An Unusual Presentation of a Neck Mass – Traumatic Pseudoaneurysm Following Third Molar Surgery: A Case Report
August 13, 2023
J Diagn Treat Oral Maxillofac Pathol 2023;7: 87–93.
DOI: 10.23999/j.dtomp.2023.8.1
Under a Creative Commons license
HOW TO CITE THIS ARTICLE
Dammling C, Le JM, Aljadeff L, Jones JGA, Ogilvie M, Morlandt AB. An unusual presentation of a neck mass – traumatic pseudoaneurysm following third molar surgery: a case report. J Diagn Treat Oral Maxillofac Pathol 2023;7(8):87–93. https://doi.org/10.23999/j.dtomp.2023.8.1
NATIONAL REPOSITORY OF ACADEMIC TEXTS
https://nrat.ukrintei.ua/en/searchdoc/2023U000205/ (in English). https://nrat.ukrintei.ua/searchdoc/2023U000205/ (in Ukrainian).
ABSTRACT
Traumatic pseudoaneurysm (TPA) is an extremely rare complication following a tooth extraction. TPAs are vascular lesions that occur due to extravasated blood that is still contained by the adventitia or adjacent soft tissue. This sac of blood may continue to expand, leading to superimposed infection, severe hemorrhage, or thromboembolism. In the maxillofacial region, TPA is most often associated with penetrating trauma, condylar fractures, or orthognathic surgery and can present days to weeks following the inciting event. The purpose of this paper is to review the management of a rare facial artery TPA following routine mandibular third molar tooth extraction in a 19-year-old healthy male. A computed tomography angiography and color Doppler ultrasound were used for diagnosis of the TPA. The initial treatment involved endovascular embolization followed by surgical excision due to the delayed appearance of a large 3-cm upper neck mass. While TPA is a rare complication following third molar surgery, we report the first case presenting to the head and neck surgeon as a unilateral neck mass following definitive endovascular therapy.
KEY WORDS
Traumatic pseudoaneurysm, dentoalveolar surgery, maxillofacial complications, endovascular embolization, third molar surgery, neck mass, cervical pathology
INTRODUCTION
Third molar surgery, also known as wisdom tooth extraction, is one of the most common procedures performed by the oral and maxillofacial surgeon with a generally low complication rate.1-3 Adverse events most often include infection, alveolar osteitis, bleeding, or swelling.3 Less common complications include paresthesia, mandibular fracture and displacement of teeth or instruments. Traumatic pseudoaneurysm (TPA) formation is an extremely rare complication which has been reported in the literature as a potential sequela following tooth extraction.3-11 In the maxillofacial region, TPA is most often associated with penetrating trauma, condylar fractures, and orthognathic surgery and involves the branches of the internal maxillary artery.3,4 TPA occurs when there is disruption in the vascular endothelium followed by blood extravasation into the adventitia or adjacent soft tissue. The resulting collection of blood may continue to expand, leading superimposed infection, severe hemorrhage, or thromboembolism. These lesions lack an intact muscularis layer and are surrounded by a weak connective tissue pseudocapsule. Management can involve both surgical and endovascular treatments. Minimally invasive catheter-based embolization is the favored technique as it avoids the morbidity of an open surgical procedure.12 In this case report, we review the current diagnostic imaging modalities and endovascular treatment paradigm for traumatic pseudoaneurysm of the facial artery following third molar tooth extraction. Several months following a catheter-based embolization procedure, the patient underwent surgical excision of the organized thrombus which presented as a well-lateralized level II neck mass.
