The “Beveled One-and-a-Half-Barrel” Fibula Transplant with Virtual Surgical Planning and CT-Guided Implant Surgery for Prosthetic Rehabilitation in Posterior Mandible Defects: A Pictorial Essay
March 12, 2022
https://doi.org/10.23999/j.dtomp.2022.3.3
J Diagn Treat Oral Maxillofac Pathol 2022;6:39–59.
Under a Creative Commons license
HOW TO CITE THIS ARTICLE
Massarelli O, Meloni SM. The “beveled one-and-a-half-barrel” fibula transplant with virtual surgical planning and CT-guided implant surgery for prosthetic rehabilitation in posterior mandible defects: a pictorial essay. J Diagn Treat Oral Maxillofac Pathol 2022;6(3):39–59.
NATIONAL REPOSITORY OF ACADEMIC TEXTS
https://nrat.ukrintei.ua/en/searchdoc/2022U000179/
SUMMARY
In this study, we present a new case of segmental oro-mandibular reconstruction with fibula transplant, first described as “beveled one-and-a-half-barrel” shape, highlighting tips and tricks for not jeopardizing its vascularity and our technical considerations for adequate dental rehabilitation. A report of all reconstructive stages and secondary implant-rehabilitation phases, outlining the reliability of this new technique together with a comparative analysis of advantages and disadvantages of different reconstructive techniques for alveolar bone reconstruction was made. This technique was applied in our hospital for a 49-year-old Caucasian woman with an aggressive recurrent ameloblastoma of the left mandible. Post-operative computed tomography with clinical intra- and extraoral photography are presented. We believe that this pictorial essay presented in our paper could be useful as a goal-oriented step-by-step highly detailed surgical guide to achieve a reliable and good shaped bone hardware for further dental rehabilitation in case of segmental posterolateral mandibular reconstruction.
INTRODUCTION
Four years have passed from the first report of fibula free flap (FFF) for mandibular reconstruction described by Hidalgo1 in 1989, when in 1993 Sadove et al2 reported a simultaneous maxillary and mandibular reconstruction with one osteocutaneous fibula free flap, removing the median portion and utilizing the two distal ends. This was the first evidence in head and neck reconstruction field of the fibular periosteal feeding ability, that represents the fundamental vascular principle on which is based the “double barrel fibular graft” harvesting popularized in 1995 by Horiuchi et al3 among the head and neck surgeons community.
Later in 2004 Lee et al4 designed a non-vascularized residual fibula graft for 2-strut type mandibular reconstruction as double barrel hybrid fashion FFF.
A secondary vertical distraction osteogenesis of a fibular graft followed by implant therapy has been fundamentally analyzed by Siciliano et al5 in 1998 and then followed by others during next 21 years6–8. Many technical efforts were made to overcome the main limitation of “single barrel” and “double barrel” FFF to allow prosthetic rehabilitation with an implant-based denture by functional and aesthetic points of view, but all were unsuccessful till 2013. The problem of height discrepancy between native mandible and fibula flap was brilliantly solved by Ulkur et al9, who first described the “one-and-a-half-barrel FFF” technique in a case of right mandibular body reconstruction following a giant cell reparative granuloma resection.
The defect extended between the ascending branch and the distal part of the canine tooth and measured almost 8 cm in length.9 A 17-cm long free fibular flap was designed and harvested.9 After removing a small piece of fibular bone to fold the transplant, the authors split longitudinally the distal half of the free fibula flap and removed the bone segment away from the perforating vessels.9 Then the remaining 2 fibula segments were doubled and placed parallel to each other to proper fill the defect and a dental rehabilitation by secondary dental implantation was performed 1.5 year later using a surgical guide based on a cone beam dental volumetric tomography (CBDVT).9
Even though, the “one-and-a-half barrel” technique9 may be a good solution to improve volume insufficiency of the classical single-strut technique and volume excess of the double-barrel technique for almost all mandibular segments, we believe that for the premolar-molar region, as in cases of defects of the retromolar trigon, it is less effective.
The purpose of this study is to present a new case of oro-mandibular reconstruction with this type of flap modeling in order to confirm its technical feasibility, highlighting our technical innovations compared to the originally described by Ulkur et al.9
The computer-aided three-dimensional virtual planning together with customized cutting guides manufacturing, prompted us to raising, for the first time in literature, the one-and-a-half-barrel FFF in a “bevel shape” in a case of segmental mandibular reconstruction. This technical improvement has allowed us a tremendous mandibular reconstructive precision, especially in the premolar-molar region where an adequate prosthetic space is necessary for a very precise and long-lasting implant-supported rehabilitation. A CT-guided implant surgery helped us finalize the case in a more functional and precise way. A report of all reconstructive stages and secondary implant-rehabilitation phases, outlining the reliability of this new technique together with a comparative analysis of advantages and disadvantages of different reconstructive techniques for alveolar bone reconstruction was made.
CASE
A 49-year-old Caucasian woman, a professional teacher, with the suspicion of recurrent aggressive ameloblastoma of the left mandible was referred to the Maxillofacial Surgery Unit, University Hospital of Sassari (Sassari, Italy) in May 2016, after having performed a conservative treatment (tumor enucleation) in another center two years earlier. She denied experiencing any bleeding, but complained some pain and dysesthesia in the mandibular nerve area.
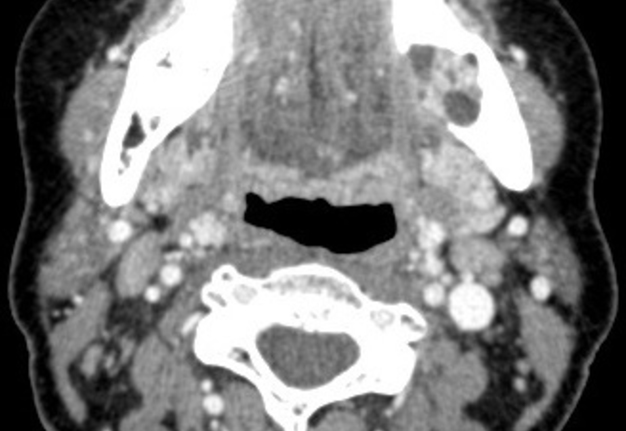
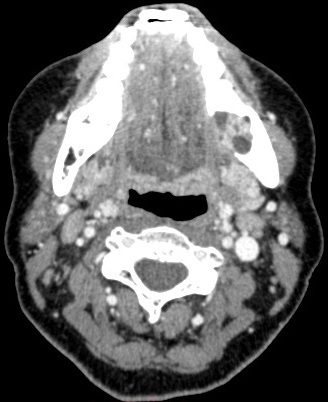
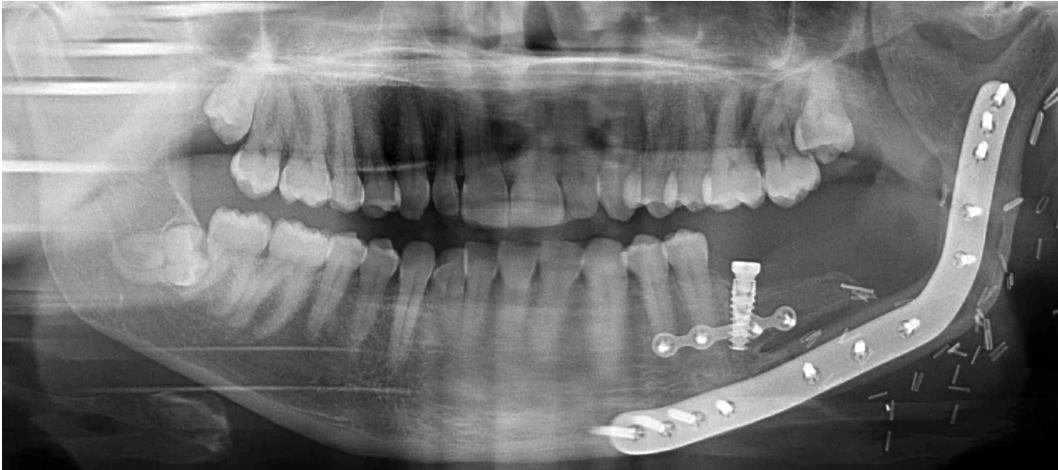
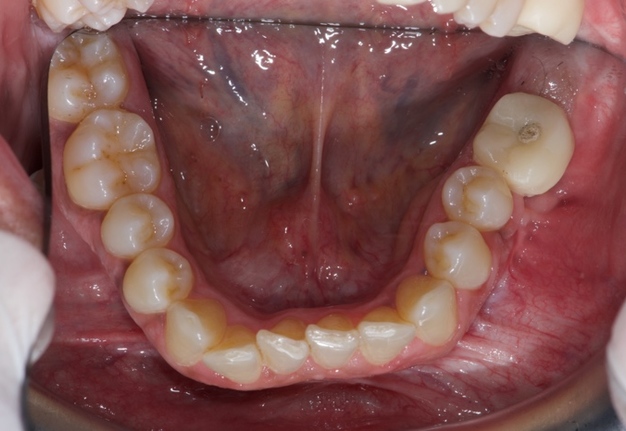
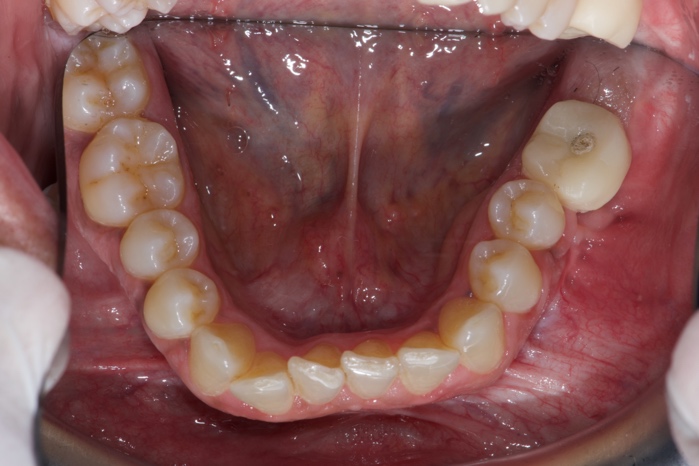
On physical examination, facial asymmetry due to swelling on the left side of the face was moderately noticed (Fig 1). The intraoral examination revealed some trigon-shape scarring of the mucosa, the absence of 3.7, extracted in previous intervention, and an ill-defined solitary swelling in the left lower posterior buccal vestibule. This extended anterioposteriorly from 3.6 to the retromolar region and mediolaterally to the buccal sulcus. The overlying mucosa was stretched and slightly whitish, but similar to adjacent mucosal color (Fig 2). On palpation, the swelling was found to be firm, bony hard in consistency, non-tender, non-fluctuant, irreducible, non-compressible and non-pulsatile. The teeth in the vicinity were non-tender to percussion, but slight mobility of 3.6 was present. On electric pulp vitality testing, all teeth in the affected area were vital except 3.6. No lymphadenopathy or fistulas were present. An incisional biopsy was made and the specimen was subjected to histopathological examination. The lesion was found to be a desmoplastic (ie, follicular) ameloblastoma. The CT scans of the mandible (Fig 3A-B) showed a large well-defined expansive radiolucent lesion with a multilocular aspect centered in the left retromolar trigon region. This was responsible for the mandibular body expansion from the mesial surface of the first left lower molar to the mesial surface of the ramus, approximately measuring 5 × 4 cm in size.
FIGURE 2. Intraoral examination showed trigon-shape scarring of the mucosa, the absence of 3.7, extracted in previous intervention and an ill-defined solitary swelling in the left lower posterior buccal vestibule. This extended anterioposteriorly from 3.6 to the retromolar region and mediolaterally to the buccal sulcus. The overlying mucosa was stretched and slightly whitish, but similar to adjacent mucosal color.
