Ultrasonographic Assessment of Masseter Muscle Region and Minimally Invasive Treatment of Post-Extraction Osteomyelitis
April 28, 2023
J Diagn Treat Oral Maxillofac Pathol 2023;7: 33–8.
DOI: 10.23999/j.dtomp.2023.4.1
Under a Creative Commons license
HOW TO CITE THIS ARTICLE
Tymofieiev OO, Fesenko II, Cherniak OS, Serha OO. Ultrasonographic assessment of masseter muscle region and minimally invasive treatment of post-extraction osteomyelitis. J Diagn Treat Oral Maxillofac Pathol 2023;7(4): 33–8. https://doi.org/10.23999/j.dtomp.2023.4.1
NATIONAL REPOSITORY OF ACADEMIC TEXTS
https://nrat.ukrintei.ua/en/searchdoc/2023U000301/
INSTITUTIONAL REPOSITORY
https://ir.kmu.edu.ua/handle/123456789/318
ABSTRACT
Background: Mandibular osteomyelitis is commonly associated with invasive surgery and sequestrectomy. Here, we report a unique case in which it was possible to choose minimally invasive treatment during the exacerbation of osteomyelitis at the stage of sequestrectomy owing to the use of and correct assessment with ultrasonography (USG). This report aimed to present wide possibilities of USG for accurate diagnosis and minimally invasive management of chronic osteomyelitis.
Case Presentation: A 50-year-old woman presented with significant swelling in the left masseteric region, trismus, and severe pain in the area of a previously extracted lower third molar. The imaging protocol included panoramic radiography, USG, and cone-beam computed tomography. Using USG, it was possible to identify the intermediate stage of abscess/phlegmon formation in the masseteric area, which would require an extraoral incision to drain the purulent focus.
Conclusion: USG allows oral and maxillofacial surgeons to obtain a precise understanding of the condition of the tissues (e.g., bone surface, masseter muscle, subcutaneous tissue) and pathologic changes (e.g., periosteal reaction, bony defects) due to purulent processes in the area of the lateral mandibular ramus surface and surrounding soft tissues. The presence of purulent material and its motion on sonopalpation can be clearly identified using USG. Therefore, it is possible to plan for a less invasive surgical strategy.
INTRODUCTION
Mandibular third molar removal is a common procedure in the outpatient clinic; however, complications such as alveolar osteitis postoperatively occur in 30% cases.1 In severe cases, osteitis can progress into chronic purulent osteomyelitis2,3, which makes treatment difficult and long, requiring periodic imaging and drug therapy. The management of mandibular osteomyelitis often involves sequestrectomy, an invasive surgery3. Radiography or computed tomography is typically performed for detailed and appropriate treatment planning in such cases. Considering the growing role and advantages of ultrasonography (USG) in the diagnosis of oral and maxillofacial pathology4,5, especially in infection cases6–8, the application of USG seems to be preferable for the precise localization of pus in osteomyelitis cases.
Here, we report a unique case of a 50-year-old woman with chronic osteomyelitis following an uncomplicated lower third molar removal wherein it was possible to choose minimally invasive treatment during the exacerbation of osteomyelitis at the stage of sequestrectomy owing to the use of and correct assessment with USG. Therefore, this report aimed to present the wide possibilities of USG in accurately identifying the purulent process, enabling minimally invasive management of chronic osteomyelitis.
