Case Report: Primary Mucosal Melanoma. An Extremely Rare Case in the Private Dental Practice
December 25, 2018
https://doi.org/10.23999/j.dtomp.2018.4.7
J Diagn Treat Oral Maxillofac Pathol 2018;2:186–9.
Under a Creative Commons license
How to cite this article
Feloniuk RV. Case report: primary mucosal melanoma. An extremely rare case in the private dental practice. J Diagn Treat Oral Maxillofac Pathol 2018;2(4):186−9.
Contents: Summary | Introduction | Case | Discussion | Conclusions | Conclusion | Acknowledgements | Confirmation Of Patient's Permission | References (15)
Summary
Mucosal melanoma (synonyms: oral melanoma, oral mucosal melanoma, and oral malignant melanoma) of the head and neck is a very rare and aggressive malignancy with a very poor prognosis [1, 2]. A 56-year-old white gentleman was referred to the private dental clinic with a darkly pigmented lesion on upper alveolar ridge, upper lip mucosa, and hard palate. That paper describes: differential diagnostics, classification of oral melanomas [10, 11] that differs from cutaneous melanomas, tumor–node–metastasis (TNM) staging of the oral mucosal melanoma [1, 2], and treatment options.
Introduction
Mucosal melanoma (synonyms: oral melanoma, oral mucosal melanoma, and oral malignant melanoma) of the head and neck is a very rare and aggressive malignancy with a very poor prognosis (Breik et al, 2016; Ascierto et al, 2017) [1, 2]. In the maxillofacial area the melanoma can be finded in mandible (Cervenka et al, 2017), parotid glands (Pain et al, 1986; Tymofieiev, 2012), nasal mucosa and maxillary sinuses (Maldonado-Mendoza et al, 2015; Breik et al, 2016; Shin and Kim, 2017), etc. [1, 3-7]. Tseng et al (2011) noted that among head neck melanomas face the is most frequently affected (48.1%) [8]. According to Chidzonga et al (2007), the primary oral mucosal malignant melanoma representing 0.2% to 8% of all melanomas [9]. The goal of this paper is demonstrate clinical features of the POMM that involved upper alveolar ridge, upper lip mucosa, and hard palate.
Case Report
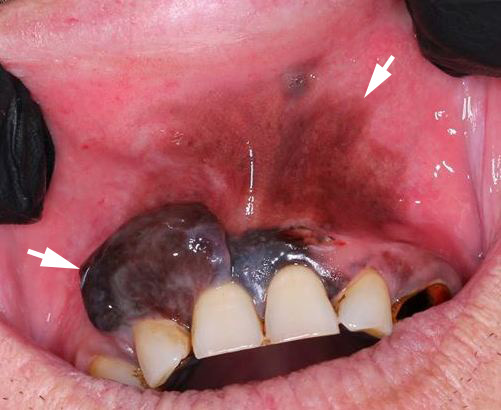
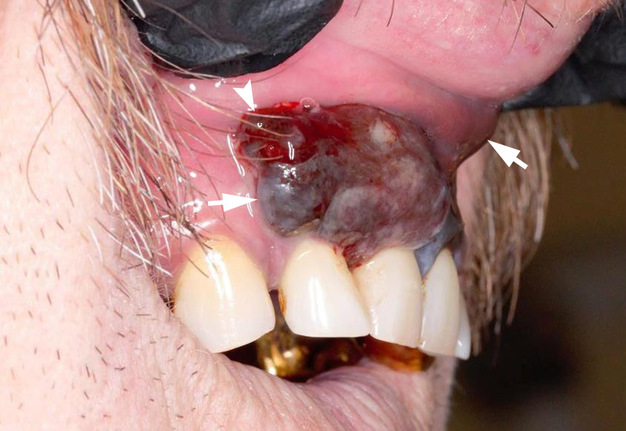
A 56-year-old white gentleman was referred to the private dental clinic with complaints for appearance of intraoral lesion (Fig 1) that had been present for three months and showed an extremely quick growth. Intraoral investigation showed a darkly pigmented lesion on upper alveolar ridge, upper lip mucosa, and hard palate. Similar to report of Magliocca et al (2006) in a patient of our clinic was no family history of melanoma [10]. After precise investigation of the lesion, medical history, and patients` complaints the patient was referred to the Head Neck Oncological Department. Where the diagnosis of primary mucosal melanoma was proved after incisional biopsy.
