Analysis of a First Unilateral and Then Bilateral Internal Jugular Vein Thrombosis in a Heroin User
October 31, 2019
https://doi.org/10.23999/j.dtomp.2019.10.2
J Diagn Treat Oral Maxillofac Pathol 2019;3:234−55.
Under a Creative Commons license
How to cite this article
Borodavko DS, Abramenko AV, Borodavko SP, Cherniak OS, Fesenko II. Analysis of a first unilateral and then bilateral internal jugular vein thrombosis in a heroin user. J Diagn Treat Oral Maxillofac Pathol 2019;3(10):234−55.
INSTITUTIONAL REPOSITORY
https://ir.kmu.edu.ua/handle/123456789/722
Contents: Summary | Introduction | Case | Discussion | Conclusions | Patient Consent | Fundings | Acknowledgements | References (56)
Summary
This report documents a first unilateral and then bilateral internal jugular vein (IJV) thrombosis as a result of repeated injections of heroin, which is rare in a practice of oral and maxillofacial surgeon. The patient was a 21-year-old male who was referred to a hospital with the diagnosis of phlegmon of the right neck. Emergency non-contrast computed tomography (5 images and 1 Supplemental Video are presented) revealed a hyperattenuating content in the lumen of expanded right IJV which fills its entire length. The patient received initial treatment according to the protocol. Ultrasound (US) (2 images and 2 Supplemental Videos are presented) in a first 24 hours supported the diagnosis describing a case as occlusive acute thrombosis. After 4 days of a positive dynamic the patient was transferred to outpatient mode. In a 10 day US examination (2 images and 2 Supplemental Videos are presented) simultaneously with positive changes in the lumen of a right IJV (partial clot lysis) an appearance of a left IJV thrombosis was noted. Analysis of thrombotic conditions of the neck, diagnostics methods, treatment options, and complications are performed.
INTRODUCTION
Internal jugular vein (IJV) thrombosis shortly is described as a thrombus in the lumen of the IJV vein.
Extended, this condition is described as intraluminal thrombus located in any part of the IJV length from the intracranial jugular vein to the junction of the IJV and subclavian vein.1
IJV thrombosis (IJVT) can be caused by: 1) malignant tumor,1, 2 2) central venous catheter, 3) deep neck space infection,2 4) intravenous drug abuse,2 5) antiphospholipid (Hughes) syndrome,3 etc.
Regardless of whether the IJV thrombosis accompanies with the signs of inflammation (fever, neck pain and swelling, leukocytosis, etc.)1 or not4 the diagnosis of thrombosis replaced such terms as thrombophlebitis (venous thrombosis with phlebitis) and phlebothrombosis (venous thrombosis without phlebitis).
Studies usually describe unilateral5 or bilateral4 IJVT in non-drug user cases. Limited reports dedicated to IJVT upon drug use.6 We present a unique case of a first unilateral and then bilateral internal jugular vein thrombosis in a 21-year-old chronic heroin user. Report is accompanied with clinical view of the patient, multislice CT scans, CT cine loops, US images, and four US videos in the dynamic of non-surgical treatment. The goals of our article are: 1) to train the maxillofacial surgeons in the ultrasound anatomy of the vascular-nerve bundle of the neck upon thrombosis and 2) to perform a revision of current terminology of thrombotic conditions at the neck.
CASE
A 21-year-old male was referred to the Kyiv Regional Clinical Hospital by physicians of two other medical institutions with a different diagnosis: phlegmon of the right neck and abscess of the neck. The main patients` complaints were severe fever, pain in the right neck, 6-day swelling, and extremely painful and complicated lateral movements of the head. Laboratory tests showed leukocytosis. Left neck was asymptomatic. Physical examination revealed two symmetrically arranged round-shape 0.4 × 0.4-cm nodules at the lower aspect of the neck (Fig 1). These nodules are the consequences of repeated injections of drug into the same part of the vein. And the drug users usually called it “mines” or “volcanoes.” According to the patient`s words he injected heroin during last 3 years.