CASE REPORT
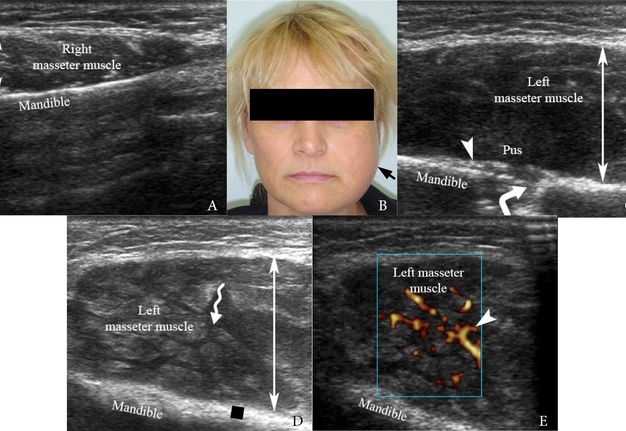
A 50-year-old Caucasian female was referred to our hospital in June 2015 with significant swelling in the left masseteric region (Fig 1), trismus, and severe pain in the tooth socket of a previously extracted lower left third molar. According to the patient, the tooth was removed by a dentist 3 weeks earlier at another clinic because of a partially destroyed crown and periodic night pain. Clinically, painful swelling was noted in the left parotid-masseter region on palpation (Fig 1B). The mouth opening was also painful and limited to 1.0 cm. Intraoral examination revealed purulent discharge from the socket of tooth 3.8 (i.e., the lower left third molar). No comorbidities were reported by patient.
For soft tissue examination, USG was performed using a 12-3 MHz linear transducer (model HD11 XE, Koninklijke Philips N.V., Eindhoven, Netherlands). Gray-scale USG showed the spread of purulent exudate between bundles of fibers of the left masseter muscle, which created a honeycomb patten on USG (Fig 1) (also known as cobblestoned appearance). Sonopalpation (i.e., gentle pressure with the transducer) on gray-scale USG revealed slight motion of the purulent material located between the fibers of the masseter muscle. Ultrasound signs of periosteal reaction and bone defects at the lateral surface of the ramus were noted. Periosteal reaction at the lateral surface of the left ramus was visualized on USG as a thick hyperechoic line compared with a thin hyperechoic band (lateral surface of the right ramus) on the healthy side. On both sides, the artifact of acoustic shadowing was noted distal to the mandibular surface due to the reflective properties of the cortical bone tissue. The diagnostic protocol included USG of both the masseter muscles and rami, the right healthy side, and the left affected side. Color and power Doppler USG revealed hypervascularity in the left masseter muscle. Panoramic radiography (Fig 2A) showed margins of the socket of the removed tooth 3.8, a tortuous area of bone resorption posteriorly, and no radiological signs of the non-removed parts of the tooth. An exacerbation of chronic suppurative post-extraction osteomyelitis of the left ramus mandible was diagnosed.
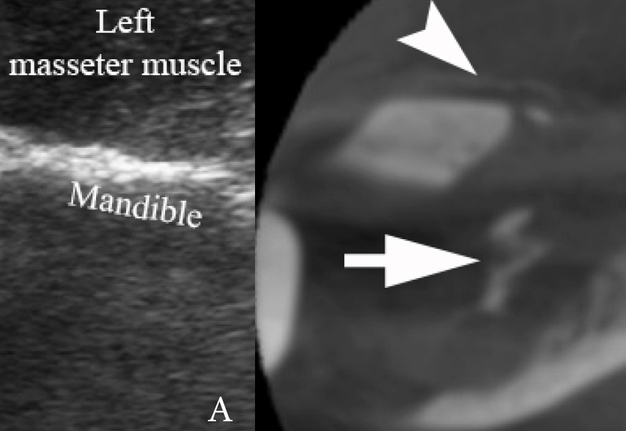
FIGURE 1. (A) Gray-scale USG of the right masseter muscle and ramus (healthy side). Lateral surface of the ramus visualized as a thin hyperechoic line. (B) Clinical photograph shows significant swelling (arrow) in the left masseter region. Up and down arrows show thickness of the right (healthy) and left (involved in purulent inflammation) masseter muscles. (C) Curved arrow indicates cortical bone defect at the lateral surface of left ramus and arrowhead – on periosteal reaction. (D) The spread of purulent exudate (waved arrow, anechoic content) between the bundles of fibers of the left masseter muscle creates a honeycomb USG pattern on gray-scale sonogram. Quadrate labels hyperechoic area (periosteal reaction). (E) Power Doppler USG shows increased masseter muscle vascularity (arrowhead). The soft tissues’ “depth” at the presented cropped sonograms is 3.0 cm.