CASE SUMMARY
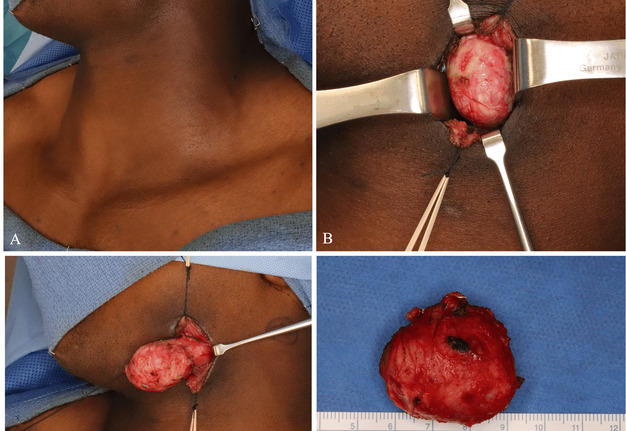
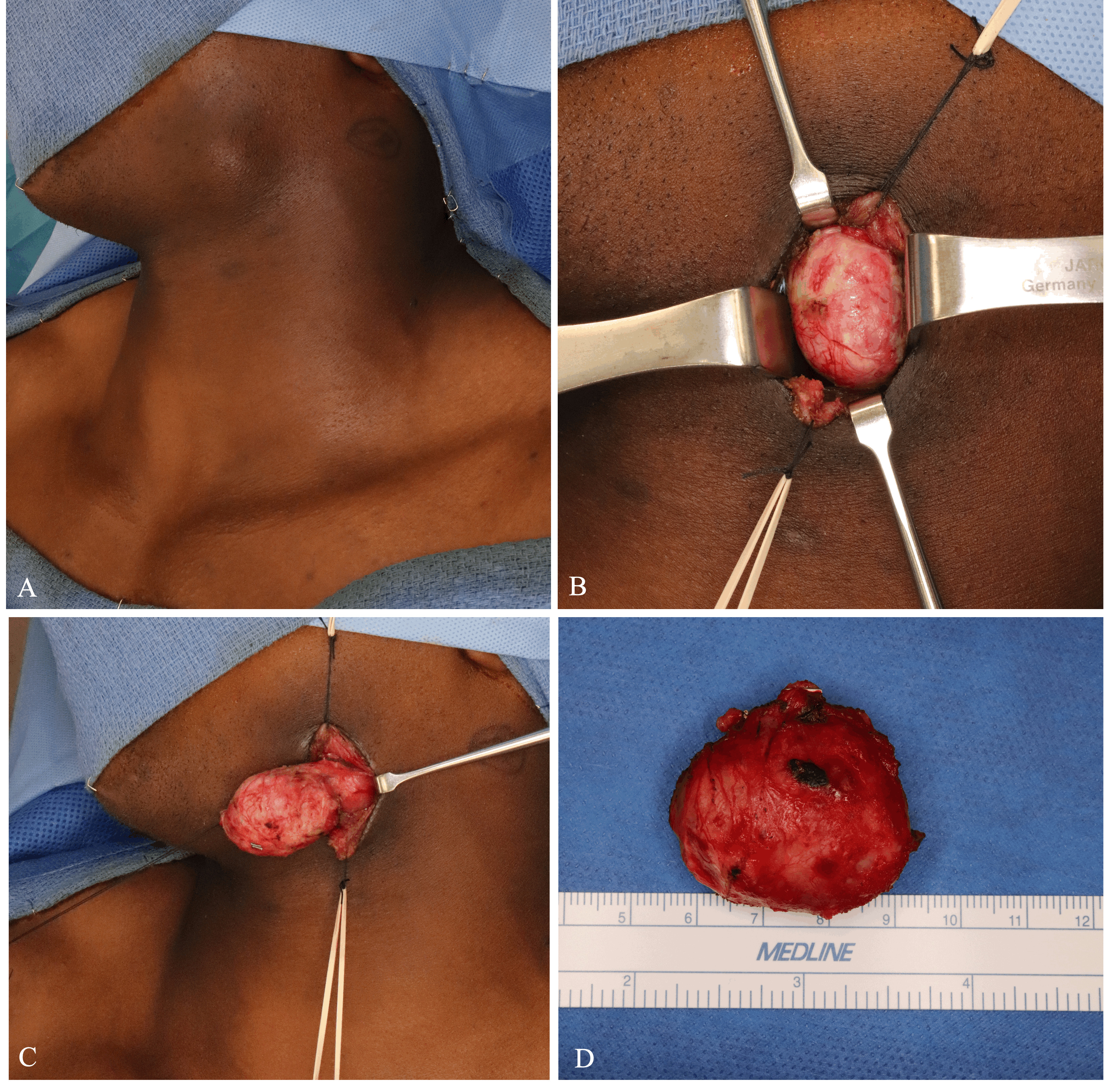
A 19-year-old male with no significant medical history presented to our clinic for evaluation of firm, non-pulsatile, and non-painful mass at the left angle of the mandible that had been present for 3 months (Fig 1). Upon further investigation, the patient recalled having a routine and uneventful third molar tooth extraction several months prior. He developed acute neck swelling shortly thereafter and sought medical attention at a nearby emergency department.
