Buccal Plate Preservation at Anterior Maxilla Using Immediate Implant Placement With a 2.0 mm Gap Technique Based on Spontaneous Bone Healing: Case Report
December 25, 2018
https://doi.org/10.23999/j.dtomp.2018.4.2
J Diagn Treat Oral Maxillofac Pathol 2018;2:151−4.
Under a Creative Commons license
How to cite this article
Nagorniak KY, Nagorniak IV. Buccal plate preservation at anterior maxilla using immediate implant placement with a 2.0 mm gap technique based on spontaneous bone healing: case report. J Diagn Treat Oral Maxillofac Pathol 2018;2(4):151−4.
Contents: Summary | Introduction | Case Presentation | Discussion | Results | Conclusions | Conflict of Interest | Role of the Co-Authors | Ethical Approval | Term of Consent | Fundings | References (12)
Summary
Gap (synonyms: jumping distance, bone gap) between the implant surface and surrounding bone upon the immediate implant placement can be used for buccal plate preservation. Our case report revised a ITI and Neves et al (2013) [6, 7] recommendations. Finally, case report in a 32-year-oldpatient confirms a good spontaneous bone healing and successful osseointegration in a situation of 2 mm gap between immediate implant allowing preserving a buccal plate.
Introduction
A space that can be seen between the implant surface and surrounding bone upon the immediate implant placement is called a gap (synonyms: jumping distance, bone gap) [1, 2]. A gap (Mehta and Shah, 2015) can occur on any aspect of an immediately placed dental