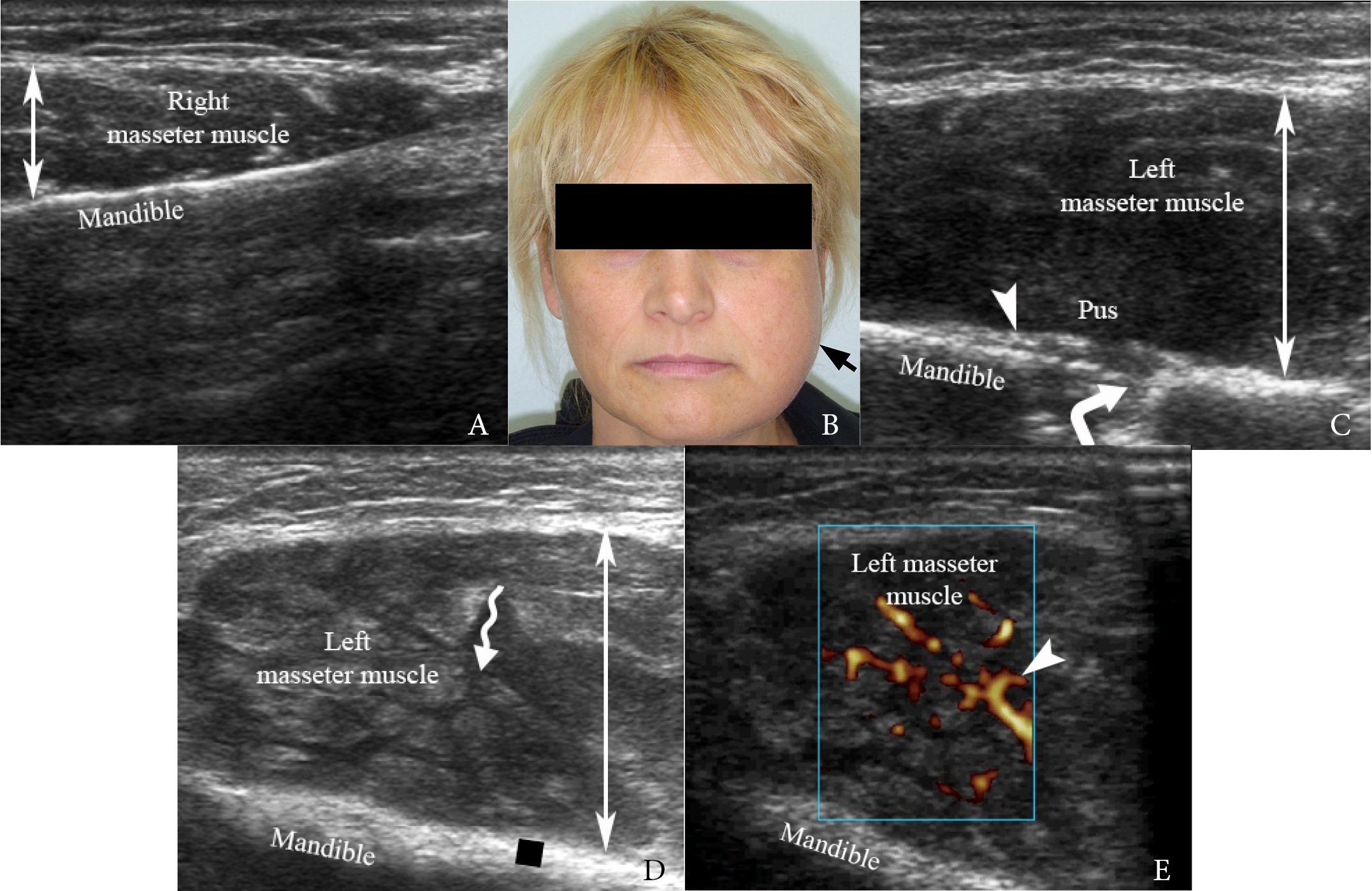
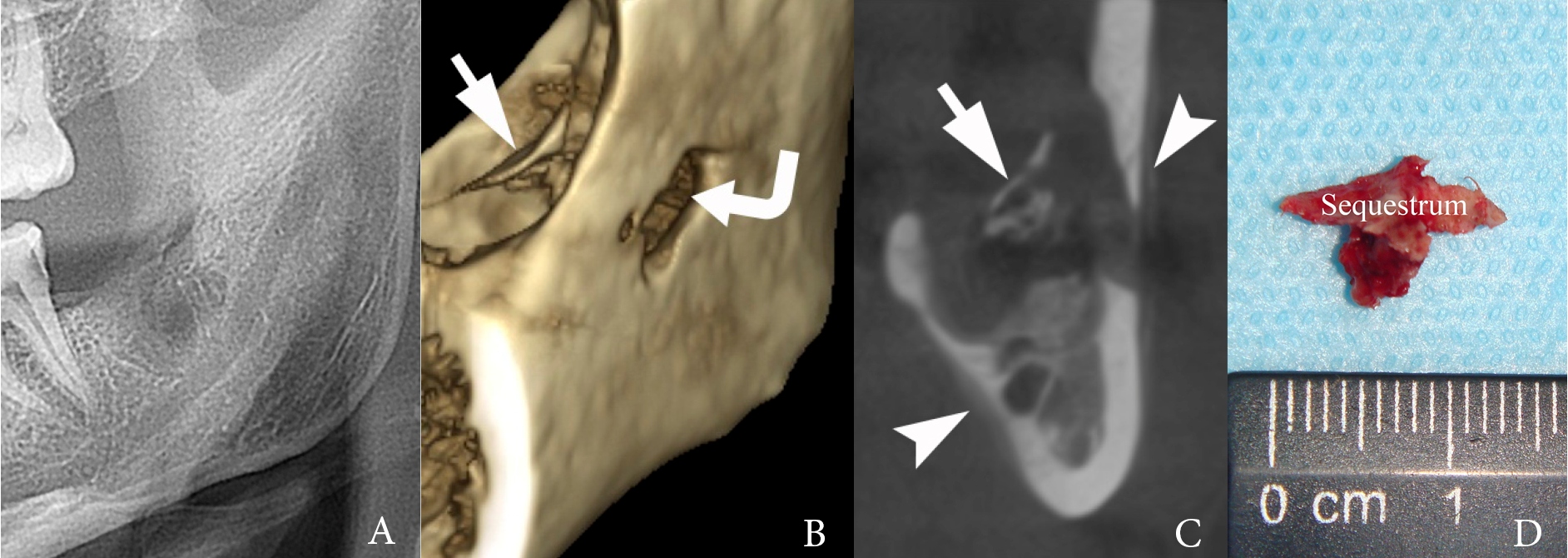
FIGURE 2. (A) Panoramic radiography at the initial hospital visit (day 28 after tooth extraction). (B) Three-dimensional and (C) coronal CBCT scans on day 51 after extraction. Arrow, sequestrum; curved arrow, cortical bone defect; arrowheads, thin periosteal reaction. (D) Removed mandibular sequestrum on day 62 after tooth extraction.