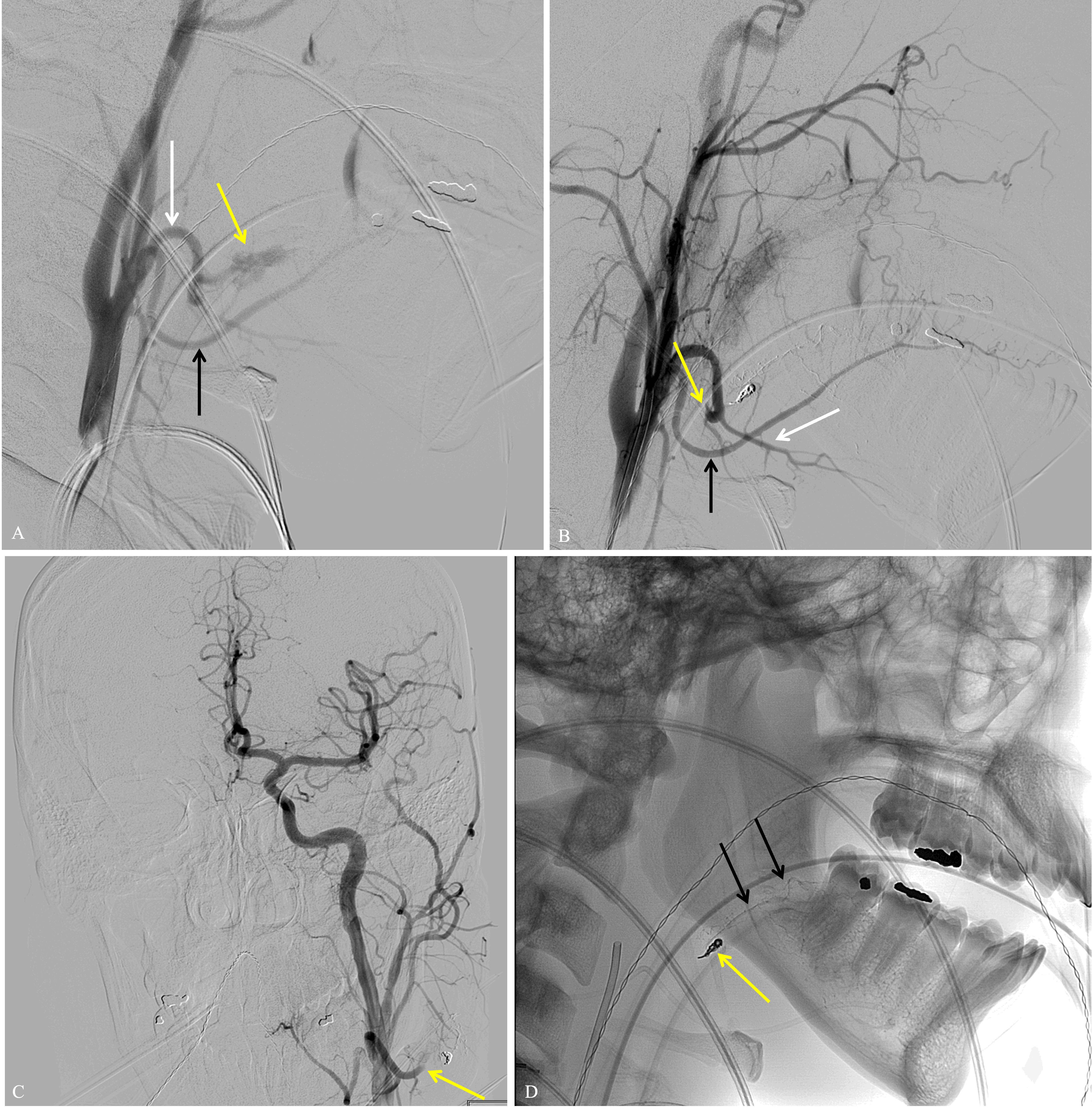
A computed tomography angiography (CTA) demonstrated a 3-cm left-sided facial artery pseudoaneurysm containing arterial blood and thrombus (Fig 2A and 2B). Ultrasound with color Doppler showed turbulent bidirectional blood flow in a “yin-yang” pattern highly suggestive of TPA (Fig 2C). Following a thorough discussion of the risks and benefits of embolization, the Interventional Neuroradiology service then treated the patient with endovascular therapy. A 5-french sheath (Terumo, Somerset, NJ) was placed into the right radial artery under ultrasound guidance. An anti-spasmodic cocktail of nitroglycerin, heparin and verapamil was given intra-arterially. A left common carotid artery angiogram confirmed the TSA arising from a 2nd order branch of the facial artery (Fig 3A). A microcatheter (Echelon 10, Medtronic, Minneapolis, MN) was then advanced into the left external carotid and facial arteries and a super selective angiogram performed. With the microcatheter tip just proximal to the TPA, an embolization coil (Axium, EV3 Neurovascular, Irvine, CA) was detached at its orifice. Next, a liquid embolic (Trufill, Cerenovus, Irvine, CA) admixed 1:1 with lipiodol was infused around the coil to completely occlude arterial inflow to the TSA (Fig 3D).
FIGURE 2. Computed tomography angiography of axial (A) and coronal (B) views of the 3-cm pseudoaneurysm (yellow arrow) located at the left mandibular angle and a color Doppler ultrasound (C) of the mass demonstrating “yin-yang” pattern (yellow arrow) consistent with a partially thrombosed pseudoaneurysm.
An immediate post-embolization angiogram demonstrated facial artery occlusion distal to the submental branch, at the proximal aspect of the TSA. However, the facial artery reconstituted distally by way of its anastomosis with the lingual artery, and this allowed minimal delayed filling of the TSA in retrograde fashion (Fig 3B and 3C). The patient was discharged home the same day and instructed to perform manual compression of the TSA twice daily for 20 minutes at a time to help ensure thrombosis.