Discussion
Magliocca et al (2006) are strongly recommended that differential diagnosis should be made between different types of pigmented intraoral pathology such as [10]:
-
Drug disease or smoking associated melanosis;
-
Kaposi’s sarcoma;
-
Oral melanotic macule;
-
Physiologic or racial pigmentation;
-
Melanocytic nevus;
-
Melanoacanthoma.
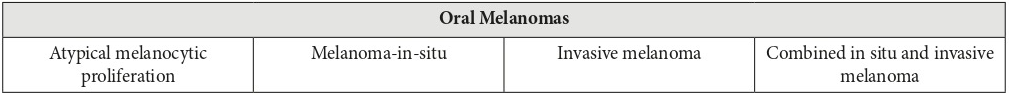
That case clearly confirms three predilections which were reported in the works of Barker et al (1997), Buchner et al (2004), and Magliocca et al (2006) [11, 12, 10]: 1) Most cases of melanoma occur between the 4th and 7th decades of life, with a mean age at 55–57 years; 2) A male predilection has been reported for oral mucosal melanoma; 3) Oral mucosal melanoma demonstrates a predilection for maxillary mucosa, with most cases appearing on keratinizing mucosa of the gingiva and palate. Discussing about possibility to use the classification of cutaneous melanomas the 1995 WESTOP Banff Workshop and Magliocca et al (2006) noted that oral melanoma should be classified in different manner and included 4 types [10, 11]. Which are presented in a Table 1.
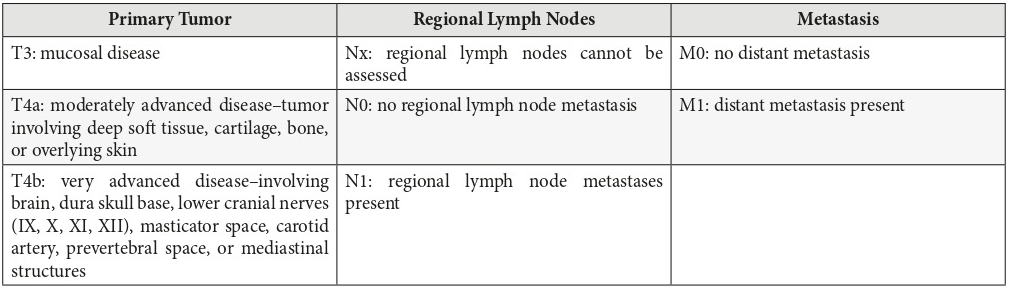
Bakkal et al (2015) and Breik et al (2016) are clearly demonstrating (Table 2) the American Joint Committee on Cancer TNM (tumor–node–metastasis) staging system [13, 1] that should be used upon treatment of that types of malignancy. Also, Bakkal et al (2015) are insisted that combination of radical surgical resection and adjuvant radiotherapy (RT) seems to be highly effective for local control [13]. The results of study Wushou et al (2015) suggest that post-operative radiotherapy (PORT) improves local-regional control but has no impact on overall status OS in head neck mucosa; melanomas patients [14]. Lopez et al (2016) argued that complete surgical resection with clear margins is the mainstay of primary oral melanoma management and may provide the best results, although the therapeutic strategy should be tailored individually according to tumor stage, location, and previous treatments [15]. Despite of all types of treatment prognosis is still very poor and stay at level of 5-20% (in a 5 year follow-up) from the moment of diagnosis.
Conclusions
All authors insisting that early detection of the melanoma, correct diagnosis according to the stage of that type of aggressive malignancy, and precise treatment can give the patient hope to get into the group of 5-20% of 5-year survival rate [10].
Acknowledgments
None.
Сonfirmation of patient’s permission
Written patient consent was obtained for publishing the clinical photographs.