First, local anesthesia, 2.5 mL of 4% Ultracaine® D-S forte (Aventis Pharma Deutschland GmbH, Frankfurt, Germany), using an anesthetic solution in ampules (2.0 mL per ampule) was performed. Then, using a gauze swab, a smear was obtained from the wall of the alveolus for bacteriological examination. The alveolus was washed with 30.0 mL of diluted betadine solution (Betadine® 10%, Egis Pharmaceuticals PLC, Körmend, Hungary) using a pre-broken and bent needle on a 10.0-mL syringe. On irrigation, the tip of the needle was moved to the posterior area of resorption, rotated, and advanced through the area of the cortical bone defect. A significant amount of purulent exudate was removed. The patient was advised to visit our clinic daily for the next 7 days until the purulent discharge, swelling, and other complaints resolved. The following medications were prescribed: cafaxone (Ceftriaxonum) 1.0 g (Lupin Ltd., Mumbai, India) intramuscularly twice daily for 7 days, rinsing the oral cavity with a chlorhexidine solution three times daily for 7 days, Nurofen® non-steroidal anti-inflammatory drug (Reckitt Benckiser Healthcare International Ltd, Slough, England) twice daily for 5 days, and Linex® (Lek Pharmaceuticals d.d., Sandoz, Novartis division, Ljubljana, Slovenia) two capsules three times a day for 7 days.
A comparison of panoramic radiography and cone-beam computed tomography (CBCT) (Planmeca ProMax 3D Max, Planmeca, Finland) performed on days 28 and 51 after tooth removal is presented in Figure 2. CBCT showed a bilobed cortical bone defect measuring 0.52 × 0.9 cm at the lateral surface of the mandible ramus, thin periosteal reaction along the lateral and medial aspects of the mandible, and сlearly formed sequestrum. The density of the periosteal reaction at the lateral surface of the left mandibular ramus varied from 102 to 317 Hounsfield units and was 0.14 cm thick.
Eight weeks after the onset of symptoms, the patient underwent a pre-sequestrectomy evaluation of the local tissues, analysis of the complaints, and planning for the surgery. Swelling or trismus was not observed. The patient reported no pain during the previous week. Intraoral examination revealed improved mouth opening and a healthy color of the soft tissues around the socket of tooth 3.8. The anterior part of the sequestrum was visible in the epithelialized tooth socket. The mandibular sequestrum was removed using a Folkman spoon without premedication and/or anesthesia. The patient did not experience pain or discomfort. Histological examination confirmed the diagnosis. Using USG, it was possible to identify the intermediate stage of abscess/phlegmon formation in the masseteric area, which would require an extraoral incision to drain the purulent focus.
DISCUSSION
Management of third molar pathology requires both accurate imaging9 and appropriate surgical techniques to reduce the likelihood of developing complications and their manifestations10–15. Imaging analysis of the jawbone and condition of neighboring soft tissues requires correct understanding of the anatomy and the pathological effects on anatomical structures. Extensive research (2022) based on dissected formaldehyde-fixed human cadaver heads, computed tomography of fresh cadavers, magnetic resonance data, and histological sections has shown all the three masseter muscle layers—superficial, deep, and coronoid16. Recently published sonographic studies have highlighted the possibilities of non-radiation imaging for pathologies located in masseter muscle7,17. USG proved its usefulness for identifying masseteric area abscesses, phlegmon diagnostics, and drainage of the abscesses7,16,17.