FIGURE 3. (A) Lateral digital subtraction angiogram (DSA) from the left common carotid artery demonstrating pseudoaneurysm (yellow arrow) coming off the 2nd order branch of the facial artery (white arrow). The lingual artery in inferior to the facial artery (black arrow). (B) Post-embolization DSA demonstrating successful cessation of flow in 2nd order facial artery and pseudoaneurysm and preservation of flow in the other 2nd order branch off facial artery, submental artery (white arrow). The lingual artery is inferior (black arrow). (C) Anterior-to-posterior DSA demonstrating normal cerebral angiogram and successful 2nd order facial artery embolization (yellow arrow). (D) Lateral radiograph post embolization demonstrating coil pack (yellow arrow) and glue in adjacent 3rd order facial artery branches (black arrows) in region of wisdom tooth extraction.
At 1-month clinic follow-up, the patient denied any further pulsatile symptoms or bleeding although noted slight facial asymmetry around the previous pseudoaneurysm (Fig 4A). Two months later, the patient presented to the Oral Oncology service complaining of a painless left upper neck mass. Computed tomography demonstrated a well-circumscribed, scarred mass in the region of the previous pseudoaneurysm. Under general anesthesia, a horizontal incision was made in a natural skin crease directly overlying the lesion. Subplatysmal flaps were elevated, and the lesion was identified under the superficial layer of the deep cervical fascia (Fig 4B). Both superior and inferior to the lesion, several feeder branches of the external carotid system were identified, suture ligated, and divided. The lesion was then dissected from the mylohyoid and posterior belly of the digastric muscles and excised (Fig 4C and 4D). The patient tolerated the procedure well and had an uneventful postoperative course. He was content with both functional and cosmetic outcomes.