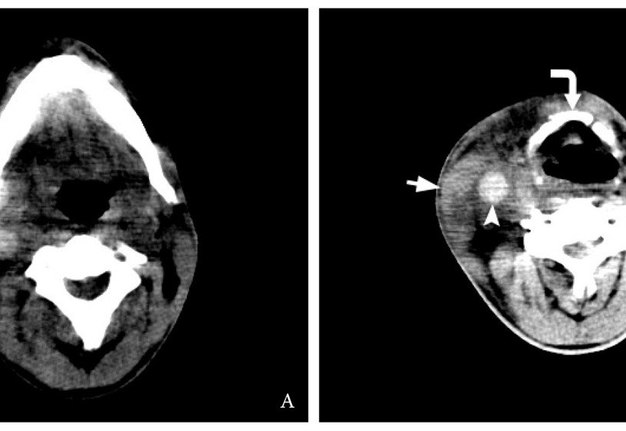
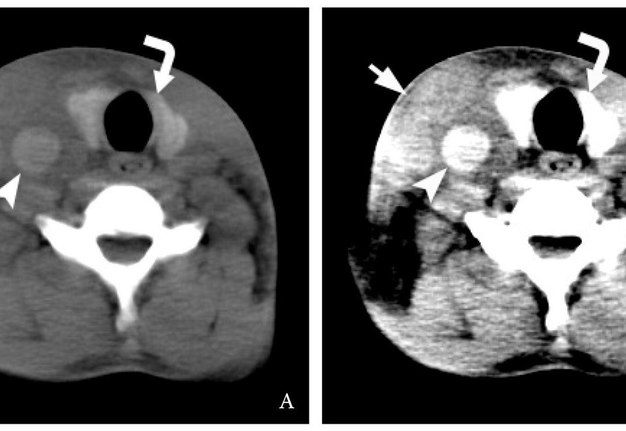
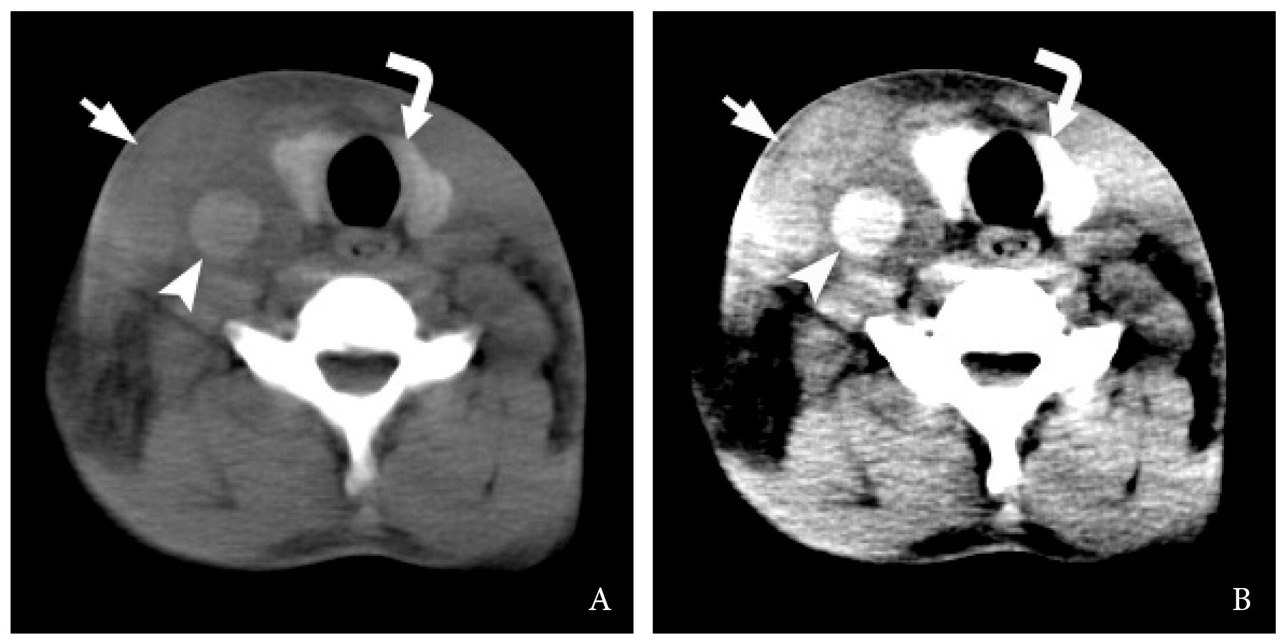
Emergency non-contrast multidetector computed tomography (MDCT) (General Electric, HiSpeed Dual) revealed a swelling of the right sternocleidomastoid muscle, subcutaneous tissues, and presence of thrombus filled the entire length of the expanded right IJV, from the level of mastoid process to the level of clavicle (Figs 2 and 3). The blood clot showed hyperdense appearance and was perfectly visualized on brain window of the MDCT. The attenuation values in a 0.4- cm2 measured intraluminal area were 69.4 ± 6.9 Hounsfield units (HU).