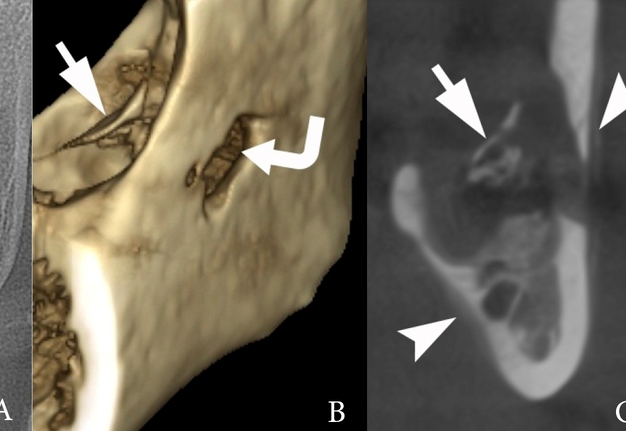
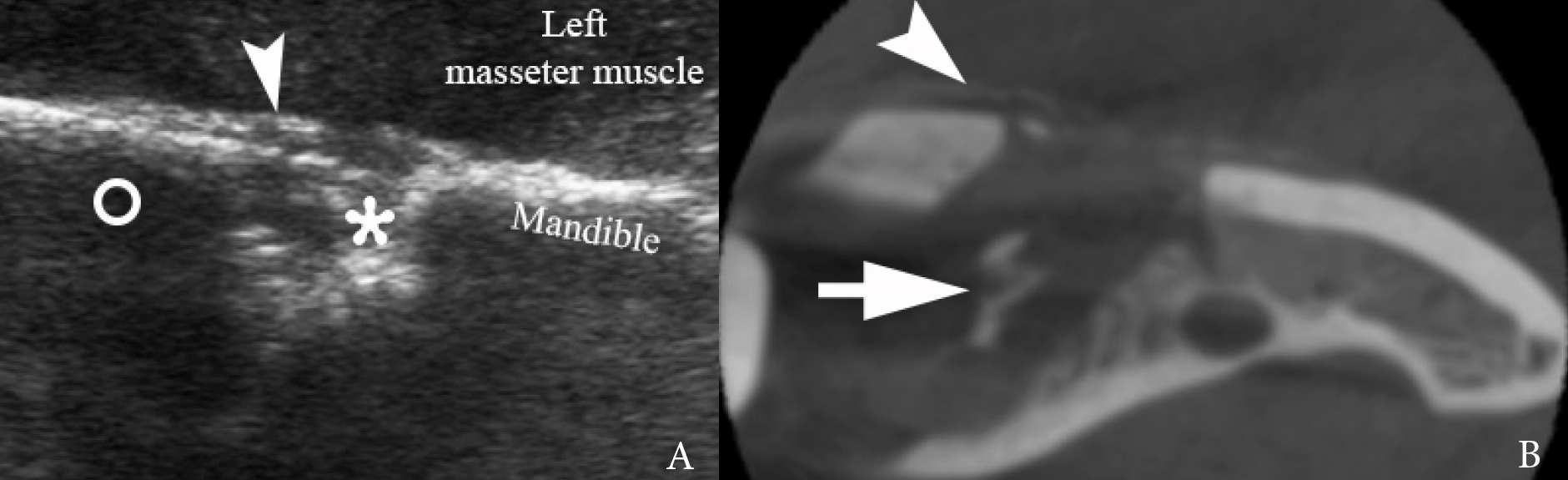
To clarify the diagnostic possibilities of USG18,19 and CBCT20,21 for the analysis of the bone structure, presence of periosteal reaction, and condition of masseter muscle in a case of mandibular osteomyelitis, we compared the gray-scale (i.e., B-mode) sonogram and axial CBCT scan (Fig 3).
FIGURE 3. Left side. Comparing periosteal reaction on (A) gray-scale sonogram and (B) axial CBCT scan at the same location but on different terms of the course of osteomyelitis (USG – on day 28 after tooth extraction and CBCT – on day 51 after tooth extraction). Periosteal reaction (arrowhead) is visualized as thickening and elevation of the periosteum from the underlying lateral cortical bone of the ramus. Intraosseous defect in ramus is indicated by asterisk. A circle labels the artifact of acoustic shadowing posteriorly to the lateral surface of the mandibular ramus. Bone defect of the cortical bone is a place via which the purulent content spread through the periosteum and between fibers of the masseter muscle. Arrow labels sequestrum.