DISCUSSION
TPA in the maxillofacial region is extremely rare and has been reported to occur following penetrating trauma, condylar fractures, orthognathic surgery, and dental extractions. The mandibular portion of the internal maxillary artery is at frequent risk of injury with subcondylar fractures due to its close approximation with the condylar neck. During orthognathic surgery, both the facial artery and descending palatine arteries are at risk for TPA formation due to the proximity of these vessels to the osteotomy sites.13 TPA related to dental extractions have been reported to occur at the lingual artery, internal maxillary artery, facial artery, and inferior alveolar artery.3,6-10,14,15 When there is clinical concern for the occurrence of a TPA, a CTA remains the preferred diagnostic modality for initial evaluation.11 However, when a CTA cannot be obtained, the utilization of ultrasonography and color Doppler can also verify a pseudoaneurysm with the visualization of bidirectional blood flow as shown in this case.
The inferior alveolar branch of the internal maxillary artery provides vascular supply to the mandible and dentition via the mandibular foramen and more commonly associated with injury following dentoalveolar surgery. Meanwhile, injury to the facial artery, as described in this case report, is much less common and may relate to excessive lateral dissection during flap elevation for mandibular third molars. In addition, the anastomoses between the facial and inferior alveolar arteries via mylohyoid and submental branches should also be evaluated at the time of catheter angiography when vessel injury is suspected.16
Treatment for TPA most commonly involves endovascular therapy with interventional radiology. Endovascular treatments for TPA are diverse and include gel foam, cyano-acrylate, ethylene vinyl alcohol (EVOH), coils, particles, and ethanol. Acute complications associated with endovascular treatment can include facial palsy, stroke, or central retinal artery occlusion due to thromboembolic events.11 Small TSAs may be saturated with liquid embolic to prevent retrograde filling. However, the same technique is impractical for large TPA as the embolic will harden and result in a palpable mass. In most scenarios, the arterial segment distal to the TPA cannot be catheterized and so proximal inflow alone is occluded. In some cases, like the one presented here, retrograde filling may occur and oppose complete thrombosis. The authors recommend daily manual compression to counteract this occurrence and hasten resolution. Additional surgery may be indicated to remove the residual thrombus, which may present clinically as a mass that can be unaesthetic as shown in this case.
CONCLUSION
In this case, a TPA that had occurred following routine third molar surgery initially presented to our clinic as a unilateral neck mass. Initially, the TPA was treated by endovascular coil embolization with complete resolution, and the residual organized thrombus mass was completely excised 2 months later to correct the patient’s facial deformity. While TPA in the maxillofacial region following routine third molar surgery is an uncommon complication, early recognition using diagnostic imaging followed by treatment collaboration with neuroradiology is essential in preventing more serious complications.
ACKNOWLEDGEMENTS
Not applicable.
AUTHORS’ CONTRIBUTIONS
All authors made substantial contributions to the conception, design of the study, analysis and interpretation, composition of the manuscript, and final approval of the manuscript.
FINANCIAL SUPPORT AND SPONSORSHIP
None.
CONFLICTS OF INTEREST
All authors declared that there are no conflicts of interest.
CONSENT FOR PUBLICATION
The author declares that signed Informed Consents were obtained for publication of patient’s images in this manuscript.