References (15)
-
Breik O, Sim F, Wong T, Nastri A, Iseli TA, Wiesenfeld D. Survival outcomes of mucosal melanoma in the head and neck: case series and review of current treatment guidelines. J Oral Maxillofac Surg 2016;74(9):1859─71. Crossref
-
Ascierto PA, Accorona R, Botti G, Farina D, Fossati P, Gatta G, Gogas H, Lombardi D, Maroldi R, Nicolai P, Ravanelli M, Vanella V. Mucosal melanoma of the head and neck. Crit Rev Oncol Hematol 2017;112:136─52. Crossref
-
Cervenka PD, Perez L Jr, Perez DE, Jones B. Melanoma Metastasis to the Mandible-Case Report and Comprehensive Literature Review. J Oral Maxillofac Surg 2017;75(9):2025.e1-2025.e12. Crossref
-
Pain JA, Collier DSTJ, Conn PC. Malignant melanoma of a parotid lymph gland: An unusual case. Int J Oral Maxillofac Surg 1986;15(5):645–7. Crossref
-
Tymofieiev OO. Manual of maxillofacial and oral surgery [Russian]. 5th ed. Kyiv: Chervona Ruta-Turs; 2012.
-
Maldonado-Mendoza J, Ramı´rez-Amador V, Anaya-Saavedra G, Irigoyen-Camacho ME, Ruíz-Godoy L, Ruíz-García E, Meneses-García A. Clinicopathological characterization of primary oral and sinonasal melanoma in a referral centre in Mexico City: 2000–2012. Int J Oral Maxillofac Surg 2015;44(4):427–32. Crossref
-
Shin SH, Kim SG. Malignant melanoma occurred in maxillary sinus: case report with review of literature. Int J Oral Maxillofac Surg 2017;46(S1):294. Crossref
-
Tseng WH, Martinez SR. Tumor location predicts survival in cutaneous head and neck melanoma. J Surg Res 2011;167:192–8.
-
Chidzonga MM, Mahomva L, Marimo C, Makunike-Mutasa R. Primary malignant melanoma of the oral mucosa. J Oral Maxillofac Surg 2007;65(6):1117–20. Crossref
-
Magliocca KR, Rand MK, Su LD, Helman JI. Melanoma-in-situ of the oral cavity. Oral Oncology Extra 2006;42(1):46–8. Crossref
-
Barker BF, Carpenter WM, Daniels TE, Kahn MA, Leider AS, Lozada-Nur F, Lynch DP, Melrose R, Merrell P, Morton T, Peters E, Regezi JA, Richards SD, Rick GM, Rohrer MD, Slater L, Stewart JC, Tomich CE, Vickers RA, Wood NK, Young SK. Oral mucosal melanomas: the WESTOP Banff workshop proceedings. Western Society of Teachers of Oral Pathology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997;83(6):672–9.
-
Buchner A, Merrell PW, Carpenter WM. Relative frequency of solitary melanocytic lesions of the oral mucosa. J Oral Pathol Med 2004;33(9):550–7.
-
Bakkal FK, Başman A, Kızıl Y, Ekinci Ö, Gümüşok M, Ekrem Zorlu M, Aydil U. Mucosal melanoma of the head and neck: recurrence characteristics and survival outcomes. Oral Surg Oral Med Oral Pathol Oral Radiol 2015;120(5):575–80. Crossref
-
Wushou A, Hou J, Zhao YJ, Miao XC. Postoperative adjuvant radiotherapy improves loco-regional recurrence of head and neck mucosal melanoma. J Craniomaxillofac Surg 2015;43(4):553–8. Crossref
-
López F, Rodrigo JP, Cardesa A, Triantafyllou A, Devaney KO, Mendenhall WM, Haigentz M Jr, Strojan P, Pellitteri PK, Bradford CR, Shaha AR, Hunt JL, de Bree R, Takes RP, Rinaldo A, Ferlito A. Update on primary head and neck mucosal melanoma. Head Neck 2016;38(1):147–55. Crossref