The results suggest that USG depicts a periosteal reaction earlier than plain radiography, indicating underlying bone disorders20. Moreover, USG, a non-radiation imaging technique, can be performed multiple times at all stages of osteomyelitis. Although a relatively similar ultrasound picture (Fig 1C) of the condition was published in another study22, in our case, we conducted a more in-depth examination of the sonographic features of the tissues (in particular, the newly formed periosteal reaction). Comparing our case with other published cases of purulent processes in the area of the masseter muscle and their ultrasound descriptions7,18,19,22,23, it is worth noting that the described cases demonstrate different ultrasound pattern with limited accumulation of purulent material. The ultrasound images showing the spread of pus between the fibers of the masseter muscle and the minimally invasive treatment presented in this article are unique among other scientific studies.
USG is highly recommended for oral and maxillofacial surgeons as a first-line imaging technique for the detection and assessment of purulent processes in the masseter muscle region. Thus, the sonographic assessment of the masseter muscle and other tissues involved in the purulent process allows for a correct diagnosis and, in some cases, avoidance of extraoral incisions and more invasive treatment procedures. USG, including sonopalpation, being a dynamic imaging technique, in contrast to static CBCT imaging, provides more benefit to the treating team in diagnostics.
CONCLUSIONS
In summary, diagnostic ultrasound allows oral and maxillofacial surgeons to obtain a precise understanding of the condition of the tissues (e.g., bone surface, masseter muscle, subcutaneous tissue) and pathologic changes (e.g., periosteal reaction, bony defects) due to purulent processes in the area of the lateral mandibular ramus surface and surrounding soft tissues. The presence of purulent material and its motion on sonopalpation can be clearly identified using USG. Such precise diagnosis makes it possible to opt for a less invasive surgical approach, such as in the current case of post- extraction osteomyelitis of the mandible.
AUTHORS CONTRIBUTION STATEMENT
OOT and IIF drafted the manuscript. IIF participated in patient management. All authors participated in the data collection and analysis. IIF and OSC contributed to figure preparation. All authors have contributed to the manuscript and approved the submitted version.
TRANSPARENCY DECLARATION
This work was unfunded. The authors have no conflicts of interest to disclose.
REFERENCES (23)
-
Hatab N, Yahya J, Alqulaihi S. Management of alveolar osteitis in dental practice: a literature review. J Diagn Treat Oral Maxillofac Pathol 2017;1(3−4):147−55. https://doi.org/10.23999/j.dtomp.2017.34.7
-
Schoen R, Suarez-Cunqueiro MM, Metzger MC, Schmelzeisen R. Osteomyelitis of the mandible following third molar surgery: a regrettable consequence in a healthy patient. Quintessence Int 2009; 40(5):351−4.
-
Humber CC, Albilia JB, Rittenberg B. Chronic osteomyelitis following an uncomplicated dental extraction. J Can Dent Assoc 2011;77:b98.
-
Demidov VH, Cherniak OS, Snisarevskyi PP, et al. Schwannoma of the tongue: ultrasonography. J Diagn Treat Oral Maxillofac Pathol 2022;6(11):138–47. https://doi.org/10.23999/j.dtomp.2022.11.2
-
Savchuk LA, Nozhenko OA. Foreign body retrograde migration to the intraglandular duct of the submandibular gland with a developing of foreign body-induced sialolithiasis: analysis of ultrasonography, surgery, and literature published during last 124 years. J Diagn Treat Oral Maxillofac Pathol 2020;4(3):53–9. https://doi.org/10.23999/j.dtomp.2020.3.2
-
Tymofieiev OO, Ushko NO, Fesenko II, et al. Suppurative mastoid lymphadenitis mimicking mastoiditis: a case report. J Korean Assoc Oral Maxillofac Surg 2021;47(5):398–402. https://doi.org/10.5125/jkaoms.2021.47.5.398
-
Cherniak OS, Ripolovska OV, Nozhenko OA, Fesenko II. Accuracy of ultrasound in diagnostics of odontogenic infection in layers of temporal and parotid masseter region. J Diagn Treat Oral Maxillofac Pathol 2019;3(9):214−29. https://doi.org/10.23999/j.dtomp.2019.9.2
-
Borodavko DS, Abramenko AV, Borodavko SP, et al. Analysis of a first unilateral and then bilateral internal jugular vein thrombosis in a heroin user. J Diagn Treat Oral Maxillofac Pathol 2019;3(10):234−55. https://doi.org/10.23999/j.dtomp.2019.10.2
-
Babkina TM, Shekera OG, Storozhchuk YO, et al. Gigantic dentigerous cysts associated with the ectopic/impacted upper third molars: computed tomography analysis of nasolacrimal duct and osteomeatal complex obstructions and review of literature. J Diagn Treat Oral Maxillofac Pathol 2020;4(5):79–94. https://doi.org/10.23999/j.dtomp.2020.5.1
-
Ciantar M, Adlam DM. Treatment with infliximab: implications in oral surgery? A case report. Br J Oral Maxillofac Surg 2007;45(6):507−10. https://doi.org/10.1016/j.bjoms.2006.06.004
-
Silva TCG, Maranhão Filho AWA, Alencar MGM, et al. Mandibular fracture after third molar removal: a case report. Gen Dent 2019;67(4):e7−e10.