REFERENCES (16)
-
Bui CH, Seldin EB, Dodson TB. Types, frequencies, and risk factors for complications after third molar extraction. J Oral Maxillofac Surg 2003;61(12):1379–89. https://doi.org/10.1016/j.joms.2003.04.001
- Rafetto LK, Synan W. Surgical management of third molars. Atlas Oral Maxillofac Surg Clin North Am2012;20(2):197–223. https://doi.org/10.1016/j.cxom.2012.07.002
- Heifetz-Li JJ, Abdelsamie S. Pseudoaneurysm following “routine” third molar extraction: a case report and review of the literature. Oral Maxillofac Surg Cases 2022;8(1):100249. https://doi.org/10.1016/j.omsc.2022.100249
- Pukenas BA, Albuquerque FC, Pukenas MJ, et al. Novel endovascular treatment of enlarging facial artery pseudoaneursym resulting from molar extraction: a case report. J Oral Maxillofac Surg 2012;70(3):e185–e189.https://doi.org/10.1016/j.joms.2011.10.031
- Stiefel MF, Park MS, McDougall CG, et al. Endovascular treatment of hemorrhagic alveolar artery pseudoaneurysm after tooth extraction: a case report. J Oral Maxillofac Surg 2010;68(9):2325–8.https://doi.org/10.1016/j.joms.2009.12.011
- Koga M, Toyofuku S, Aoki M, et al. Use of transcatheter arterial embolization to treat a case of massive arterial bleeding caused by a traumatic aneurysm developing after tooth extraction (Japanese). Jpn J Oral Maxillofacial Surg 2005;51(1):63–6. https://doi.org/10.5794/JJOMS.51.63
- De Lucas EM, Gutierrez A, Gonzalez Mandly A, et al. Life-threatening pseudo-aneurysm of the facial artery after dental extraction: successful treatment with emergent endovascular embolization. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;106(1):129–32. https://doi.org/10.1016/j.tripleo.2007.09.031
- Salgarelli A, Morana G, Beltramello A, Nocini PF. Pseudoaneurysm of the lingual artery: a case report. J Oral Maxillofac Surg 1997;55(8):860–4. https://doi.org/10.1016/s0278-2391(97)90351-7
- Marco de Lucas E, Gutiérrez A, González Mandly A, et al. Life-threatening pseudoaneurysm of the facial artery after dental extraction: successful treatment with emergent endovascular embolization. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;106(1):129–32. https://doi.org/10.1016/j.tripleo.2007.09.031
- Rayati F, Parsa H, Abed PF, Karagah T. Facial artery pseudoaneurysm following surgical removal of a mandibular molar. J Oral Maxillofac Surg 2010;68(7):1683–5. https://doi.org/10.1016/j.joms.2009.07.078
- Rawat SK, Singh D, Suresh Babu P, George R, Mongia P. Traumatic pseudoaneurysm: a life-threatening complication after surgical extraction of impacted maxillary third molar. J Maxillofac Oral Surg 2019;18(1):57–60. https://doi.org/10.1007%2Fs12663-018-1118-z
- Bianchi B, Verazzani, A, Ferri A, et al. Endovascular embolization for the management of inferior alveolar artery bleeding after a third molar extraction: a case report. Quintessence Int 2016;47(3):227–31. https://doi.org/10.3290/j.qi.a35261
- Jo HW, Kim YS, Kang DH, et al. Pseudoaneurysm of the facial artery occurred after mandibular sagittal split ramus osteotomy. Oral Maxillofac Surg 2013;17(2):151–4. https://doi.org/10.1007/s10006-012-0339-4
- Sagara Y, Kiyosue H, Tanoue S, et al. Selective transarterial embolization with n-butyl-2-cyanoacrylate for the treatment of arterial hemorrhage after third molar extraction. Neuroradiology 2013;55(6):725–32. https://doi.org/10.1007/s00234-013-1158-5
- Wasson M, Ghodke B, Dillon JK. Exsanguinating hemorrhage following third molar extraction: report of a case and discussion of materials and methods in selective embolization. J Oral Maxillofac Surg 2012;70(10):2271–5. https://doi.org/10.1016/j.joms.2012.03.003
- Harrigan M, Deveikis J, Essential neurovascular anatomy. In: Harrigan M, Deveikis J, editors. Handbook of cerebrovascular disease and neurointerventional technique. 3rd edition. Cham, Switzerland: Springer International Publishing, 2018; pp. 3–98. https://doi.org/10.1007/978-1-61779-946-4