The Video 1 (Supplemental Video Content) demonstrates 16 consecutive non-contrast axial CT scans of the neck. Video 1 is available in the page of the full-text article on dtjournal.org and in the YouTube channel ‘‘Videos DTJournal,’’ available at Link. Total video`s duration: 23 sec. The analysis of CT images with different window settings revealed that the “brain window” is preferable to “head neck window” in diagnostics of IJV thrombosis upon non-contrast CT (Fig 4).
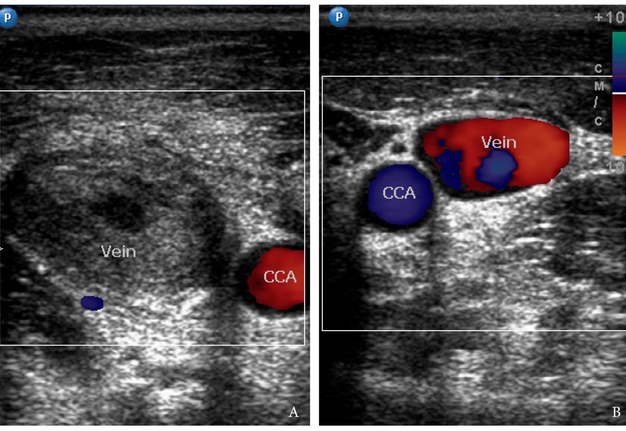
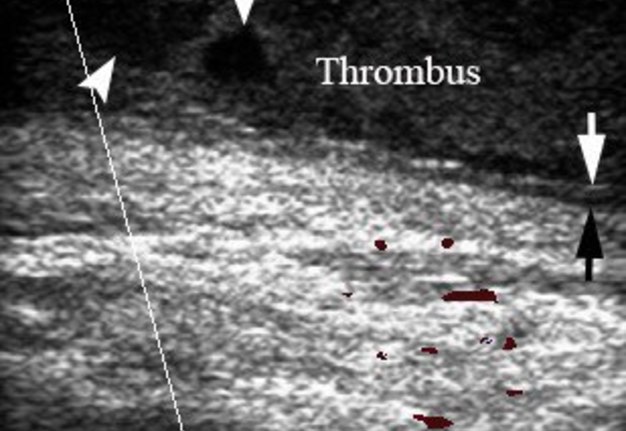
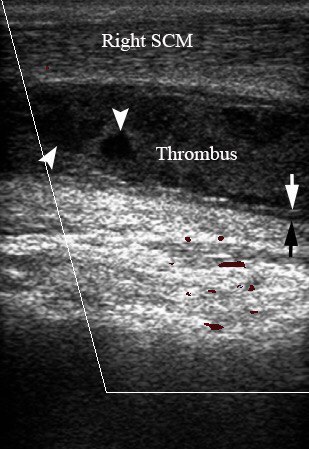
The gray scale (synonym: B-mode) and Doppler ultrasound (US) (model: HD11 XE, Philips) of the bilateral neck was performed by an experienced physician (O.S.C.; her experience in ultrasound investigation – 11 years) on the next morning after starting the medication therapy (intramuscular injections of ceftriaxone 1.0 g two times per day, anti-inflammatory medication, and probiotics) and compresses (ceftriaxone + dexamethasone + dimethyl sulfoxide solution) during first 24 hours. The gray scale and Doppler US showed complete obstruction of the distended right IJV by hypoechoic thrombus and no occlusion of the contralateral IJV (Fig 5). Right IJV was non-compressible with no mobile valves. The Video 2 (Supplemental Video Content) demonstrates condition of a right symptomatic side of the neck. Transverse gray scale ultrasound shows how the entire lumen of the right internal jugular vein is obliterated by thrombus (it has a heterogenous hypoechoic appearance) from lower to upper neck. Reactive lymph nodes with echogenic hilum and a swelled right sternocleidomastoid muscle are also visualized. Video 2 is available in the page of the full-text article on dtjournal.org and in the YouTube channel “Videos DTJournal,” available at Link. Total video`s duration: 3 sec. The Video 3 (Supplemental Video Content) depicts a gray scale sonograms obtained from longitudinal position of the probe respectively to the right subclavian vein. It demonstrates a sagging of the thrombus to the place where the right IJV unites with the right subclavian vein (anechoic tubular structure) and is going further as a right brachiocephalic vein. The IJV valve (visualized as a thin curved line at the lower aspect of the clot) does not allow the thrombus to penetrate below. Video 3 is available in the page of the full-text article on dtjournal.org and in the YouTube channel “Videos DTJournal,” available at Link. Total video`s duration: 4 sec.
