital cystic lesions of the head and neck. Neuroimaging Clin N Am 2011;21(3):621–39. https://doi.org/10.1016/j.nic.2011.05.006
-
Erich JB, Johnsen DS. Congenital dermoid cyst. Am J Surg 1953;85(1):104–7. https://doi.org/10.1016/0002-9610(53)90598-4
-
Huang CC, Ko SF, Huang HY, et al. Epidermal cysts in the superficial soft tissue: sonographic features with an emphasis on the pseudotestis pattern. J Ultrasound Med 2011;30(1):11–7.https://doi.org/10.7863/jum.2011.30.1.11
-
Tymofieiev OO, Ushko NO, Fesenko II, Cherniak OS. Maxillofacial surgery specialization in Ukraine: a new order and step in the growth of the specialty: analysis of qualification categories. J Diagn Treat Oral Maxillofac Pathol 2021;5(4):43–51. https://doi.org/10.23999/j.dtomp.2021.4.3
-
Jecker P. Sonography of other neck masses. In: Welkoborsky HJ, Jecker P, editors. Ultrasonography of the head and neck. Cham: Springer Nature Switzerland AG; 2019. p. 95–138. https://doi.org/10.1007/978-3-030-12641-4_6
-
Veselinović D, Krasić D, Stefanović I, et al. Orbital dermoid and epidermoid cysts: case study. Srp Arh Celok Lek2010;138(11–12):755–9. https://doi.org/10.2298/sarh1012755v
-
Eshraghi B, Shahsanaei A, Abounoori M, Pourazizi M. Atypical intraorbital dermoid and epidermoid cyst: asingle institution cross-sectional retrospective study. Ann Med Surg (Lond) 2022;79:103997. https://doi.org/10.1016/j.amsu.2022.103997
-
Tymofieiev OO, Fesenko II, Cherniak OS, Zaritska VI. Features of diagnostics, clinical course and treatment of the branchial cleft cysts. J Diagn Treat Oral Maxillofac Pathol 2017;1(1):15–31. https://doi.org/10.23999/j.dtomp.2017.1.3
-
Demidov VH, Cherniak OS. Hemolymphangioma of the neck. J Diagn Treat Oral Maxillofac Pathol2022;6(8):114–6. https://doi.org/10.23999/j.dtomp.2022.8.2
-
Wong SSM, Dai EYL, Tang EWK, Ahuja AT. Head and neck. In: Ahuja AT, Antonio GE, Nung RCH, et al.Essential radiology for medical students, interns and residents. Kyiv: OMF Publishing; 2017. p. 1–50.
-
Walsh R, North J, Cordoro KM, et al. Midline anterior neck inclusion cyst: a novel superficial congenital developmental anomaly of the neck. Pediatr Dermatol 2018;35(1):55–8. https://doi.org/10.1111/pde.13371
-
Rappaport A, Grouwels P, Strybol D. A rare case of a preperitoneal epidermoid cyst. Radiol Case Rep2022;18(3):745–9. https://doi.org/10.1016/j.radcr.2022.11.032
-
Yuen HY, Ahuja AT. Benign clinical conditions in the adjacent neck. In: Sofferman RA, Ahuja AT, editors.Ultrasound of the thyroid and parathyroid glands. Berlin: Springer Science+Business Media, LLC: 2012. p. 229–59. https://doi.org/10.1007/978-1-4614-0974-8_11
-
Neudorfer M, Leibovitch I, Stolovitch C, et al. Intraorbital and periorbital tumors in children--value of ultrasound and color Doppler imaging in the differential diagnosis. Am J Ophthalmol 2004;137(6):1065–1072. https://doi.org/10.1016/j.ajo.2004.01.050
-
Ahuja AT. Lumps and bumps in the head and neck. In: Practical head and neck ultrasound. Ahuja AT, Evans R, editors. 1st ed. London: Greenwich Medical Media Limited; 2000. p. 87–106.
-
Choi HI, Choi YH, Cheon JE, et al. Ultrasonographic features differentiating thyroglossal duct cysts from dermoid cysts. Ultrasonography 2018;37(1):71–7. https://doi.org/10.14366/usg.17027
-
Wong KT, Lee YY, King AD, Ahuja AT. Imaging of cystic or cyst-like neck masses. Clin Radiol 2008;63(6):613–22. https://doi.org/10.1016/j.crad.2007.12.007
-
Kim CS, Na YC, Yun CS, et al. Epidermoid cyst: a single-center review of 432 cases. Arch Craniofac Surg2020;21(3):171–5. https://doi.org/10.7181/acfs.2020.00248
-
Hoang VT, Trinh CT, Nguyen CH, et al. Overview of epidermoid cyst. Eur J Radiol Open 2019;6:291–301. https://doi.org/10.1016/j.ejro.2019.08.003
-
Bruneton JN, Tranquart F, Brunner P, Mourou MY. Miscellaneous. In: Bruneton JN, editor. Applications of sonography in head and neck pathology. Berlin Heidelberg: Springer-Verlag; 2002. p. 253–86. https://doi.org/10.1007/978-3-642-56213-6_8
-
Delantoni A. Sonographic anatomy and pathology floor of the mouth. In: Orhan K, editor. Ultrasonography in dentomaxillofacial diagnostics. Cham: Springer Nature Switzerland AG; 2021. p. 99–108. https://doi.org/10.1007/978-3-030-62179-7_8
-
Franz L, Isola M, Bagatto D, et al. A novel approach to skull-base and orbital osteotomies through virtual planning and navigation. Laryngoscope 2019;129(4):823–31. https://doi.org/10.1002/lary.27479
-
Aldana H, Orozco M, Ordoñez L, et al. Trabecular juvenile ossifying fibroma management by virtual surgical planning, piezoelectric surgery, and simultaneous patient specific implant (PSI) reconstruction. J Diagn Treat Oral Maxillofac Pathol 2020;4(2):39–48. https://doi.org/10.23999/j.dtomp.2020.2.6
-
Arango H, Vidal J, Moncada JA, López JP. Alternative management of severe maxillary asymmetry with multi-vector osteogenic distraction and customized polyetheretherketone (PEEK) prosthesis. J Diagn Treat Oral Maxillofac Pathol 2021;5(6):69–76. https://doi.org/10.23999/j.dtomp.2021.6.2
-
Habib LA, Yoon MK. Patient specific implants in orbital reconstruction: a pilot study. Am J Ophthalmol Case Rep2021;24:101222. https://doi.org/10.1016/j.ajoc.2021.101222
-
Dave TV, Gupta Rathi S, Kaliki S, Mishra D. Orbital and periorbital dermoid cysts: comparison of clinical features and management outcomes in children and adults. Eur J Ophthalmol 2021;31(5):2631–8. https://doi.org/10.1177/1120672120964686