implant: buccal, lingual or proximally [1]. To avoid soft tissues recession in aesthetic zone of anterior maxilla is extremely important to preserve buccal plate in the rehabilitation of patients [3-6]. Because of thin buccal plate in that zone we should pay attention to the plate preservation. As buccal plate resorption is a main reason of soft tissue recession [1, 4]. The purpose of that report is to highlight the technique of immediate implant placement achieving 2.0 mm distance between implant and buccal plate surfaces that allow to obtain a spontaneous bone healing and to preserve buccal plate what reduces a risk of soft tissues recession [7-12].
Case Presentation
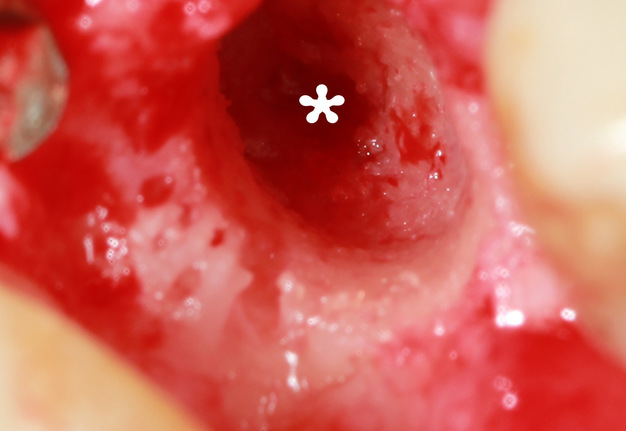
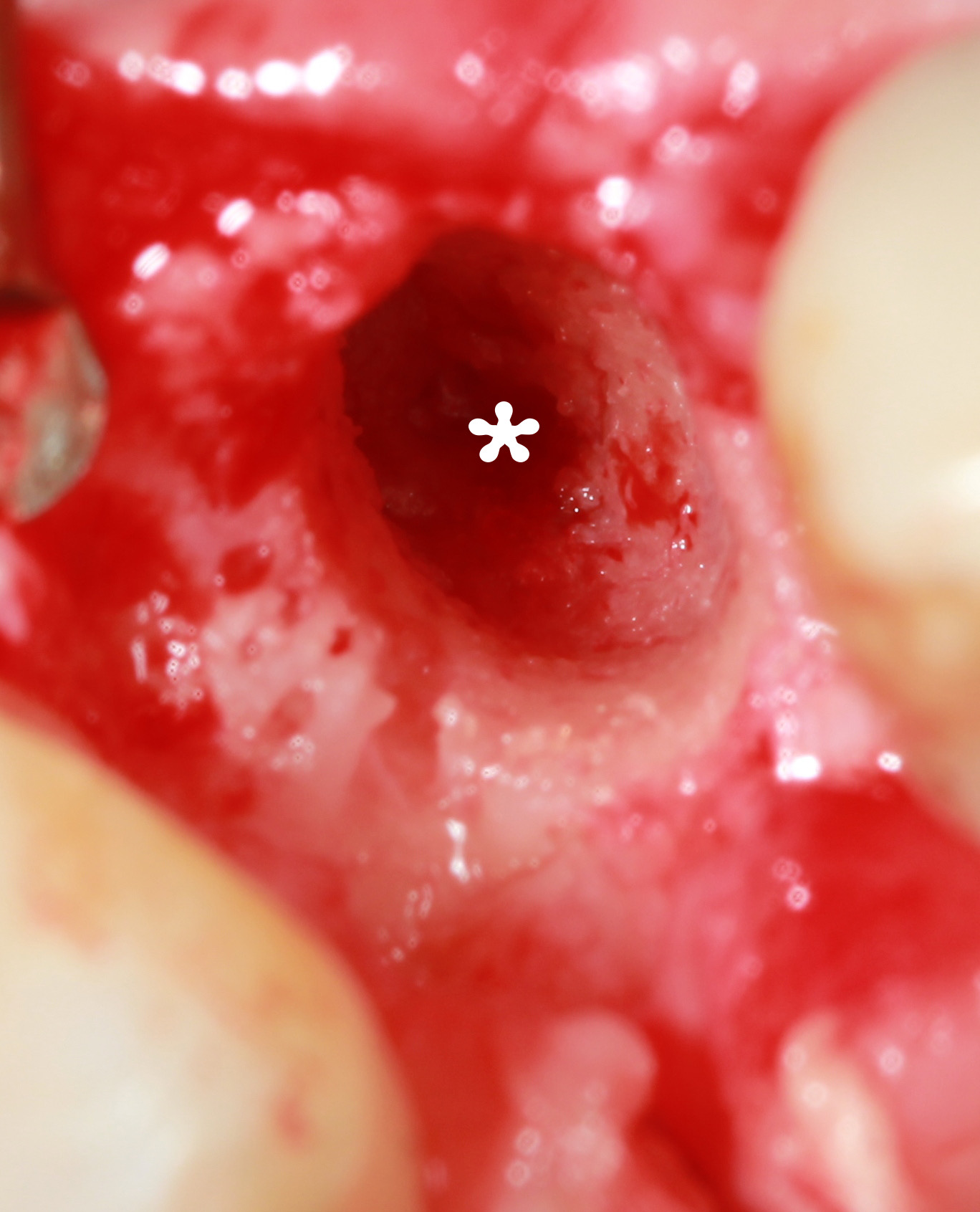