FIGURE 1. Clinical view of a 21-year-old patient before treatment. Notes a forced tilt of the head to the right side. Movement of the head to the left side is extremely painful for the patient and it’s very difficult to turn his head completely to the left. Swelling of the right neck without erythema is indicated by arrowhead, bilateral “mines” (places of the repeated injections of a drug) – by arrows.
FIGURE 3. Non-contrast axial CT images (brain window) at the level of mandible (A) and hyoid bone (B) (curved arrow). Notes a hyperdense (synonym: hyperattenuated) content, ie thrombus (arrowhead), in the lumen of the right IJV. The attenuation values in a 0.4 cm2 of the measured intraluminal area was 69.4 ± 6.9 HU. A swelled right sternocleidomastoid muscle is indicated by arrow.FIGURE 3. Non-contrast axial CT images (brain window) at the level of mandible (A) and hyoid bone (B) (curved arrow). Notes a hyperdense (synonym: hyperattenuated) content, ie thrombus (arrowhead), in the lumen of the right IJV. The attenuation values in a 0.4 cm2 of the measured intraluminal area was 69.4 ± 6.9 HU. A swelled right sternocleidomastoid muscle is indicated by arrow.
VIDEO 1. Supplemental Video Content demonstrates 16 consecutive non-contrast axial CT scans (brain window) of the neck. Image at the level of clavicles (asterisks) showed hyperattenuated content (arrowhead), ie thrombus, in the lumen of the right IJV. Arrow – lower part of the swelled right sternocleidomastoid muscle. Video is available in the page of the full-text article on dtjournal.org and in the YouTube channel “Videos DTJournal,” available at https://youtu.be/CB9JAuM6tQE. Total video`s duration: 23 sec.
FIGURE 5. Comparison of transverse color Doppler sonograms of the right (A) and left (B) neurovascular bundles of the neck during first 24 hours after hospitalization. A: Notes an occlusive thrombus (T) in the right dilated IJV (vein) and a layered structure of the peripheral part of a clot. B: Left non-obstructed IJV (vein) has a typical appearance, its size two times smaller than an obstructed vein. CCA – common carotid artery.
VIDEO 2. Supplemental Video Content shows gray scale sonogram obtained from transversal position of the probe respectively to the neurovascular bundle of the neck. The entire lumen of the right internal jugular vein is obliterated by thrombus (has a heterogenous hypoechoic appearance and indicated as thrombus in a right IJV). Arrow – reactive lymph node with echogenic hilum (arrowhead), curved arrow – ramification (bifurcation) of the common carotid artery into external and internal carotid arteries (ECA and ICA), right SCM – a swelled right sternocleidomastoid muscle. Depth of US is 4.0 cm. Video is available in the page of the full-text article on dtjournal.org and in the YouTube channel “Videos DTJournal,” available at https://youtu.be/L6Cwe5RbqpU. Total video`s duration: 3 sec.