-
Kvolik Pavić A, Zubčić V. Osteomyelitis of the jaw in COVID-19 patients: a rare condition with a high risk for severe complications. Front Surg 2022;9:867088. https://doi.org/10.3389/fsurg.2022.867088
-
Tymofieiev OO. Removal of the teeth [Ukrainian]. In: Tymofieiev OO, editor. Maxillofacial surgery. Kyiv: Medicine VSV; 2011. p. 105−43.
-
Susarla SM, Blaeser BF, Magalnick D. Third molar surgery and associated complications. Oral Maxillofac Surg Clin North Am 2003;15(2):177−86. https://doi.org/10.1016/S1042-3699(02)00102-4
-
Christidis N, Al-Moraissi EA. Editorial: orofacial pain of muscular origin-from pathophysiology to treatment. Front Oral Health 2022;2:825490. https://doi.org/10.3389/froh.2021.825490
-
Mezey SE, Müller-Gerbl M, Toranelli M, Türp JC. The human masseter muscle revisited: first description of its coronoid part. Ann Anat 2022;240:151879. https://doi.org/10.1016/j.aanat.2021.151879
-
Qin F, Zhang X, Zhang J, et al. Masseter muscle metastasis of renal cell carcinoma: a case report and literature review. Front Oncol 2022;12:830195. https://doi.org/10.3389/fonc.2022.830195
-
Al-Belasy FA. Ultrasound-guided drainage of submasseteric space abscesses. J Oral Maxillofac Surg 2005;63(1):36−41. https://doi.org/10.1016/j.joms.2004.05.218
-
Gudi SS, Sarvadnya J, Hallur N, Sikkerimath BC. Ultrasound guided drainage of submasseteric space abscesses. Ann Maxillofac Surg 2013;3(1):31−4. https://doi.org/10.4103/2231-0746.110074
-
Moraux A, Gitto S, Bianchi S. Ultrasound features of the normal and pathologic periosteum. J Ultrasound Med 2019;38(3):775−84. https://doi.org/10.1002/jum.14762
-
Ida M, Tetsumura A, Kurabayashi T, Sasaki T. Periosteal new bone formation in the jaws. A computed tomographic study. Dentomaxillofac Radiol 1997;26(3):169−76. https://doi.org/10.1038/sj.dmfr.4600234
-
Mallorie CN, Jones SD, Drage NA, Shepherd J. The reliability of high resolution ultrasound in the identification of pus collections in head and neck swellings. Int J Oral Maxillofac Surg 2012;41(2):252−5. https://doi.org/10.1016/j.ijom.2011.10.012
-
Muthyala S, Krishna KV, Kishan TV, et al. Masseteric cysticercosis with abscess formation: a diagnostic dilemma. Med J Armed Forces India 2015;71(Suppl 1):S148−S151. https://doi.org/10.1016/j.mjafi.2013.09.008