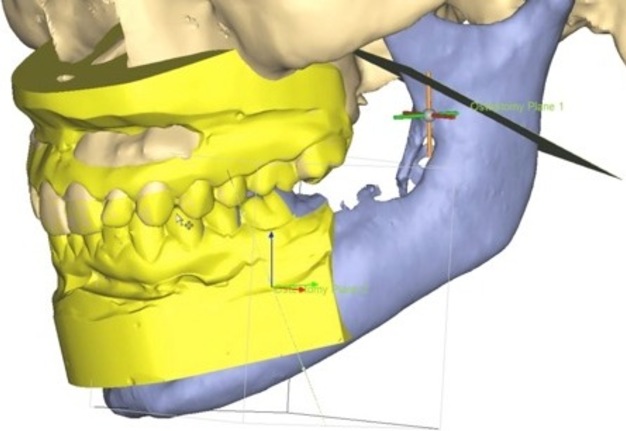
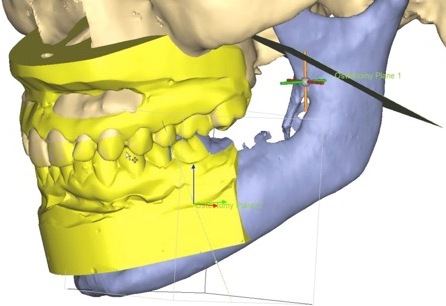
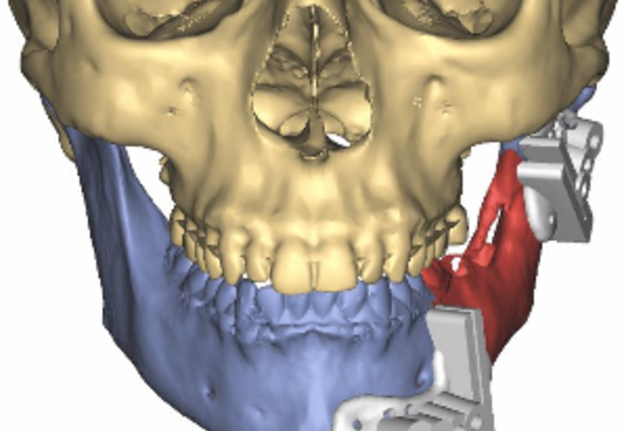
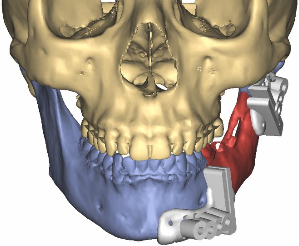
The patient underwent left angular and body mandibular resection with simultaneously reconstruction by mean a left fibula free flap that was planned and shaped thanks to the Synthes ProPlan software (Synthes GmbH, Oberdorf, Switzerland), while the implant-prosthetic rehabilitation was planned according to the NobelClinician® protocol.
After informed consent had been obtained, plaster models, dental impressions (Fig 4A-B), initial photographs, and measurements with a facebow for aesthetic-functional evaluation, were taken.
The acquisition of high resolution CT data of the maxillofacial skeleton, the plaster models of the jaw and of the donor site have been performed. The data obtained were converted into three-dimensional models thanks to the ProPlan software.
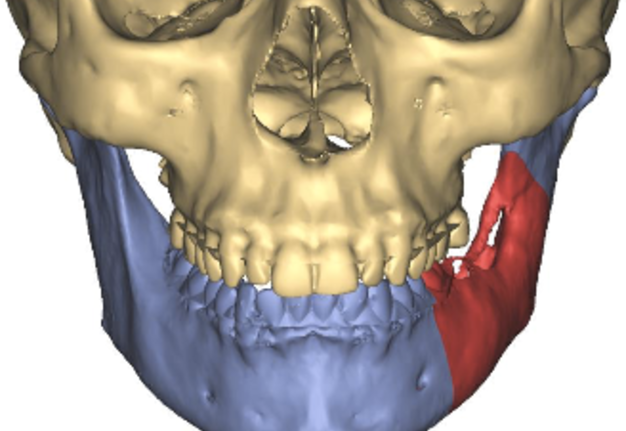
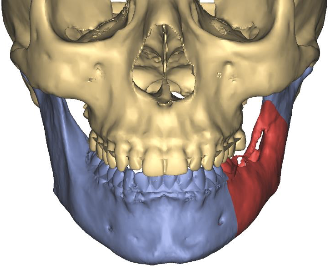
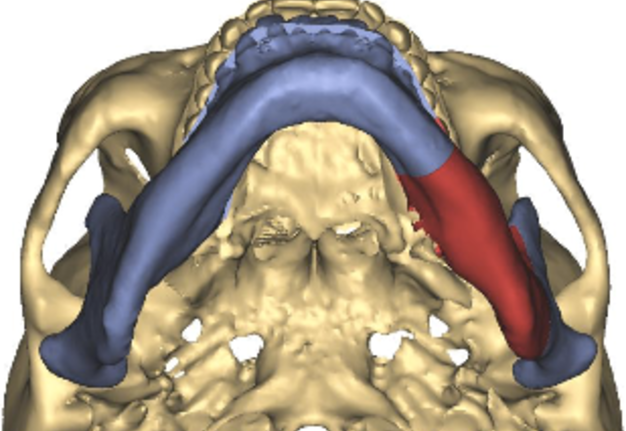
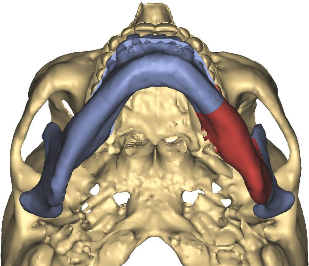
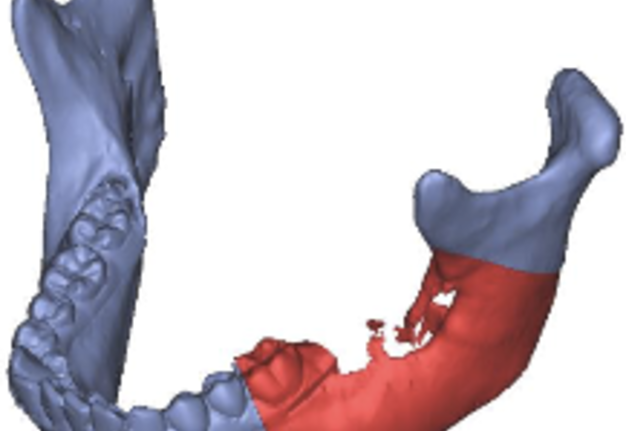
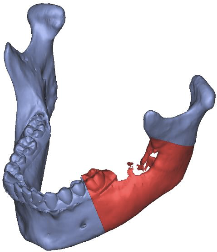
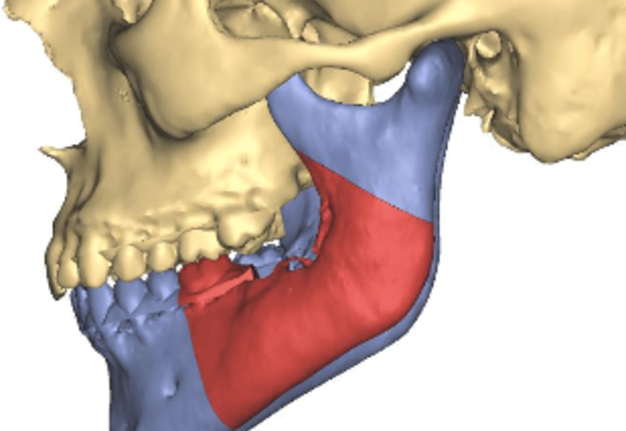
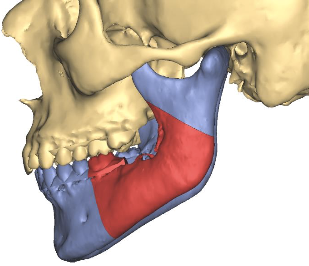
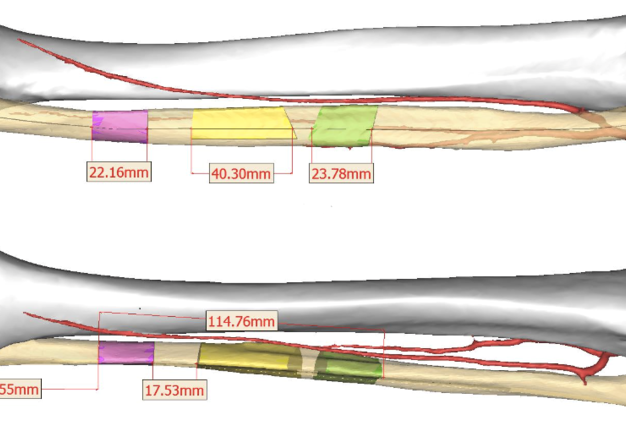
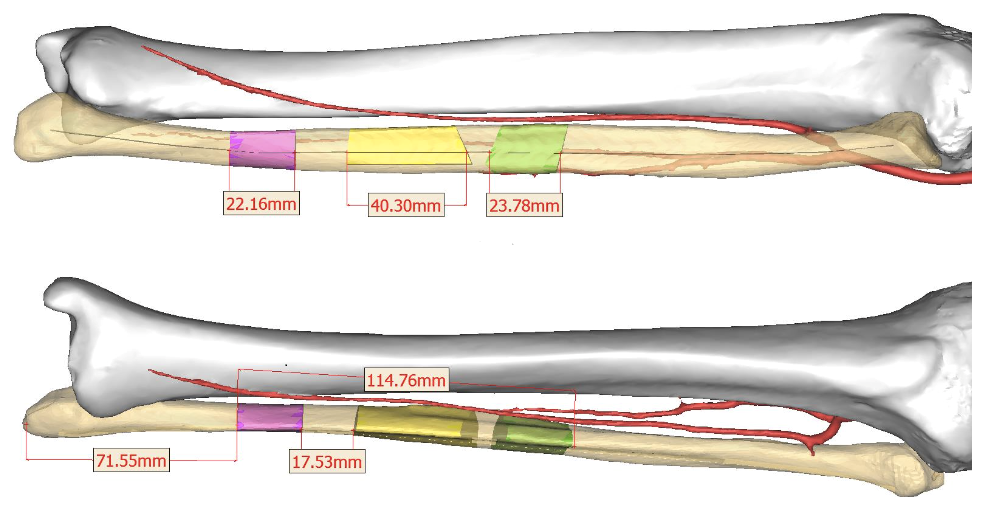
The safety margins for the lesion removal (Fig 5A-D), the number and the orientation of the fibula osteotomies (Fig 6A-B) are established through a videoconference for surgery planning.