VIDEO 3. Supplemental Video Content shows a gray scale sonogram obtained from longitudinal position of the probe respectively to the right subclavian vein (Right SV). Sonogram demonstrates a sagging of the thrombus (T) to the place where the right IJV unites with the right subclavian vein (anechoic tubular structure) and is going further as a right brachiocephalic vein (its direction is labeled by a waved arrow). The IJV valve (visualized as a thin curved line [arrowhead] at the lower aspect of the clot) does not allow the thrombus to penetrate below. Arrow – a clavicular cortical bone surface. Depth of image is 4.0 cm. Video is available in the page of the full-text article on dtjournal.org and in the YouTube channel “Videos DTJournal,” available at https://youtu.be/thIfb-M7Sa8. Total video`s duration: 4 sec.
Anamnesis, clinical manifestations, and both investigations (CT and US) proved the diagnosis of a post-injective thrombosis of the right internal jugular vein (as a result of repeated puncture7 of IJV by intravenous heroin abuser). To the initial treatment we prescribed xarelto 15 mg (similar treatment strategy as in study of Corral et al)5 two times per day during first 21 days and 20 mg during next 3 months, detralex 1 tablet 2 times per day during 2 months.
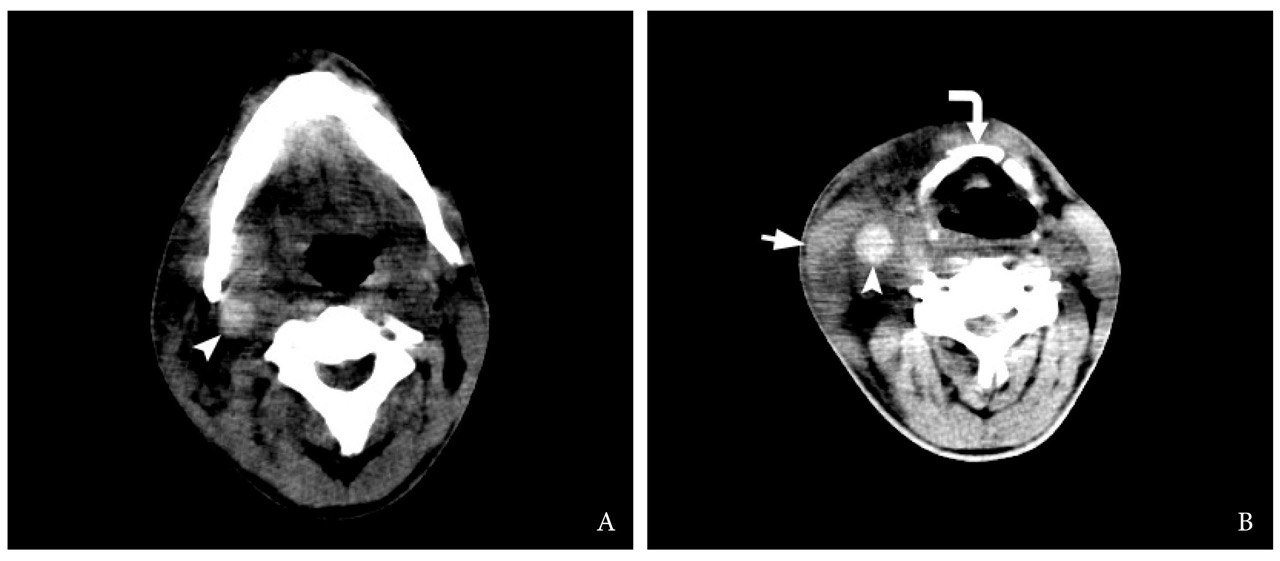
After 4 days of a positive dynamic the patient was transferred to outpatient mode. At 10 day follow-up, physical examination (Fig 6) of the patient showed no fever, pain and absence of neck swelling. A gray scale and color Doppler US (Fig 7) revealed a partial destruction of the thrombus in the lumen of right IJV, but recanalization of vein not happened yet and it is still obliterated.