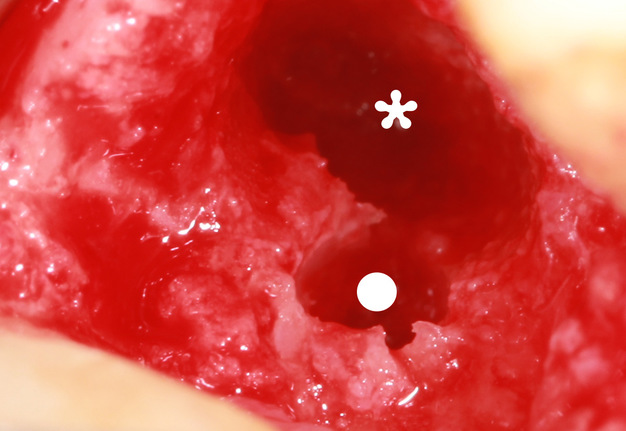
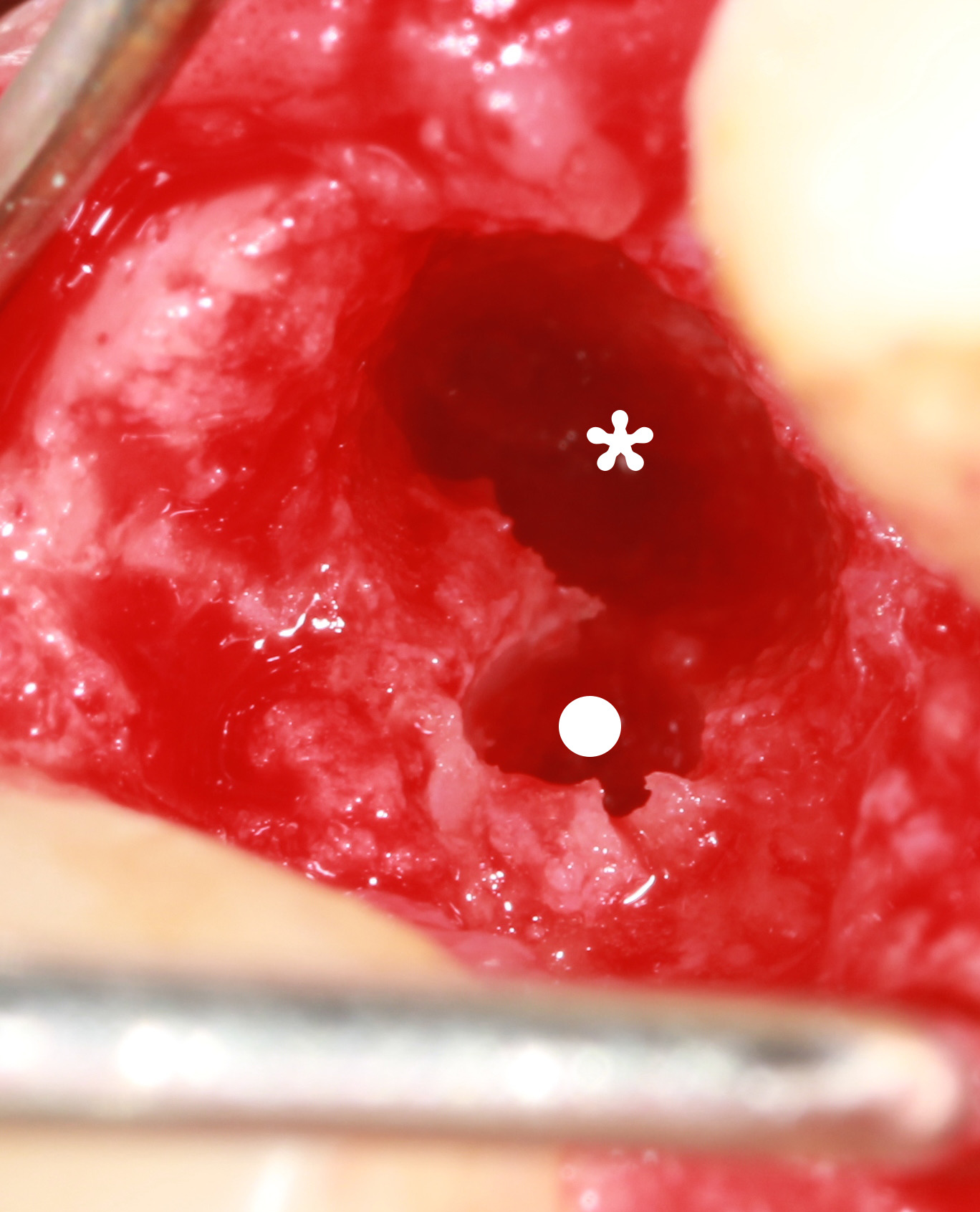
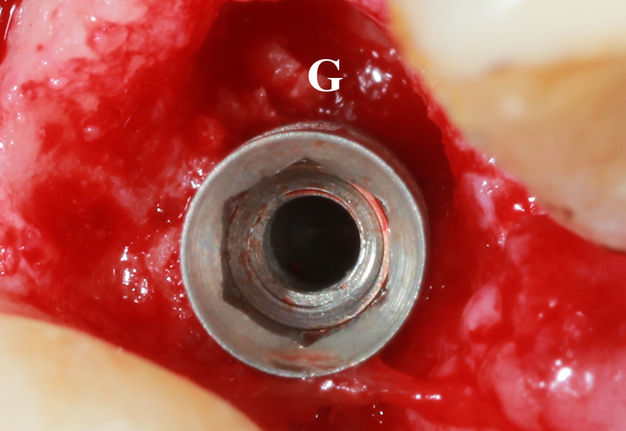
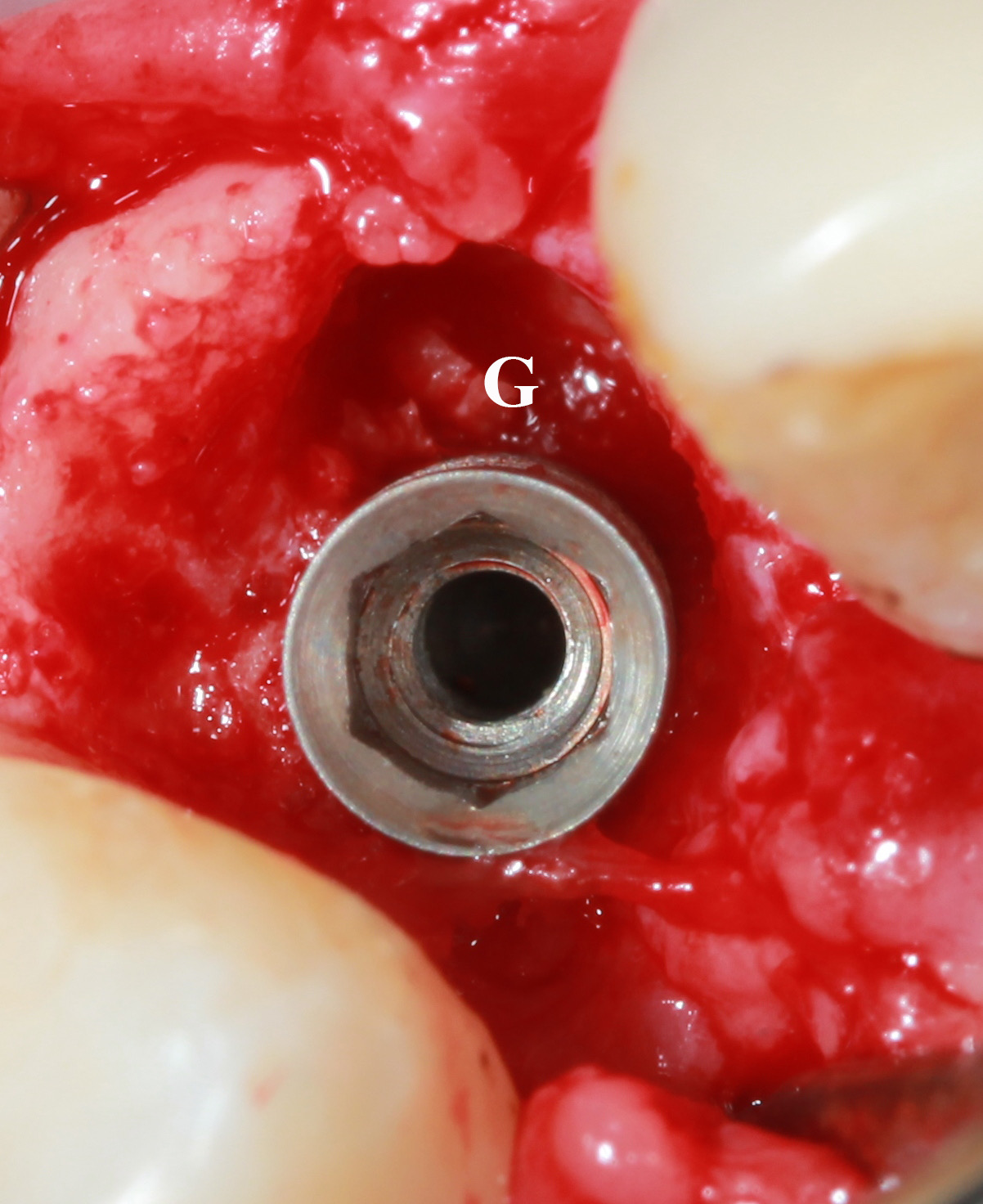
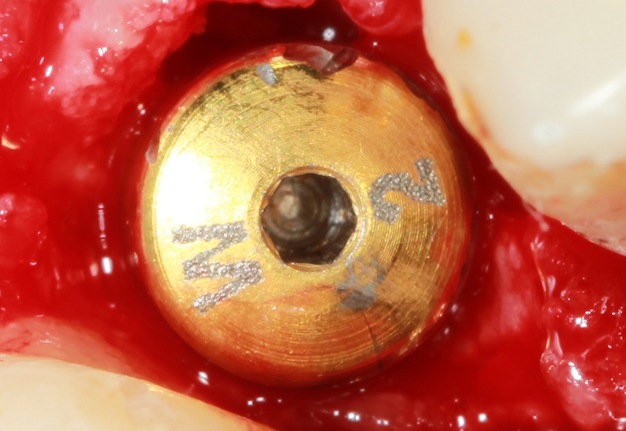
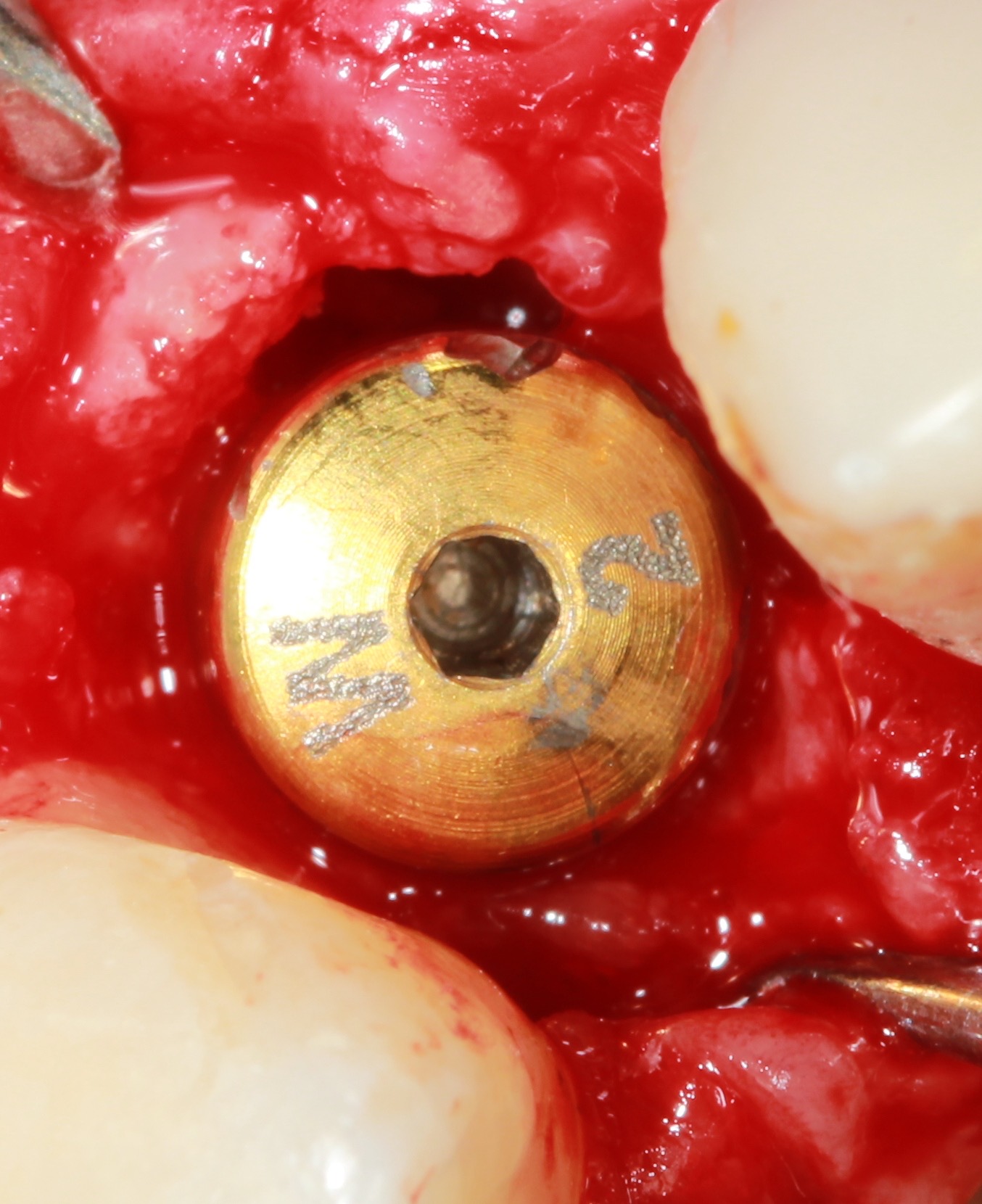
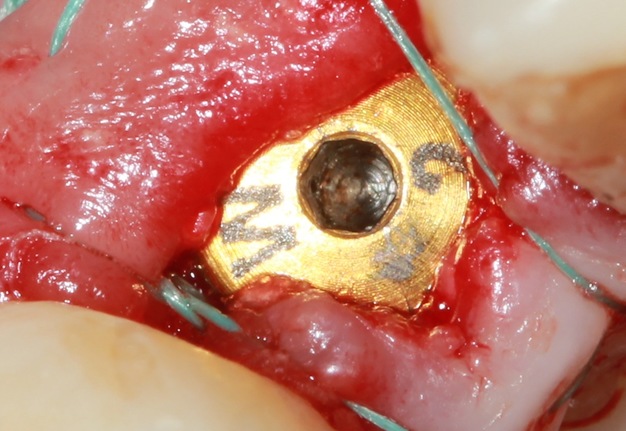
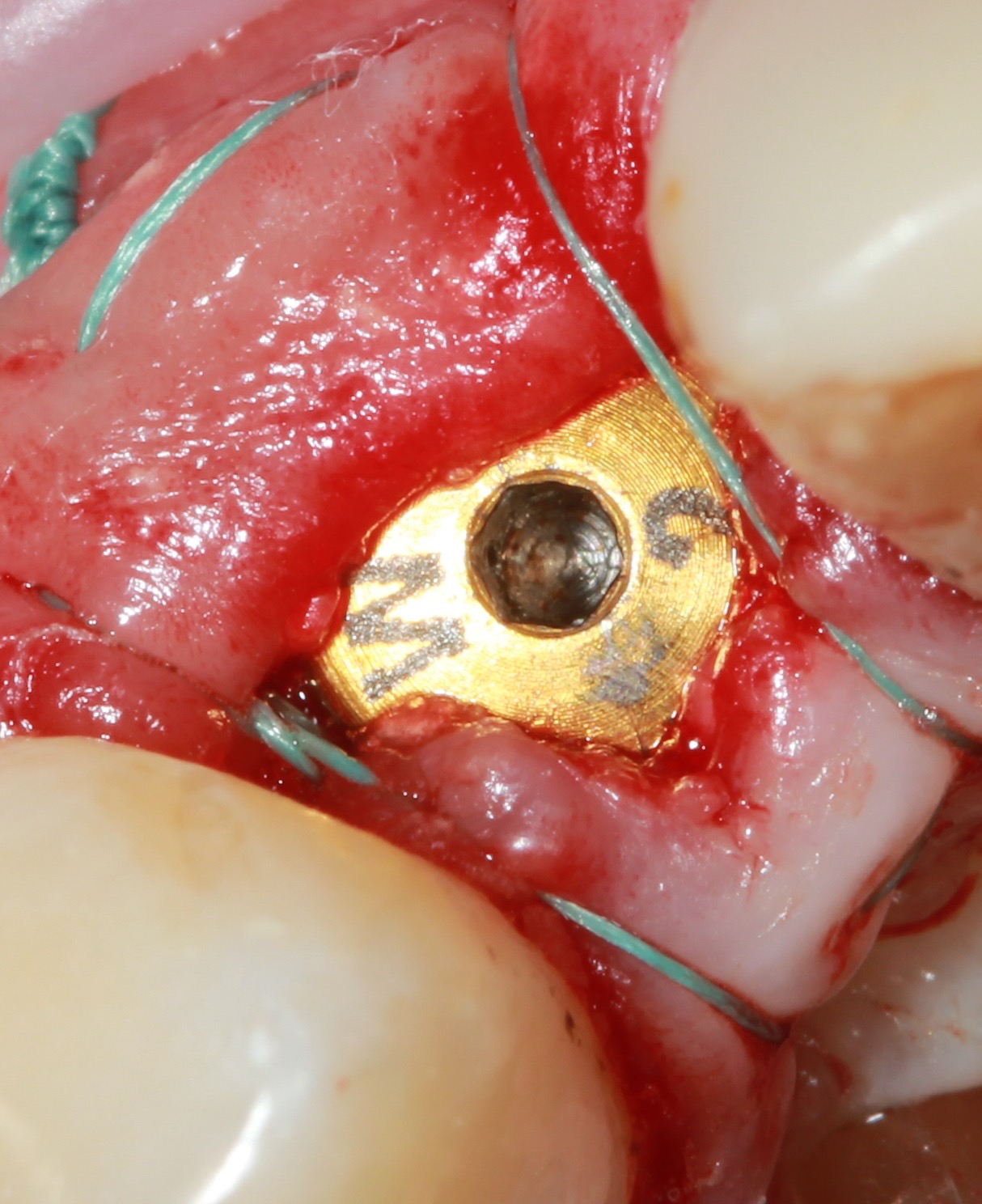
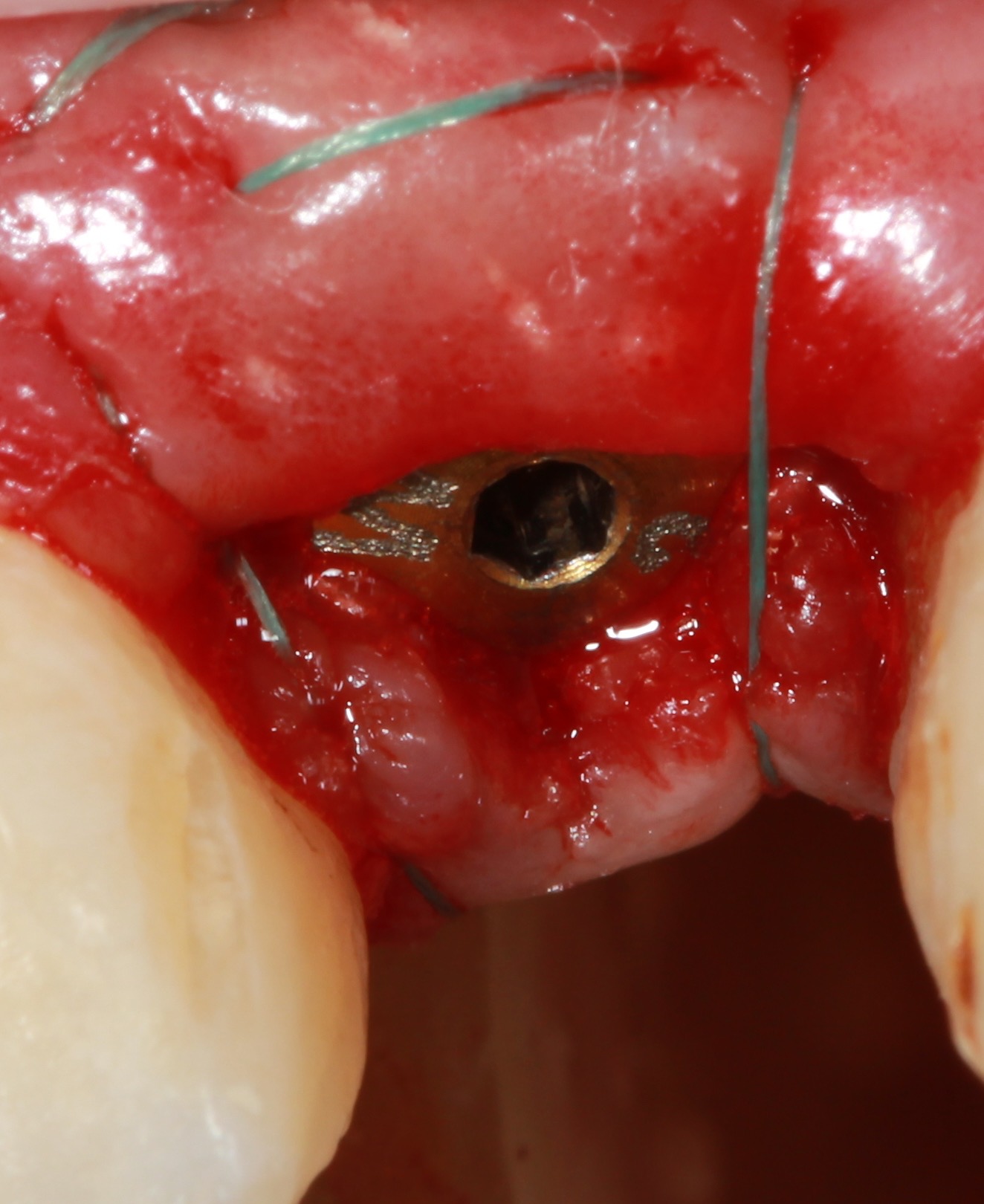
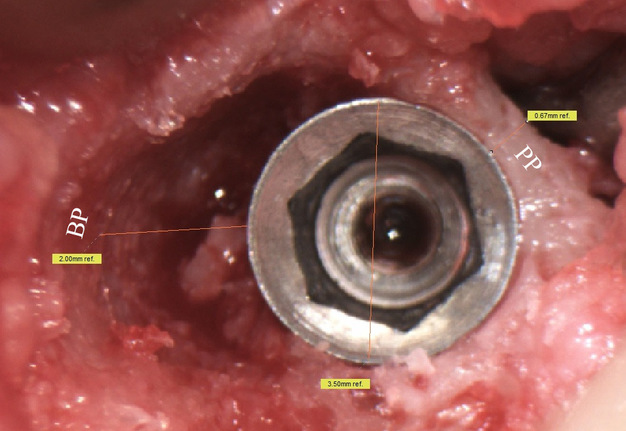
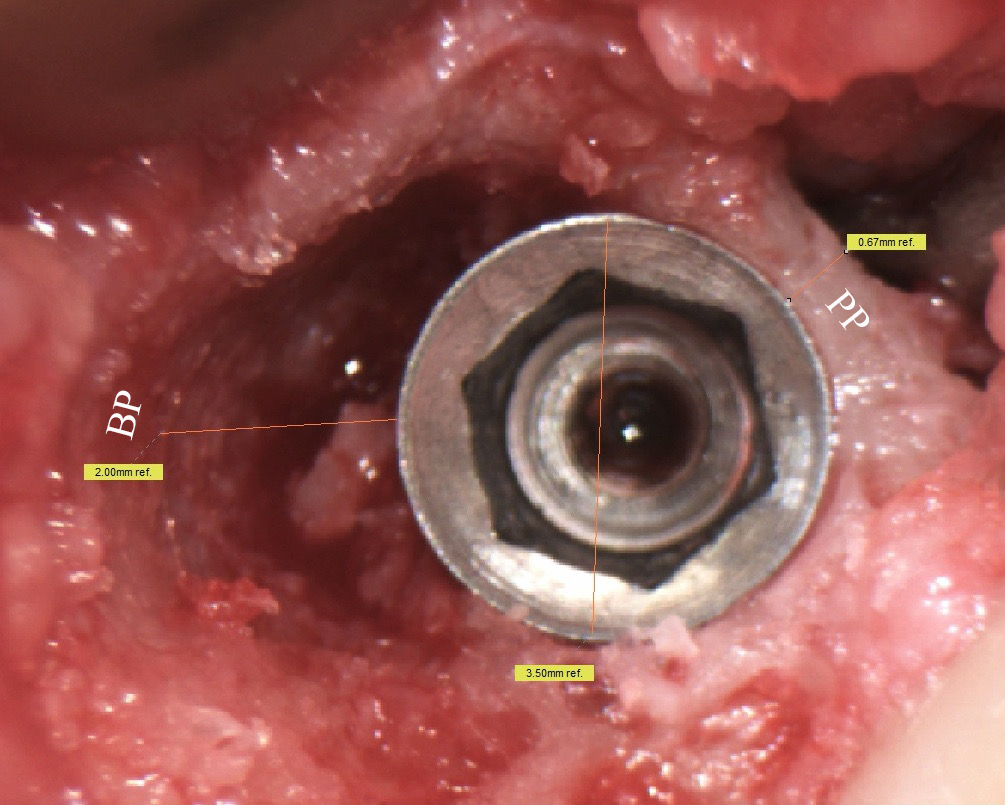
A 32-year-old lady referred to the clinic with complaints for symptoms of chronic periapical lesion of a tooth #12. A surgery was performed under local anesthesia (1.7 ml Ultracain D-S forte, Frankfurt, Aventis Pharma Deutschland GmbH). After atraumatic removal of a tooth #12 a 10 mm implant (U-Impl, Biel, Switzerland) with 3.5 mm platform was placed more palatally and distally related to the extraction socket (Fig 1). It was chosen a 10 mm implant length with a purpose of possible changing for a longer implant in future in case of re-implantation. The 5.5 mm × 2.0 mm healing abutment (W2, U-Impl, Biel, Switzerland) was used. Sutures: 4-0 coated VICRYL (Ethicon, USA). That type of technique (according to recommendation of Neves et al, 2013 [6]) allowed achieving a spontaneous bone healing and osseointegration of implant with a 2.0 mm gap (Fig 2) filled with blood clot. No graft material was used according to the size of horizontal defect recommended by Proceedings of the Third ITI Consensus Conference [7]. A 1.2 year follow-up shows a good aesthetics and no significant recession of soft tissues around the implant.
FIGURE 1A. Buccal plate preservation at anterior maxilla using immediate implant placement with a 2.0 mm gap technique. A – tooth socket (asterisk) after atraumatic extraction of tooth #12. B – view after initial drilling (place of drilling is indicated by circle). C – view after 10 mm implant with 3.5 mm platform placement. 2 mm gap is marked by letter G. D – view after the healing abutment was placed. E – axial view after suturing. F – oblique view after suturing.
FIGURE 1B. Buccal plate preservation at anterior maxilla using immediate implant placement with a 2.0 mm gap technique. A – tooth socket (asterisk) after atraumatic extraction of tooth #12. B – view after initial drilling (place of drilling is indicated by circle). C – view after 10 mm implant with 3.5 mm platform placement. 2 mm gap is marked by letter G. D – view after the healing abutment was placed. E – axial view after suturing. F – oblique view after suturing.
FIGURE 1C. Buccal plate preservation at anterior maxilla using immediate implant placement with a 2.0 mm gap technique. A – tooth socket (asterisk) after atraumatic extraction of tooth #12. B – view after initial drilling (place of drilling is indicated by circle). C – view after 10 mm implant with 3.5 mm platform placement. 2 mm gap is marked by letter G. D – view after the healing abutment was placed. E – axial view after suturing. F – oblique view after suturing.