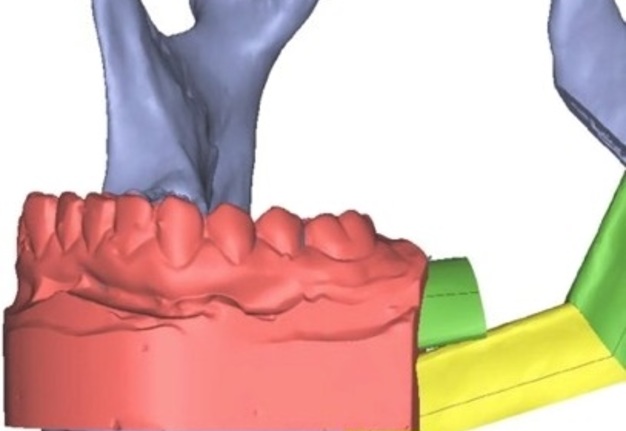
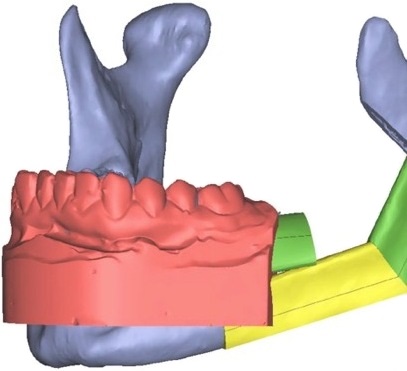
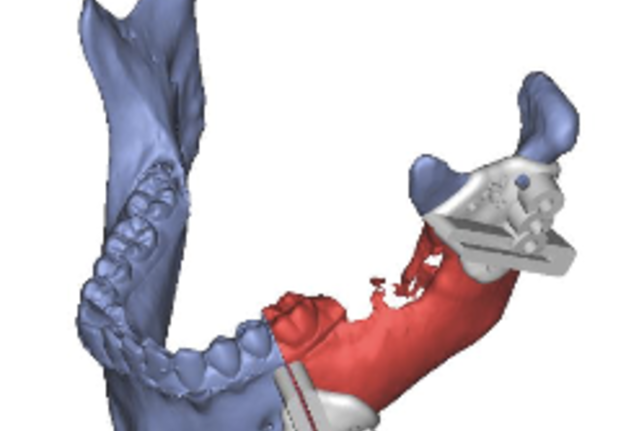
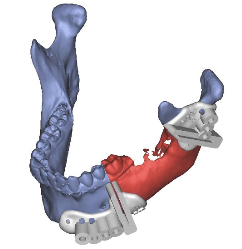
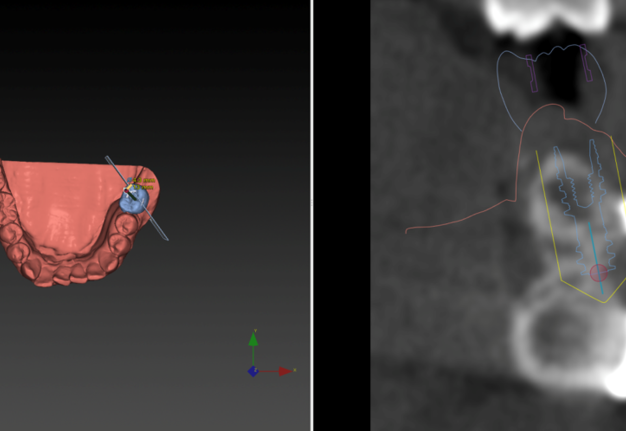
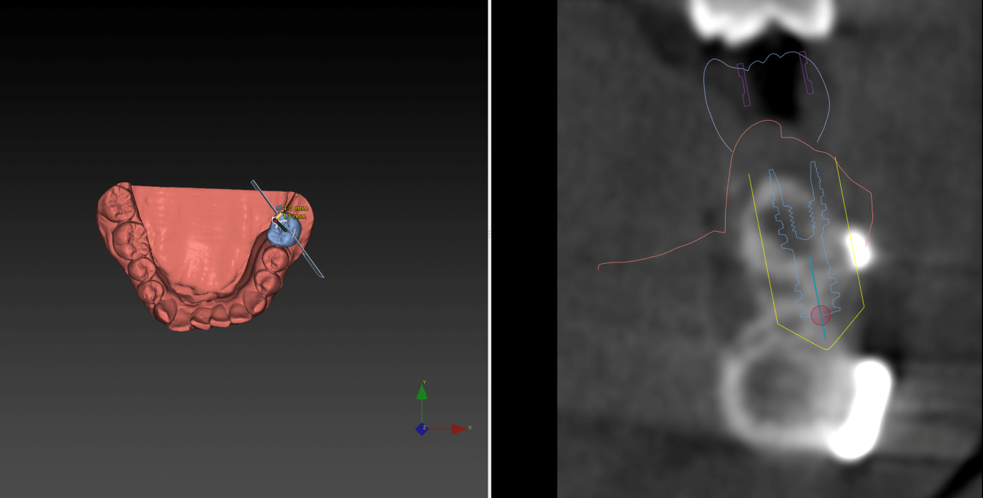
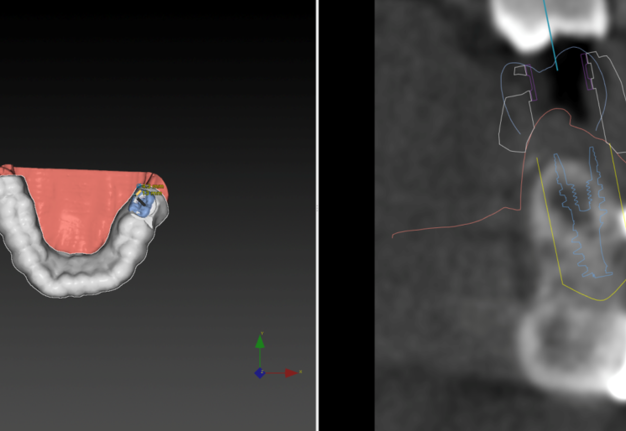
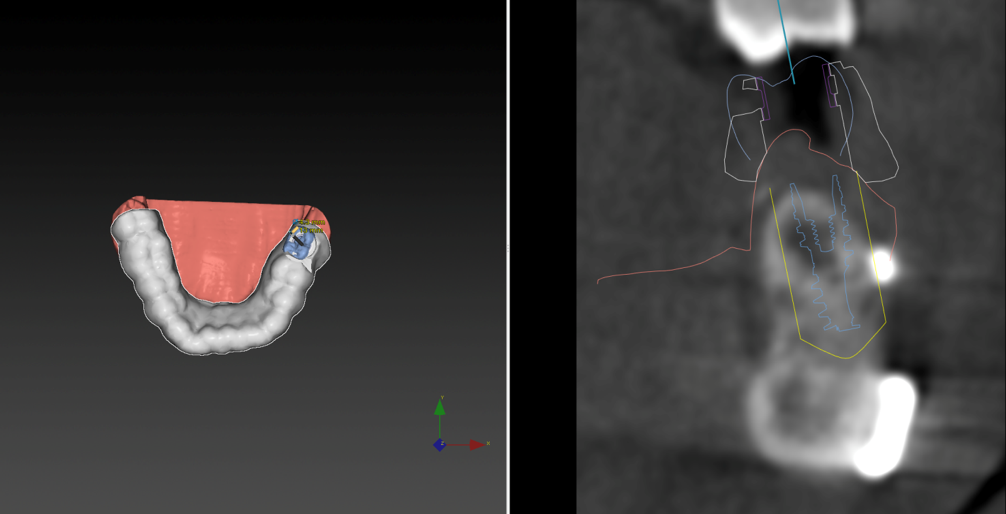
For greater precision in mandibular reconstruction the jaws’ plaster models scans were overlay on the preoperative CT mandibular data and then on the mandibular osteotomized planned model in order to preview the future proper position of the dental element in the reconstructed jaw (Fig 7A-C). This suggested us to split the doubled segment obliquely in order to obtain the exact mandibular bone height and consequently the correct prosthetic space.
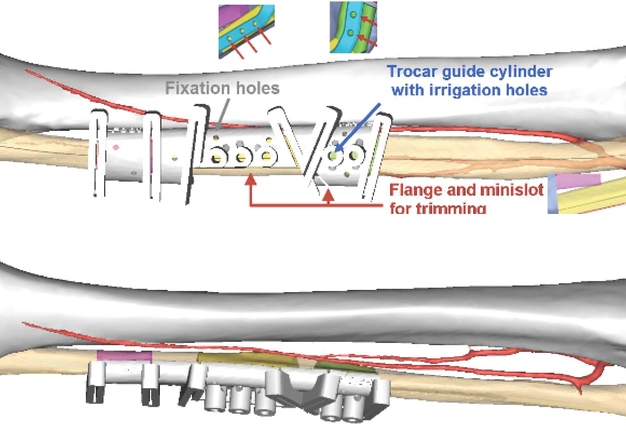
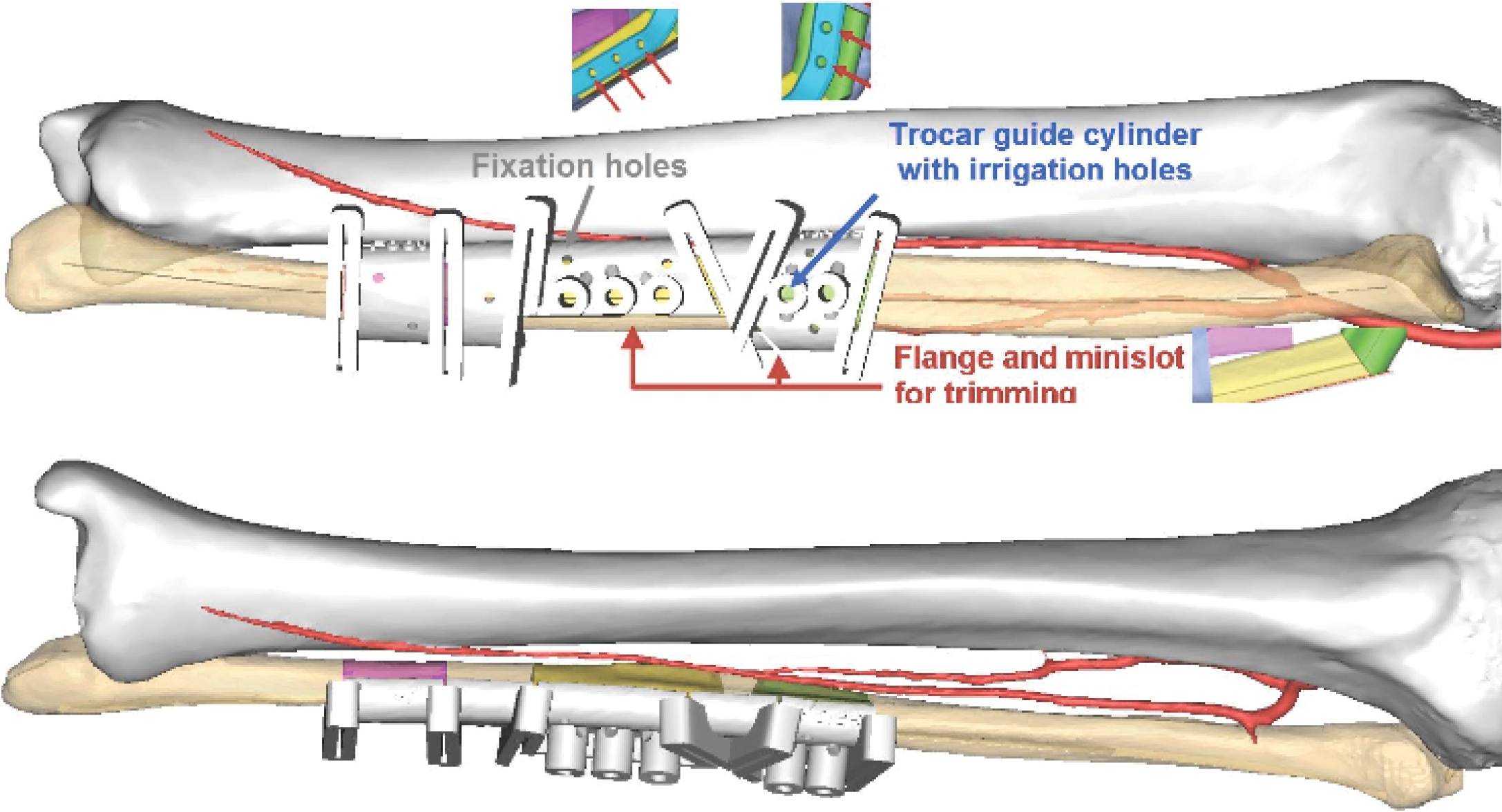
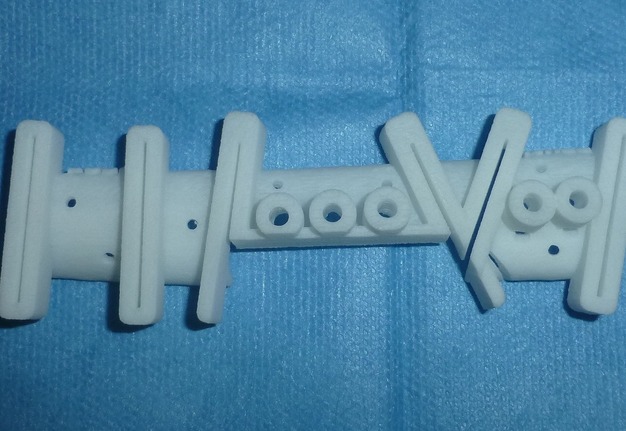
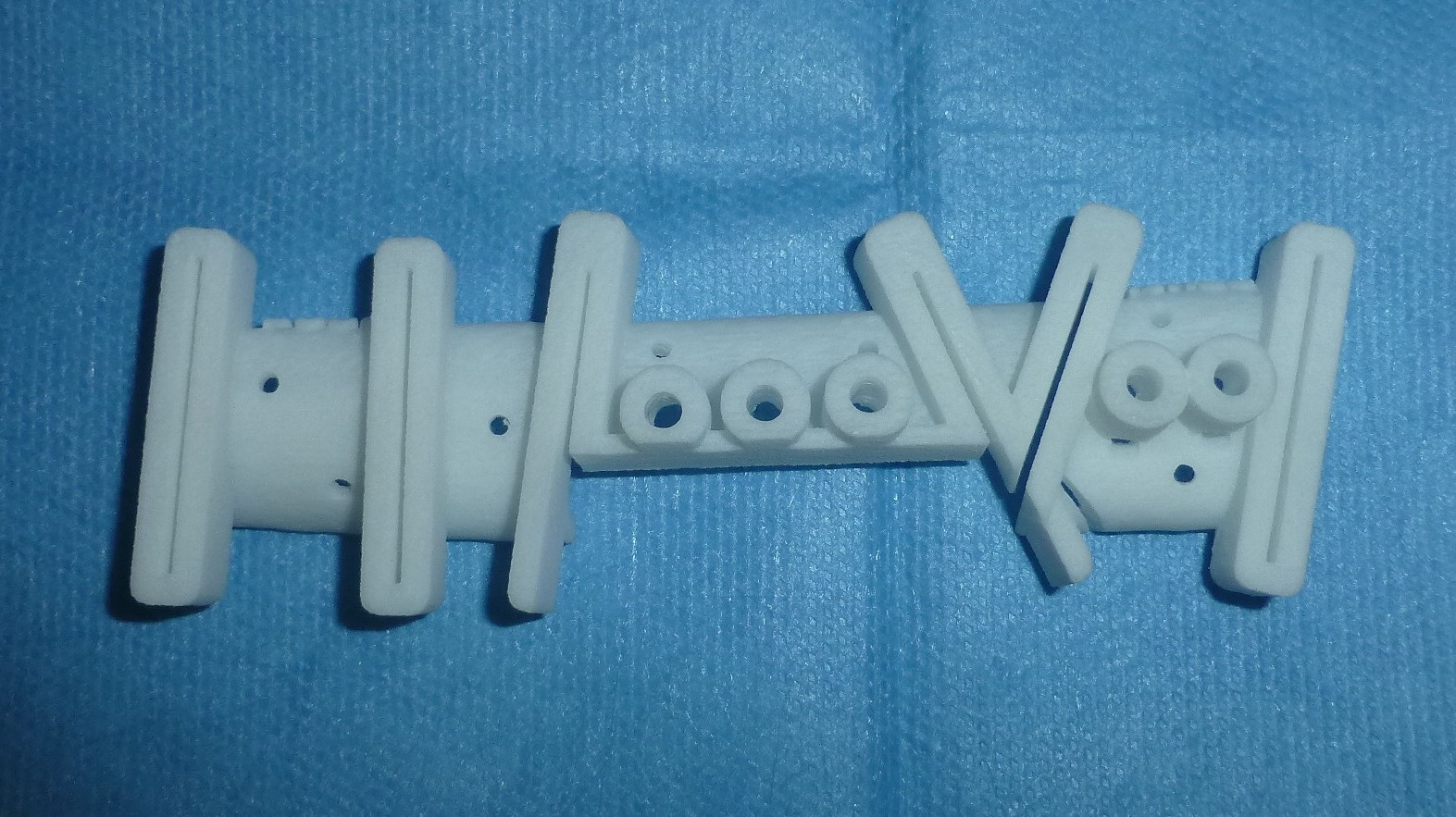
A patient specific mandible cutting guide (Fig 8A-B) as well a patient specific fibula harvesting guide with a minislot for oblique bone splitting (Fig 9A-B) have been manufactured. The latter allowed trimming safely the fibular shaft longitudinally, having considered exactly where was the vascular pedicle and avoiding sectioning it.