The Video 4 (Supplemental Video Content) depicts a gray scale US of the thrombus`s condition within a right IJV with multiple foci of clot`s destruction and reactive lymph nodes. Artifacts of the edge shadowing and acoustic enhancement are labeled and perfectly visualized. Video 4 is available in the page of the full-text article on dtjournal.org and in the YouTube channel “Videos DTJournal,” available at Link. Total video`s duration: 4 sec.
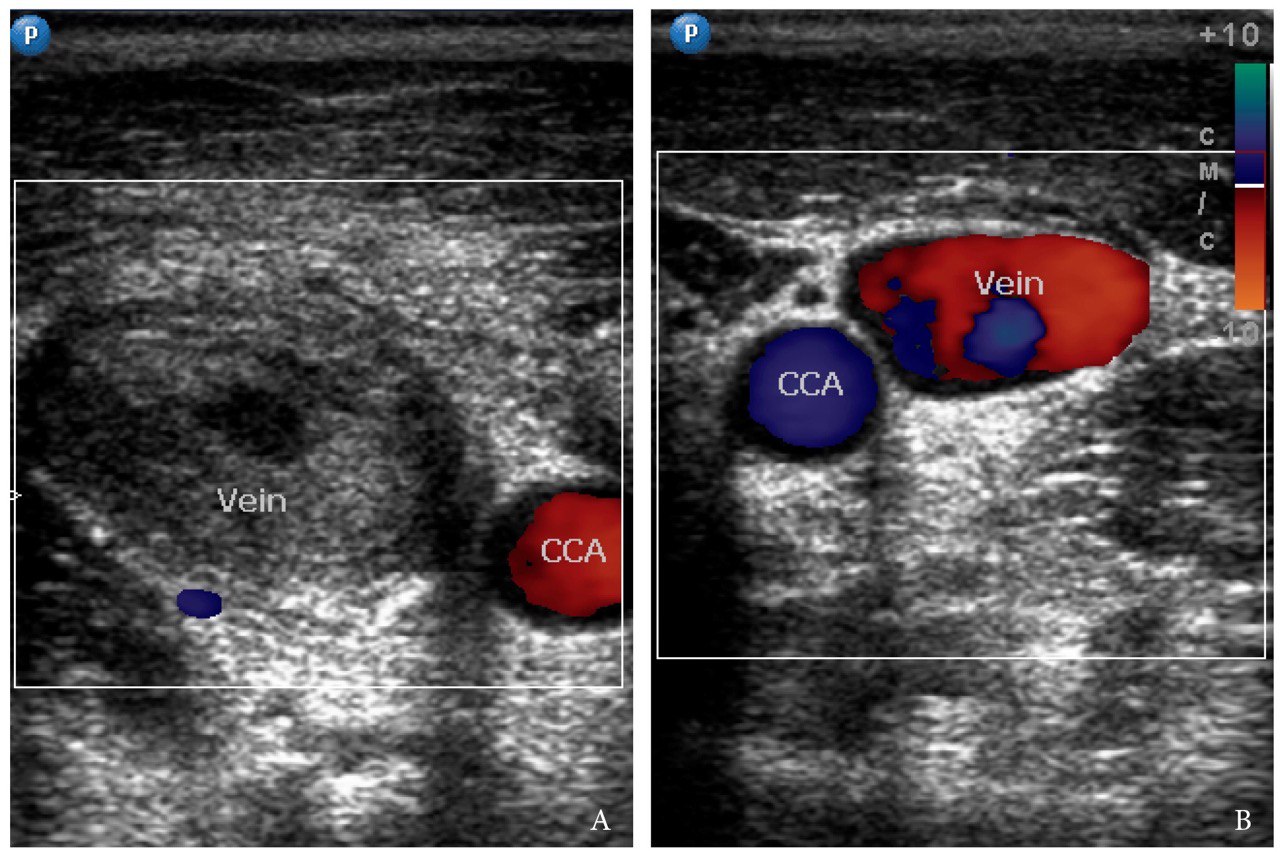
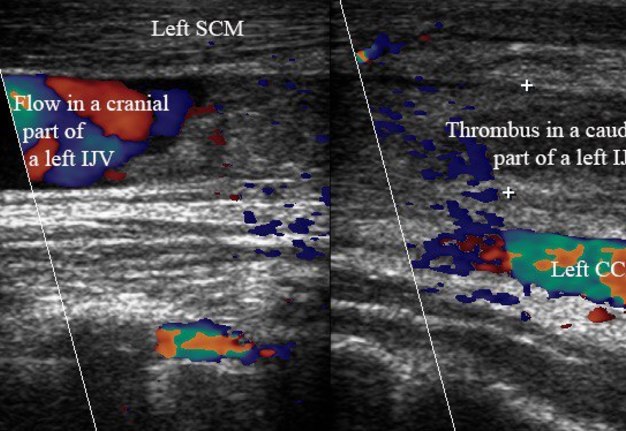
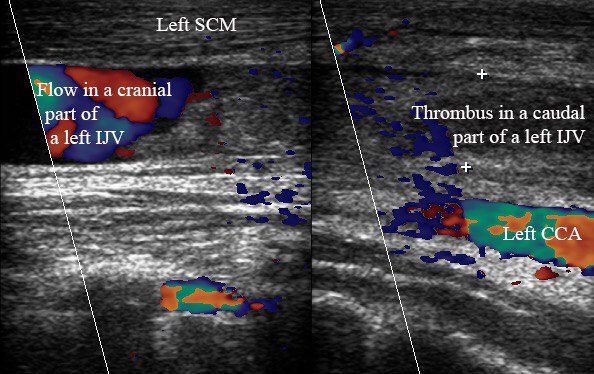
Performing US of the left neck, our team was surprised as it showed also an appearance of the left IJV thrombosis (Fig 8). The occlusive clot is located in the caudal part of the left IJV, filled the vein from its junction with subclavian vein to the level of ramification of the left common carotid artery into external and internal arteries. It’s indicated that patient, despite the prohibition to inject the drug, continue to do