FIGURE 1D. Buccal plate preservation at anterior maxilla using immediate implant placement with a 2.0 mm gap technique. A – tooth socket (asterisk) after atraumatic extraction of tooth #12. B – view after initial drilling (place of drilling is indicated by circle). C – view after 10 mm implant with 3.5 mm platform placement. 2 mm gap is marked by letter G. D – view after the healing abutment was placed. E – axial view after suturing. F – oblique view after suturing.
FIGURE 1E. Buccal plate preservation at anterior maxilla using immediate implant placement with a 2.0 mm gap technique. A – tooth socket (asterisk) after atraumatic extraction of tooth #12. B – view after initial drilling (place of drilling is indicated by circle). C – view after 10 mm implant with 3.5 mm platform placement. 2 mm gap is marked by letter G. D – view after the healing abutment was placed. E – axial view after suturing. F – oblique view after suturing.
FIGURE 1F. Buccal plate preservation at anterior maxilla using immediate implant placement with a 2.0 mm gap technique. A – tooth socket (asterisk) after atraumatic extraction of tooth #12. B – view after initial drilling (place of drilling is indicated by circle). C – view after 10 mm implant with 3.5 mm platform placement. 2 mm gap is marked by letter G. D – view after the healing abutment was placed. E – axial view after suturing. F – oblique view after suturing.
Discussion
According to Neves et al (2013) and the Proceedings of the Third ITI Consensus Conference about implants in postextraction sites present some of the consensus statements regarding buccal plate preservation and indications for gap filing [6, 7]:
-
External resorption (modeling) of the socket walls occurs during bone healing.
-
There is spontaneous bone healing and osseointegration of implants with a horizontal defect dimension of 2 mm or less.
-
Bone regeneration procedures are recommended when there is a horizontal defect dimension larger than 2 mm and/or nonintact socket walls.
Chen and Buser (2009) accentuated on a recommendation: when the gap is greater than 2 mm, bone gap filling is indicated [8].
Result
Thus, our case represents an extreme limit, a horizontal defect dimension of 2 mm, can be used as a recommended treatment with a purpose for buccal plate preservation upon immediate implantation supporting long-term aesthetics in the anterior maxilla.
Conclusion
That report, a case of 2.0 mm non grafted gap between immediate implant and buccal plate, confirms: 1) good spontaneous bone healing, 2) successful osseointegration, 3) buccal plate preservation.
Conflict of Interest
None.
Role of the Co-authors
Kateryna Y. Nagorniak (concept and design of the paper, material collection, and writing)
Ivan V. Nagorniak (concept and design of the paper, material collection, and editing)
Ethical Approval
None.
Term of Consent
Written patient consent was obtained from parents to publish the clinical photographs.
Fundings
No funding was received for this study.
Acknowledgments
None.
References (12)
-
Mehta H, Shah S. Management of buccal gap and resorption of buccal plate in immediate implant placement: a clinical case report. J Int Oral Health 2015;7(Suppl 1):72–5.
-
Botticelli D, Berglundh T, Buser D, Lindhe J. The jumping distance revisited: an experimental study in the dog. Clin Oral Implants Res 2003;14(1):35–42.
-
Januário AL, Duarte WR, Barriviera M, Mesti JC, Araújo MG, Lindhe J. Dimension of the facial bone wall in the anterior maxilla: a cone-beam computed tomography study. Clin Oral Implants Res 2011;22(10):1168–71.
-
Katranji A, Misch K, Wang HL. Cortical bone thickness in dentate and edentulous human cadavers. J Periodontol 2007;78(5):874–8.
-
Chen ST, Darby IB, Reynolds EC. A prospective clinical study of non-submerged immediate implants: Clinical outcomes and esthetic results. Clin Oral Implants Res. 2007;18(5):552–62.
-
Neves M, Correia A, Alves CC. A novel approach to preserve the buccal wall in immediate implant cases: a clinical report. J Oral Implantol 2013;39(2):198–205. Crossref
-
Chen S, Buser D. Implant placement in post-extraction sites. In: Buser D, Wismeijer D, Belser D, eds. ITI Treatment Guide. Vol 3. Berlin: Quintessence; 2008.
-
Chen ST, Buser D. Clinical and esthetic outcomes of implants placed in postextraction sites. Int J Oral Maxillofac Implants 2009;24(suppl):186–217.
-
Tavarez RR, Dos Reis WL, Rocha AT, Firoozmand LM, Bandéca MC, Tonetto MR, Malheiros AS. Atraumatic extraction and immediate implant installation: the importance of maintaining the contour gingival tissues. J Int Oral Health 2013;5(6):113–8.
-
Caiazzo A, Brugnami F, Mehra P. Buccal plate preservation with immediate post-extraction implant placement and provisionalization: preliminary results of a new technique. Int J Oral Maxillofac Surg 2013;42(5):666–70. Crossref
-
Groenendijk E, Staas TA, Graauwmans FEJ, Bronkhorst E, Verhamme L, Maal T, Meijer GJ. Immediate implant placement: the fate of the buccal crest. A retrospective cone beam computed tomography study. Int J Oral Maxillofac Surg 2017;46(12):1600–6. Crossref
-
Greenstein G, Cavallaro J. Managing the buccal gap and plate of bone: immediate dental implant placement. Dent Today 2013;32(3):70.