FIGURE 9A-B. Planning of a patient specific fibula harvesting guide with a flange and minislot for oblique bone trimming. Image A represents lateral view and image B – anterior view. Guide design:
-
Slot width: 1 mm.
-
Trocar guide cylinders: For use with Synthes trocar drill guide 03.503.045 (indicated in blue).
-
Fixation hole diameter: 2.2 mm (suitable for 1.5 mm drill, 2.0 mm screws) (indicated in gray).
-
Fixation holes are intended for temporary fixation of the guide.
Finally, a stereolithographic model and a patient-specific plate were made and sent to us helping to carry out the reconstructive plan in the operative theatre (Fig 10A-B).
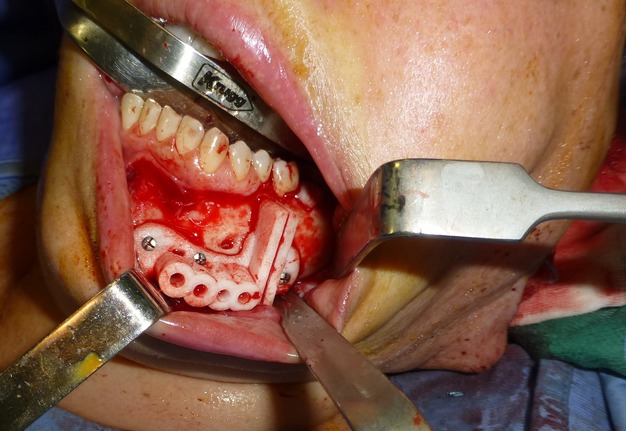
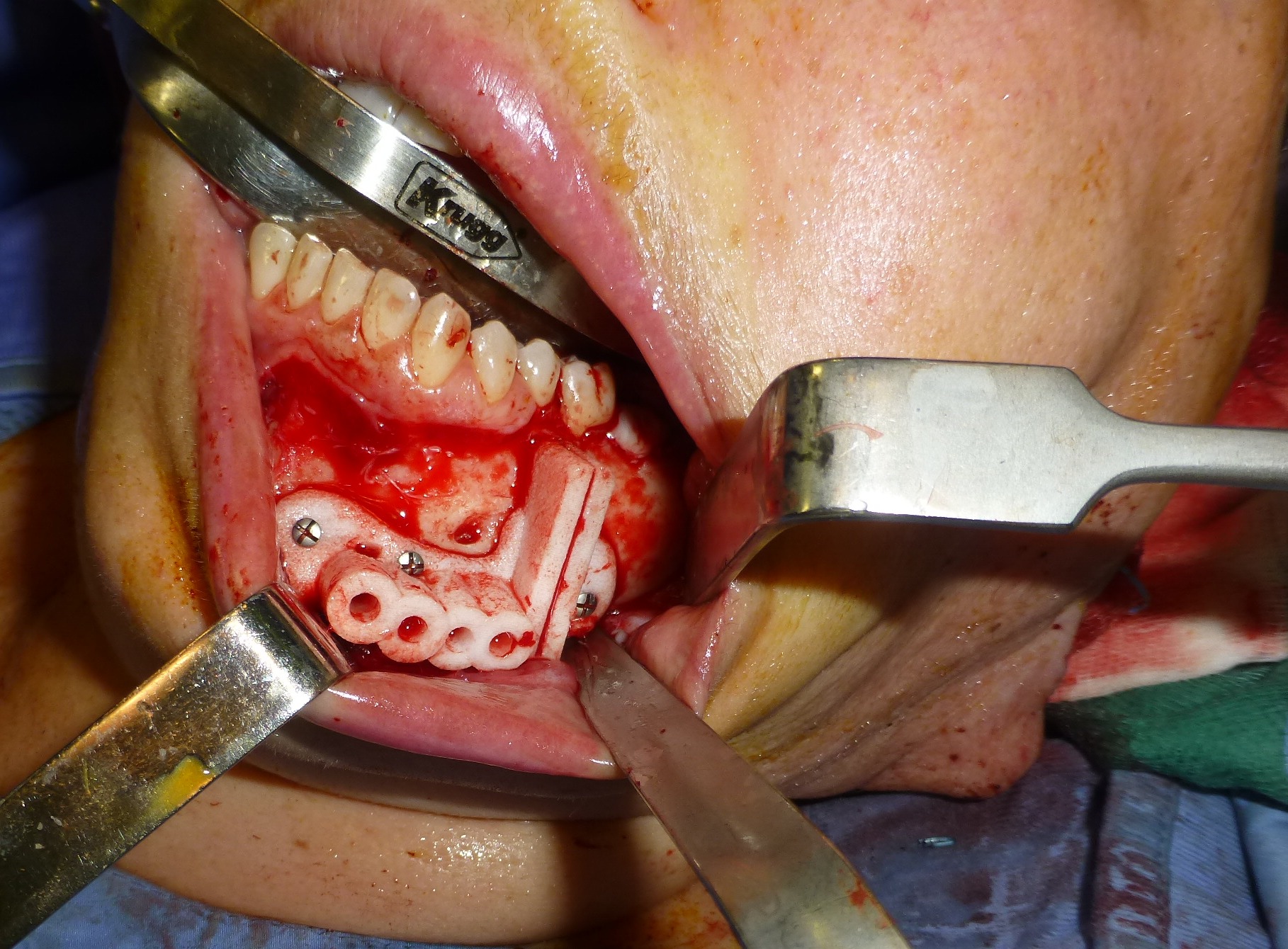
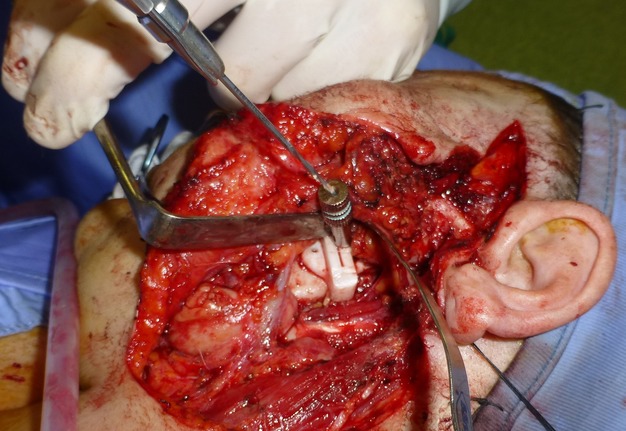
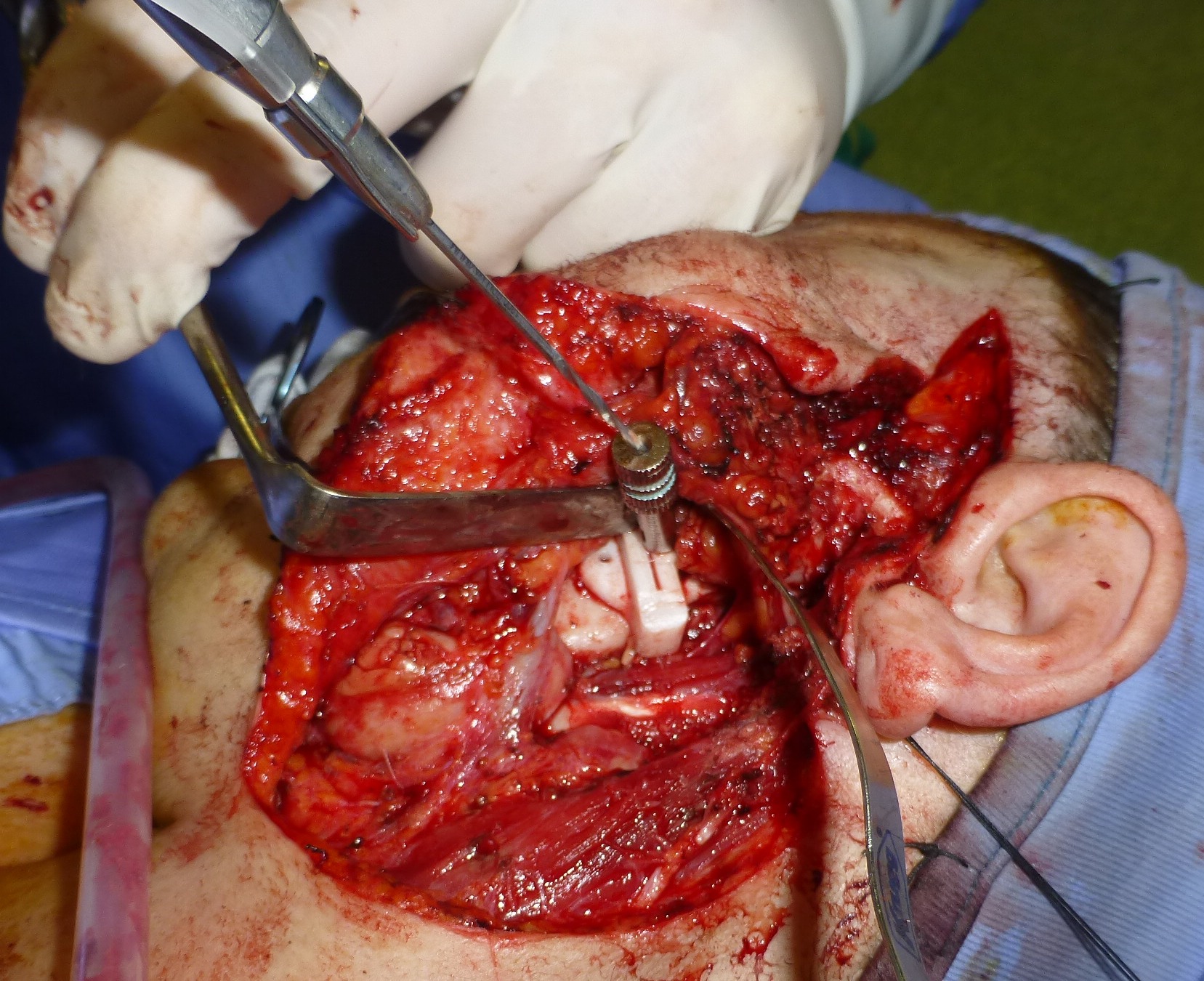
The cutting guides have fitted very well to the mandible. Resection was performed using a combined intraoral and external (preauricular) approach (Fig 11A-B) which allowed a safe resection.
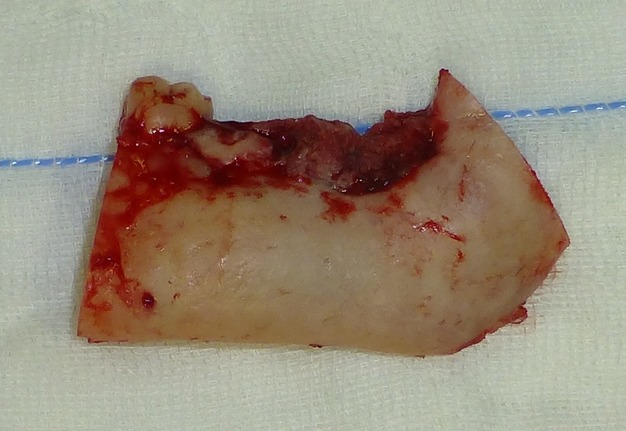
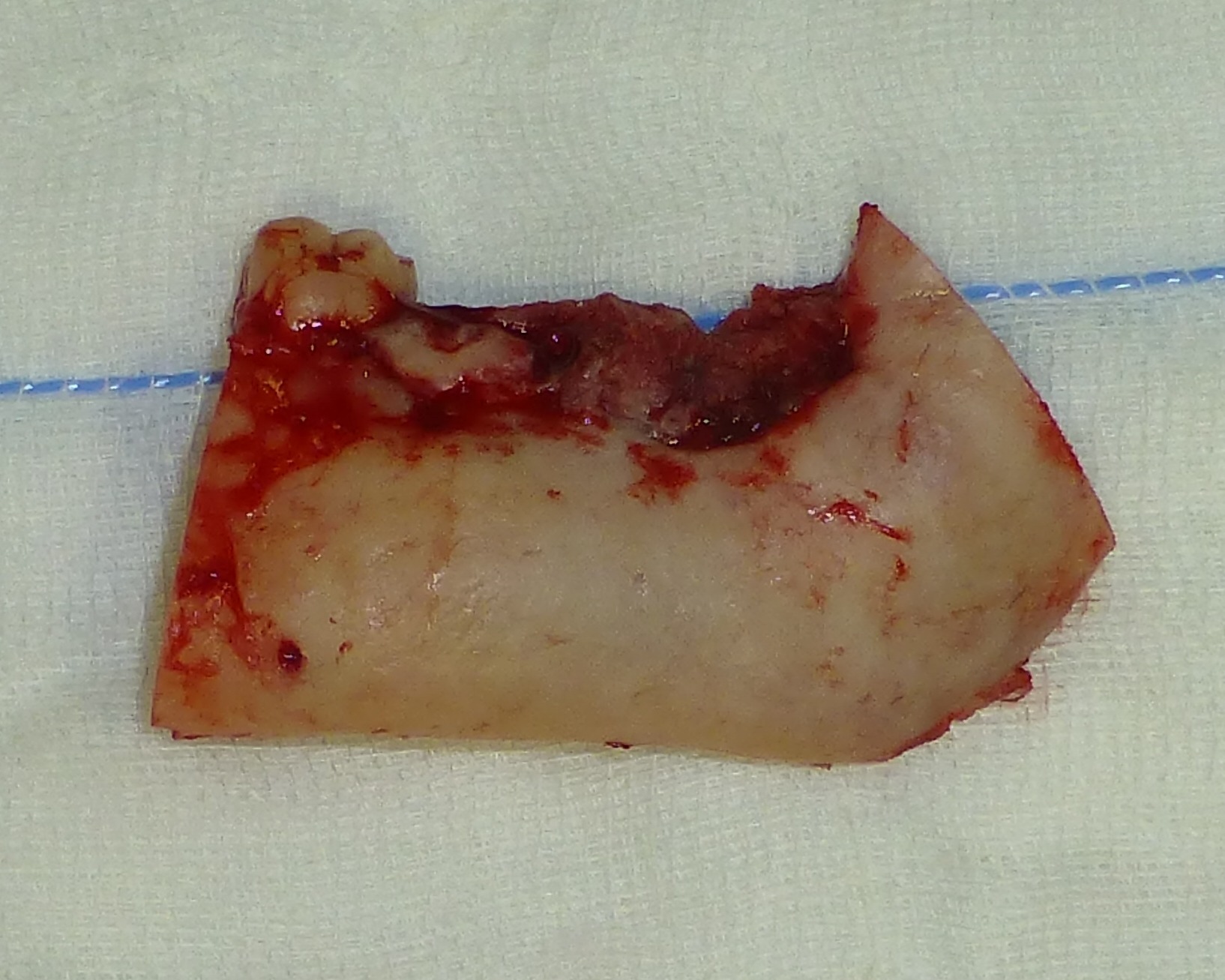
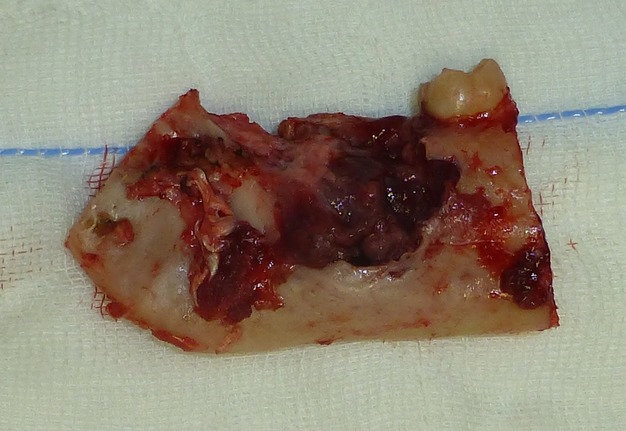
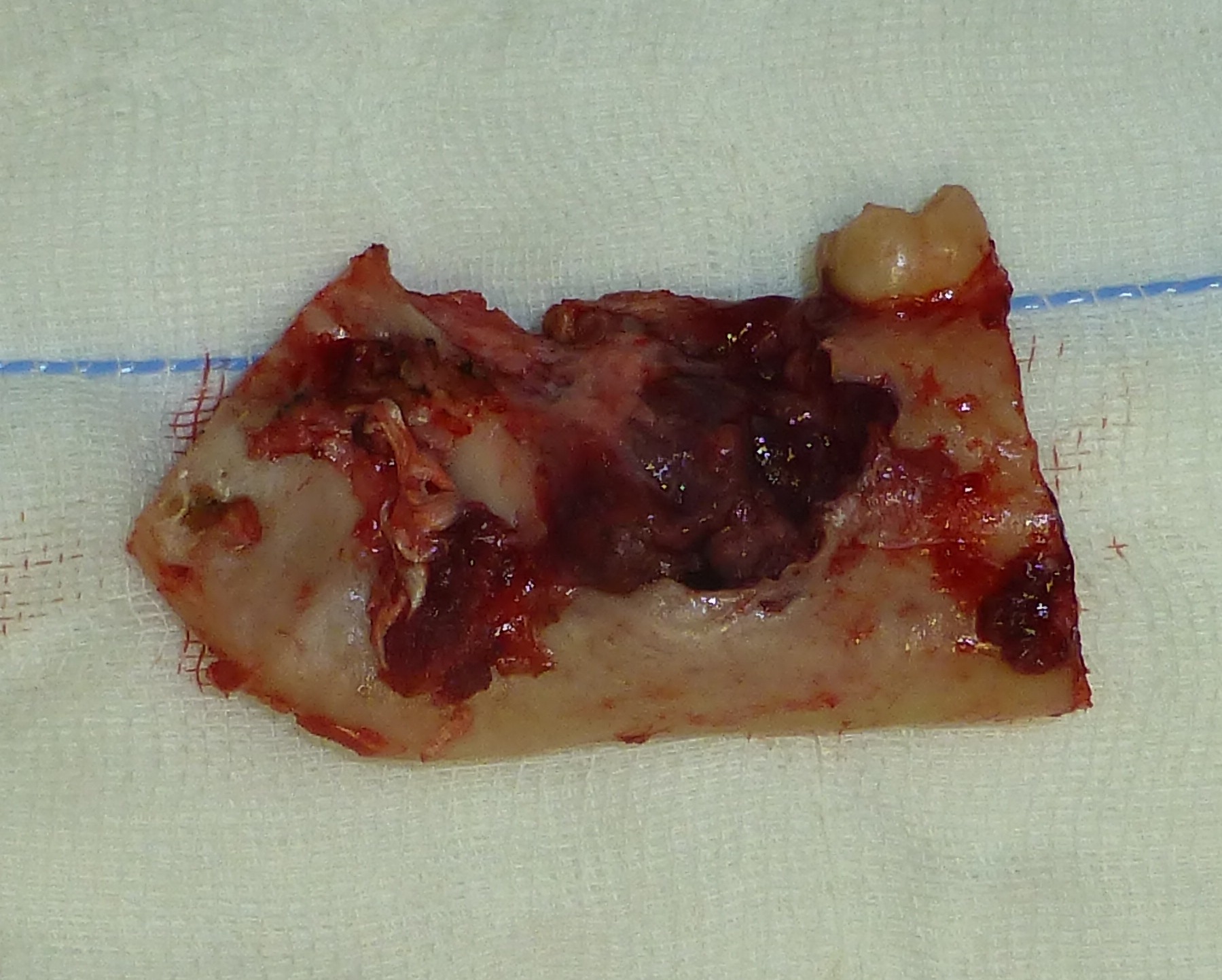
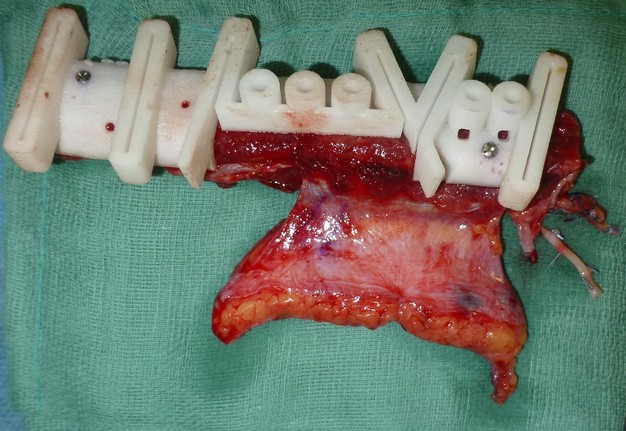
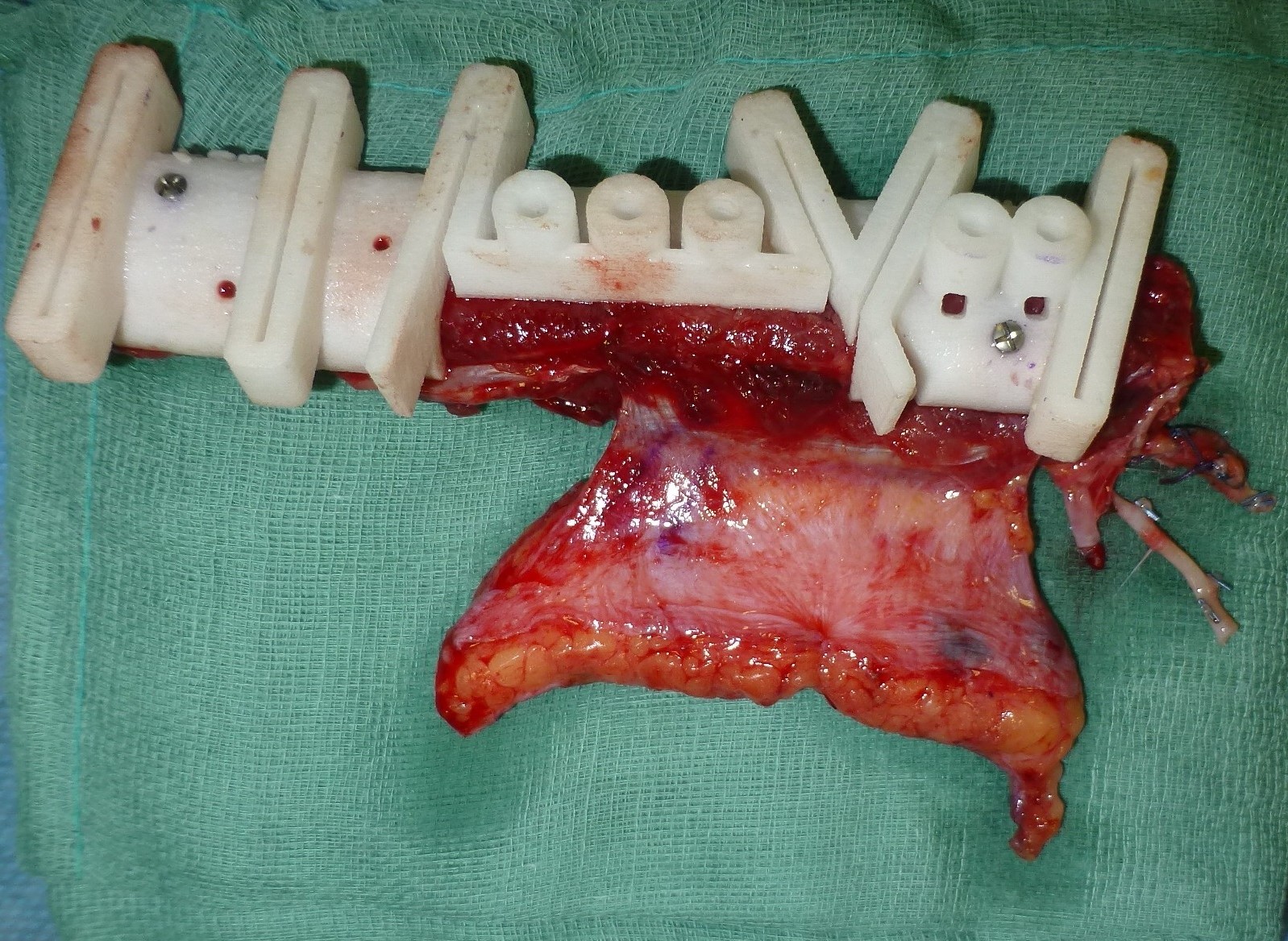
The surgical specimen consisting of a jaw segment with the lesion and associated tooth was found to have tumor-free margins (Fig 12A-B). The osteo-fasciocutaneous beveled one-and-a-half FFF transplant was harvested thanks to the planned fibula guide (Fig 13). The transplant survived completely (Fig 14). The post-operative period was uneventful and the intraoral healing was excellent (Fig 15A-B).
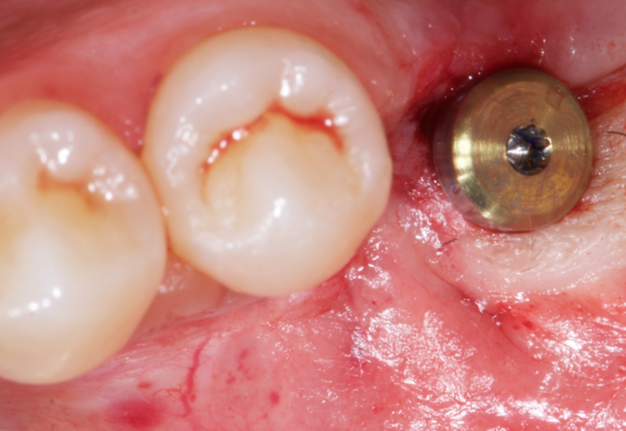
The patient underwent computer-assisted guided implant surgery following the NobelClinician® implant protocol, 14 months after the reconstructive surgery.
The study dental casts were performed mounting them in a mean value articulator, and a diagnostic wax model was made.
A provisional denture was made and the same was filled with radiopaque markers (gutta-percha) as reference points, and used as a radiographic guide for the subsequent installation of the implant. A silicone interocclusal record was made as a radiographic index.
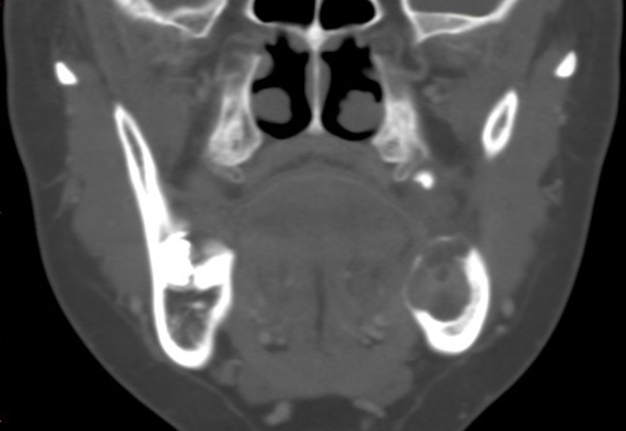
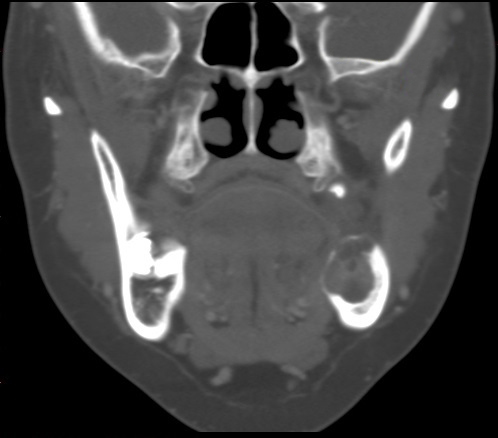
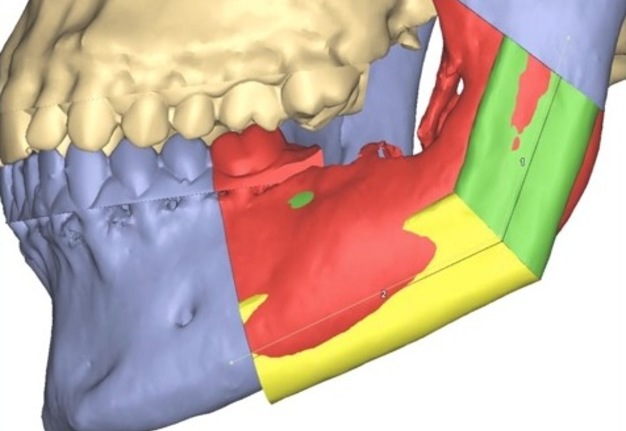
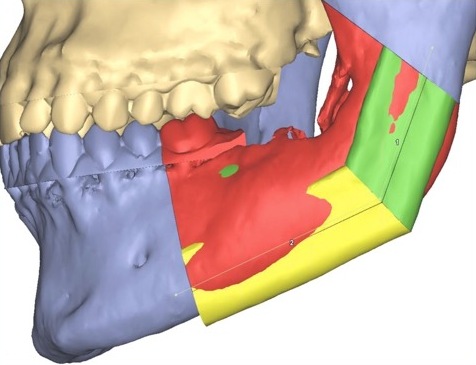
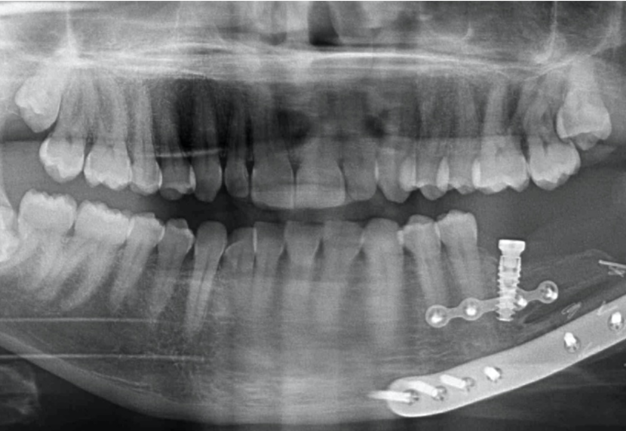
In accordance with the NobelGuide® protocol for the acquisition of data, CT (Cone Beam CT, KaVo Dental GmbH, Biberach, Germany) was taken twice: the first time with the patient wearing the denture (radiological guide) and the radiological index, and the second – with the denture alone. The CT data were transferred to the NobelGuide Procera® software for three-dimensional diagnostic and virtual implant planning. The CT virtual implant planning allowed the insertion of implants while avoiding screws and the plate in the fibular flap (Fig 16A-D). The software planning data were sent to Nobel Biocare (Goteborg, Sweden), where a surgical template was made with the guide implant in the position planned virtually. Then a metal and acrylic resin provisional prosthesis was manufactured (Fig 17A-B).
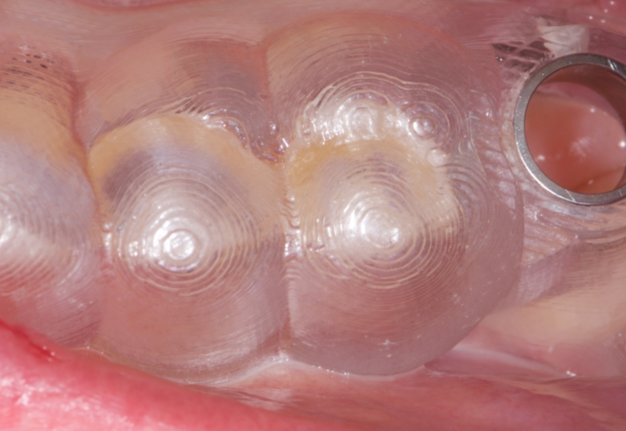
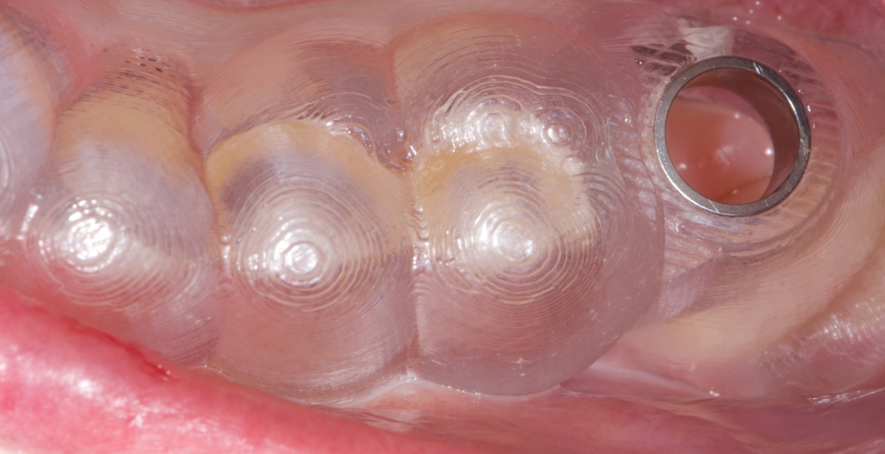
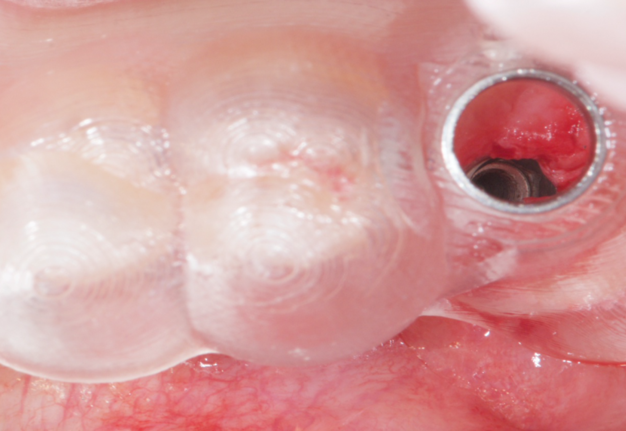
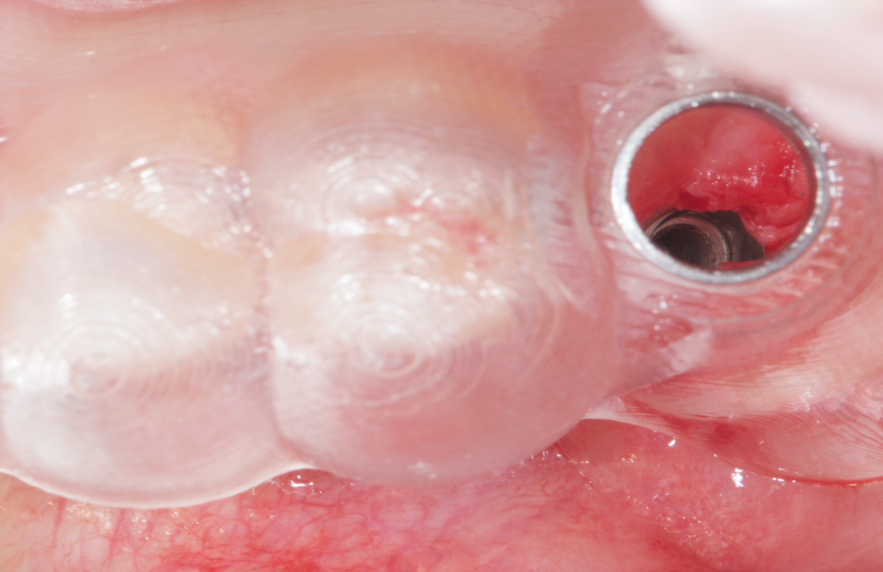
Under local anesthesia after the template had been placed, a flapless implant (Replace Tapered Groovy) was inserted using a torque of 35-45 Ncm (Fig 18A-B). The Figure 19 demonstrates panoramic radiography with flapless dental implant positioned into the beveled one-and-a-half-barrel fibula transplant.
A zirconium oxide crown was performed as a final dental restoration (Fig 20A-B).
Currently at 5-year follow-up (Fig 21), the patient is free from disease or relapses and her implant-supported prosthesis shows no signs of peri-implant bone resorption with full satisfaction from the patient.
DISCUSSION
An implant-supported fixed prosthesis represents a reliable option for stable and functional dental rehabilitation in osseous free flaps10. Individually, implant-based dental restorations in patients reconstructed with fibula flaps have been shown to confer many benefits, such as sufficient stabilization of the prosthesis, even in patients with marked irregularities of the hard and soft tissue anatomy, the possibility of compensating for smaller local soft tissues deficiencies, and contributing to an improved aesthetic result (i.e., by supporting the lip profile). Functional aspects, such as chewing, swallowing, and speech, are preserved much better than with conventional dentures. Unfortunately, many problems such as prosthetic guided implant positioning11,12, prosthesis encumbrance and soft tissue healing around implants13, arise when an implant-based prosthesis is planned for the rehabilitation of these patients14. These problems have been partially overcome with the use of computer guided implant placement in patients reconstructed with osseous free flaps with highly predictive dental implantation15–17.
Despite these improvements in oral dental rehabilitation it is very difficult to correct an insufficient or too large intermaxillary space, especially in the premolar region due to its particular shape. Usually the vertical occlusal dimension provides a minimum interocclusal distance of 2-4 mm, but it is difficult to predict in advance.
Failure to provide a sufficient prosthetic space may lead to discomfort, pain, and bone resorption while excessive free-way space may lead to discomfort from the temporomandibular joints, cheek-biting, angular cheilitis, and poor appearance18.
The main limiting feature of FFF therefore remains the residual discrepancy between native jaw and fibula graft, which causes aesthetic and functional problems.7,9,17
The fibula flap placement at the inferior border of the mandible yields excellent skeletal and soft-tissue contour but results in implant overloading, compromising long-term success.
In fact, the low height of the newly reconstructed mandible or maxillary bone leads to the need to use longer abutments to restore the occlusion, but in the same way excessive chewing forces will be discharged on the above abutments, the crown-implant relationship becomes unfavorable, which will produce instability of the same and invalidate the prosthetic-implant rehabilitation.19 To solve this problem, many surgeons have been driven to use one of following techniques: (1) placement of the fibula 0.5 to 1 cm higher than the inferior border of the remaining mandible in a functional relationship with the maxillary in order to recreate the alveolar ridge height,20,21 but to the detriment of inferior mandibular contour in which a step deformity remains, especially noticeable after radiotherapy; (2) using a single barrel fibula free flap and a low-profile reconstruction plate with dental implantation22 to achieve esthetic and functional mandibular reconstruction. However, this approach is selectively fashioned for patients with benign disease and adequate overlying soft tissue; (3) a double barrel fibular flap design has been proposed23,24 to overcome this problem, however it may result in excessive height that encroached on the prosthetic space, needing aggressive alveolopasty or extended below the inferior mandible border, worsening the facial height; (4) a 2-struct type of reconstruction in which a conventional vascularized fibular segment was placed at the inferior basal portion and a nonvascularized residual fibular segment4 or an iliac onlay bone graft25 was placed on the top of the fibula as onlay graft, which may lead to greater height resorption, however, infection and fistula formation, which can be disastrous for the patient if they occur; (5) alveolar vertical distraction of the FFF5–8,26–29 which, however, is associated with increased bone resorption processes during functional loading.
In every way the prosthodontic space, especially in the posterior mandibular area, may be excessively large or too small for proper occlusal guidance and dental restoration using traditional mandibular reconstruction techniques with single or double-barreled FFF even if vertical distraction is performed.
In 2013, a surgical team from Turkey9 described a new technique for restoring the height in the posterior fibular jaw area. A vascularized fibular flap was harvested and shaped so that a small piece of bone was removed in the middle to allow folding the flap, as usually done for a double-barrel technique. However, the distal half of the flap has been split longitudinally, and the bone segment away from the perforator vessels was removed. Then two remaining fibula segments, i.e. the “basal” and the split one, were folded and placed in parallel fashion to fit the defect. This technique was named by the authors “one-and-a-half-barrel” fibula free flap. Although it is a brilliant adaptive technique to solve the previous techniques disadvantages, we believe that the parallel orientation of the two pieces of the fibula leads to a still too high reconstruction that interferes with an adequate prosthetic restoration in premolar-molar area. Furthermore, the authors described the placement of three fixtures in their transplant, one year after removal removing the rigid internal fixation materials, but the description of planning and implant surgical procedure lacks technical details.
In 2022, a novel one-stage method for composite lateral head and neck reconstructions was introduced30. The report is illustrating how the chimeric lateral supramalleolar artery perforator (LSMAP) FFF31 can be modeled safely into a double-barrel shape. Although this new harvest technique allows the reconstruction of challenging lateral oro-mandibular defects thanks to raising of two independent skin paddles, the height of the neomandible does not allow adequate prosthetic rehabilitation in the premolar-molar area.
Furthermore, Saito et al8 appeal to the works of Bähr et al32 and He et al33 which stated that the bridging of mandibular defects of >9.0 cm in length is extremely challenging with the double-barrel technique due to the fact that the pedicle may be not long enough to reach the recipient vessels with increased risk of thrombosis by anastomosis with tension or vessels bridging limited fibula length of pedicle.
The possibility to customize the fibula free-flap reconstruction with virtual surgery planning in accordance with a pre-established dental wax-up is in our opinion a fundamental point in order to achieve the best final prosthesis.
The Synthes ProPlan® system allows preoperative planning, the study and production of specific surgical guides for accurate application of the reconstructive surgical plan and the CT guided flapless surgery by the NobelClinician® software allows precise positioning of the implant without the need to remove the plates and bone synthesis screws.
The “beveled one-a-half-barrel” technique combined with CT-guided implant surgery showed its usefulness in our practice.
The combination of these two useful technological tools, together with advanced reconstructive surgical skills, can allow three-dimensional mandibular reconstructions and aesthetic and long-lasting dental rehabilitations.
All fixtures survived. Satisfactory union was achieved in our case with no evidence of recurrence. The patient had adequate cosmetics, masticatory efforts and speech.
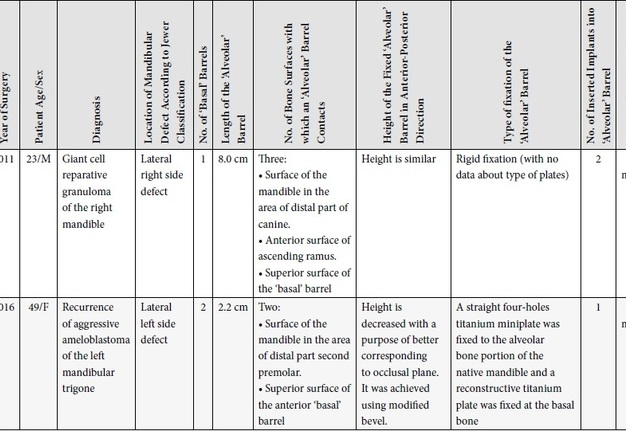
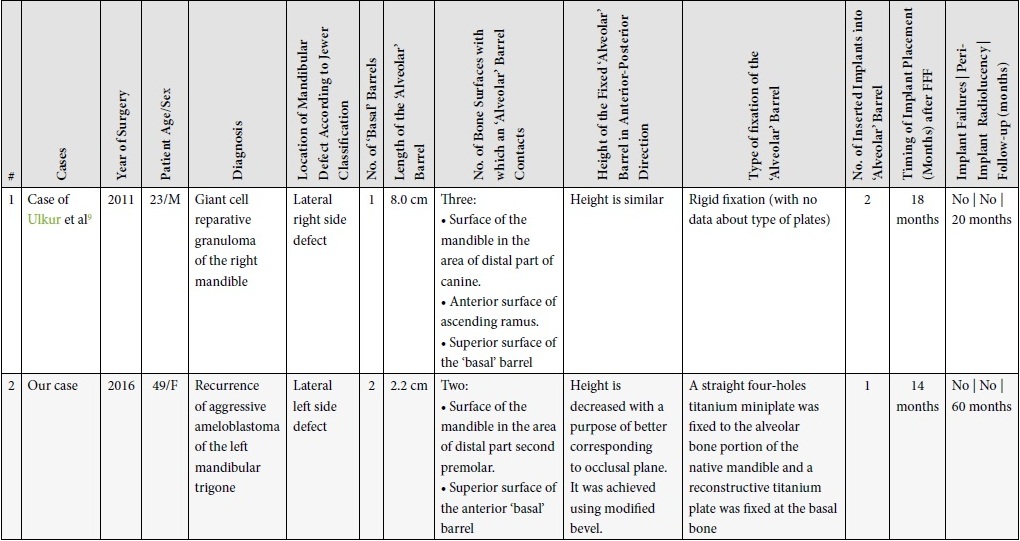
Our case have clearly confirmed the possibility of using “beveled one-a-half-barrel” FFF in reconstruction (fibula class 3: two osteotomies)21 of the long basal bone defect and alveolar bone with a needed length less than 9.0 cm. Comparison of two cases with dental implants placement into one-and-a-half barrel fibula free flaps, “longitudinal” and “beveled” respectively, is depicted in Table 1.
TABLE 1. Comparison of Two Cases with Dental Implants Placement into Longitudinal One-and-a-Half-Barrel Fibula Free Flap and into Beveled One-and-a-Half-Barrel Fibula Free Flap.
Based on the present study, the authors found that using the customized “beveled one-and-a-half barrel” FFF for the reconstruction of the posterior segmental mandible should be considered a cutting-edge technique that allows easily to follow the ideal position of the occlusal plane making the fixtures implantation more precise and long-lasting, markedly improving the facial symmetry and lower face plumpness in patients.
PATIENT CONSENT
The patient provided written consent for the use of her images.
AUTHOR CONTRIBUTIONS
Conceptualization: Massarelli O. Data acquisition: Meloni SM, Massarelli O. Data analysis, interpretation, and drafting of the manuscript: Massarelli O. Critical revision of the manuscript: Massarelli O, Meloni SM. Approval of the final version of the manuscript: both authors.
ACKNOWLEDGMENTS
We would like to thank Todd C. Hanna, MD, DDS, FACS from New York, New York, United States of America for the kind support in preparing the manuscript.
REFERENCES (33)
- Hidalgo DA. Fibula free flap: a new method of mandible reconstruction. Plast Reconstr Surg 1989;84(1):71–9. Medline | Google Scholar
- Sadove RC, Powell LA. Simultaneous maxillary and mandibular reconstruction with one free osteocutaneous flap. Plast Reconstr Surg 1993;92(1):141–6. Crossref | Medline | Google Scholar
- Horiuchi K, Hattori A, Inada I, Kamibayashi T, Sugimura M, Yajima H, Tamai S. Mandibular reconstruction using the double barrel fibular graft. Microsurgery 1995;16(7):450–4. Crossref | Medline | Google Scholar
- Lee JH, Kim MJ, Choi WS, Yoon PY, Ahn KM, Myung H, Hwang SJ, Seo BM, Choi JY, Choung PH, Kim SM. Concomitant reconstruction of mandibular basal and alveolar bone with a free fibular flap. Int J Oral Maxillofac Surg 2004;33(2):150–6. Crossref | Medline | Google Scholar
- Siciliano S, Lengelé B, Reychler H. Distraction osteogenesis of a fibula free flap used for mandibular reconstruction: preliminary report. J Craniomaxillofac Surg 1998;26(6):386–90. Crossref | Medline | Google Scholar
- Ortakoglu K, Suer BT, Ozyigit A, Ozen T, Sencimen M. Vertical distraction osteogenesis of fibula transplant for mandibular reconstruction: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;102(4):e8–11. Crossref | Medline | Google Scholar
- Cho-Lee GY, Naval-Gías L, Martos-Díaz PL, González-García R, Rodríguez-Campo FJ. Vertical distraction osteogenesis of a free vascularized fibula flap in a reconstructed hemimandible for mandibular reconstruction and optimization of the implant prosthetic rehabilitation. Report of a case. Med Oral Patol Oral Cir Bucal 2011;16(1):e74–8. Crossref | Medline | Google Scholar
- Saito N, Funayama A, Arai Y, Suda D, Takata Y, Kobayashi T. Vertical distraction osteogenesis of a reconstructed mandible with a free vascularized fibula flap: a report of two cases. Maxillofac Plast Reconstr Surg 2018;40(1):32. Crossref | Medline | Google Scholar
- Ulkur E, Karagoz H, Kulahci Y, Suer BT, Oksuz S, Kocyigit ID, Acikel C, Urhan M. One-and-a-half-barrel vascularized free fibular flap for the reconstruction of segmental mandibular defect. J Craniofac Surg 2013;24(2):e167–9. Crossref | Medline | Google Scholar
- Massarelli O, Hanna TC, Ganry L, Nagorniak IV, Fesenko II. Impact of surgeon`s Instagram television (IGTV): a case of chimeric fibula and soleus muscle transplant in a reconstruction of Cordeiro type IIIA total maxillectomy defect. J Diagn Treat Oral Maxillofac Pathol 2020;4(1):3–20. Crossref | Google Scholar
- Iizuka T, Häfliger J, Seto I, Rahal A, Mericske-Stern R, Smolka K. Oral rehabilitation after mandibular reconstruction using an osteocutaneous fibula free flap with endosseous implants. Factors affecting the functional outcome in patients with oral cancer. Clin Oral Implants Res 2005;16(1):69−79. Crossref | Medline | Google Scholar
- Hayter JP, Cawood JI. Oral rehabilitation with endosteal implants and free flaps. Int J Oral Maxillofac Surg 1996;25(1):3–12. Crossref | Medline | Google Scholar
- Meloni SM, Tallarico M, Canullo L, De Riu G., Massarelli O. Periimplant soft-tissue management in patients with a fibula free flap reconstruction: case series and description of a new technique. J Oral Science Rehabil 2016;2(4):26–30.
- Fernandes RP, Quimby A, Salman S. Comprehensive reconstruction of mandibular defects with free fibula flaps and endosseous implants. J Diagn Treat Oral Maxillofac Pathol 2017;1(1):6−10. Crossref | Google Scholar
- De Riu G, Meloni SM, Pisano M, Massarelli O, Tullio A. Computed tomography-guided implant surgery for dental rehabilitation in mandible reconstructed with a fibular free flap: description of the technique. Br J Oral Maxillofac Surg 2012;50(1):30–5. Crossref | Medline | Google Scholar
- Meloni SM, De Riu G, Pisano M, Massarelli O, Tullio A. Computer assisted dental rehabilitation in free flaps reconstructed jaws: one year follow-up of a prospective clinical study. Br J Oral Maxillofac Surg 2012;50(8):726–31. Crossref | Medline | Google Scholar
- Meloni SM, Tallarico M, De Riu G, Pisano M, Deledda A, Lolli FM, Massarelli O, Tullio A. Guided implant surgery after free-flap reconstruction: four-year results from a prospective clinical trial. J Craniomaxillofac Surg 2015;43(8):1348–55. Crossref | Medline | Google Scholar
- Jensen WO. Occlusion for the class II jaw relations patient. J Prosthet Dent 1990;64(4):432–4. Crossref | Medline | Google Scholar
- Chen J, Yin P, Li N, Wu L, Jian X, Jiang C. Functional mandibular reconstruction with double-barrel fibular flap and primary osseointegrated dental implants improve facial esthetic outcome. J Oral Maxillofac Surg 2019;77(1):218–25. Crossref | Medline | Google Scholar
- Wei FC, Santamaria E, Chang YM, Chen HC. Mandibular reconstruction with fibular osteoseptocutaneous free flap and simultaneous placement of osseointegrated dental implants. J Craniofac Surg 1997;8(6):513–21. Crossref | Medline | Google Scholar
- Smolka K, Kraehenbuehl M, Eggensperger N, Hallermann W, Thoren H, Iizuka T, Smolka W. Fibula free flap reconstruction of the mandible in cancer patients: evaluation of a combined surgical and prosthodontic treatment concept. Oral Oncol 2008;44(6):571–81. Crossref | Medline | Google Scholar
- Shen YF, Rodriguez ED, Wei FC, Tsai CY, Chang YM. Aesthetic and functional mandibular reconstruction with immediate dental implants in a free fibular flap and a low-profile reconstruction plate: five-year follow-up. Ann Plast Surg 2015;74(4):442–6. Crossref | Medline | Google Scholar
- Chang YM, Wallace CG, Tsai CY, Shen YF, Hsu YM, Wei FC. Dental implant outcome after primary implantation into double-barreled fibula osteoseptocutaneous free flap-reconstructed mandible. Plast Reconstr Surg 2011;128(6):1220–8. Crossref | Medline | Google Scholar
- Chang YM, Tsai CY, Wei FC. One-stage, double-barrel fibula osteoseptocutaneous flap and immediate dental implants for functional and aesthetic reconstruction of segmental mandibular defects. Plast Reconstr Surg 2008;122(1):14–5. Crossref | Medline | Google Scholar
- Kreusch T, Kerscher A, Behrens E. Maxillary and mandibular reconstruction with bone sandwich plasty and implants. Presented at the 8th International Congress on Reconstructive Preprosthetic Surgery; San Diego, CA; April 15, 1999.
- Cheung LK, Chua HD, Hariri F, Pow EH, Zheng L. Alveolar distraction osteogenesis for dental implant rehabilitation following fibular reconstruction: a case series. J Oral Maxillofac Surg 2013;71(2):255–71. Crossref | Medline | Google Scholar
- Chiapasco M, Brusati R, Galioto S. Distraction osteogenesis of a fibular revascularized flap for improvement of oral implant positioning in a tumor patient: a case report. J Oral Maxillofac Surg 2000;58(12):1434–40. Crossref | Medline | Google Scholar
- Nocini PF, Wangerin K, Albanese M, Kretschmer W, Cortelazzi R. Vertical distraction of a free vascularized fibula flap in a reconstructed hemimandible: case report. J Craniomaxillofac Surg 2000;28(1):20–4. Crossref | Medline | Google Scholar
- Wang F, Huang W, Zhang C, Sun J, Kaigler D, Wu Y. Comparative analysis of dental implant treatment outcomes following mandibular reconstruction with double-barrel fibula bone grafting or vertical distraction osteogenesis fibula: a retrospective study. Clin Oral Implants Res 2015;26(2):157–65. Crossref | Medline | Google Scholar
- Massarelli O. Chimeric LSMAP double-barrel fibula free flap: goal-oriented surgical technique and tips for one-stage mandibular reconstruction. Plast Reconstr Surg Glob Open 2022;10(1):e4040. Crossref | Medline | Google Scholar
- Massarelli O, Gobbi R, Biglio A, Soma D, Tullio A. Chimeric lateral supramalleolar artery perforator fibula free flap in the reconstruction of composite head and neck defects. Plast Reconstr Surg 2014;133(1):130–6. Crossref | Medline | Google Scholar
- Bähr W, Stoll P, Wachter R. Use of the “double barrel” free vascularized fibula in mandibular reconstruction. J Oral Maxillofac Surg 1998;56(1):38–44. Crossref | Medline | Google Scholar
- He Y, Zhang ZY, Zhu HG, Wu YQ, Fu HH. Double-barrel fibula vascularized free flap with dental rehabilitation for mandibular reconstruction. J Oral Maxillofac Surg 2011;69(10):2663–9. Crossref | Medline | Google Scholar