that inside the left IJV. The Video 5 (Supplemental Video Content) demonstrates a thrombus in a lumen of the left IJV. Video 5 is available in the page of the full-text article on dtjournal.org and in the YouTube channel “Videos DTJournal,” available at Link. Total video`s duration: 4 sec.
This thrombotic state at 10-days follow up led to the need of change the diagnosis from post-injective thrombosis of the right IJV into post-injective bilateral IJV thrombosis and to continue the treatment during the next three months.
DISCUSSION
This case represents a challenge in a treatment of drug abusers with internal jugular vein thrombosis by oral and maxillofacial surgeons. According to Chowdhuri et al trauma to the IJV from catheterization and repeated intravenous injections by drug users are the most frequent causes of thrombosis.8 The IJV thrombosis results from disturbance of pathophysiological mechanisms in Virchow’s triad of endothelial damage, stasis, and hypercoagulable state.9, 10 The report dedicated to analysis of physical and geographical injecting sites among injecting drug users11 stated that drug addicted persons are using neck as a possible site of drug injections in 10% of cases. Rafful et al emphasized that IJV thrombosis and deep neck infections in a neck injected drug users are requiring the medication therapy and possibly surgeries and other care procedures.12
TERMINOLOGY
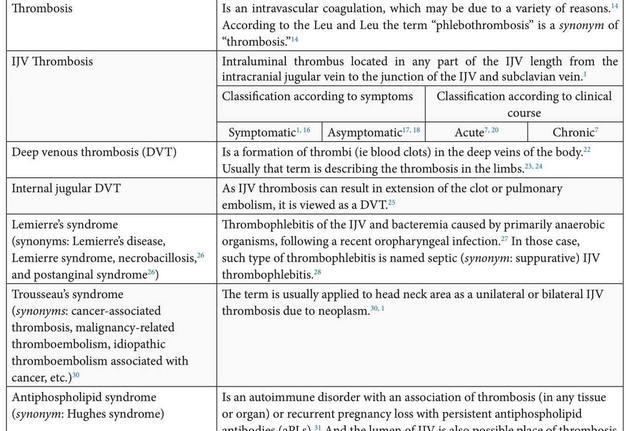
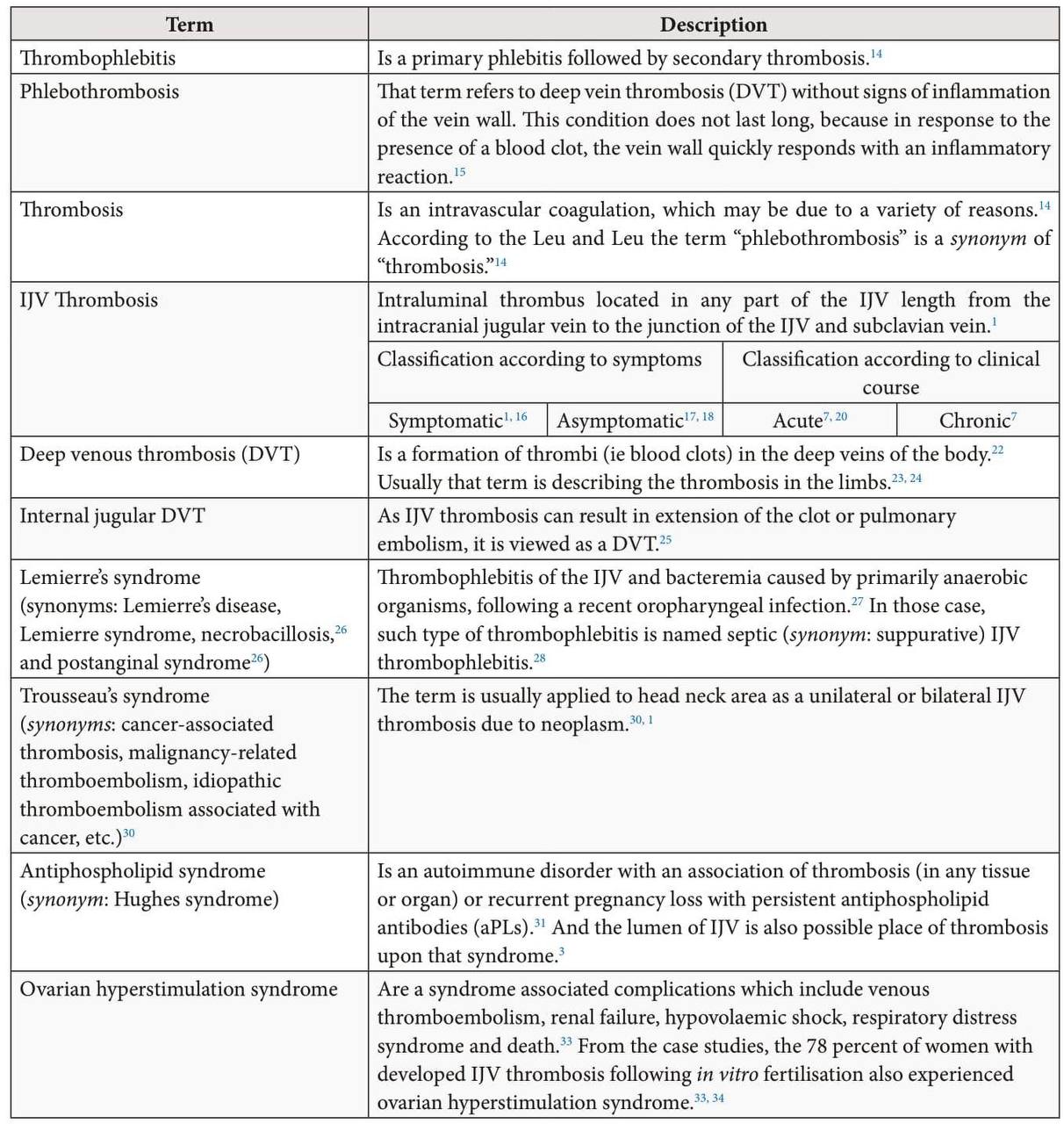
Thrombosis of the IJV can be termed by different names (Table 1), depending on the year of the publication, etiology, and clinical course. Ochsner in early 1950s stated that “phlebothrombosis” and “thrombophlebitis” are different in every respect except that in each there is a thrombus (ie clot) within the vein.13 In 1990s, Leu and Leu stated that “thrombosis” is an intravascular coagulation, which may be due to a variety of reasons.14 According to those two authors the term “phlebothrombosis” is a synonym of “thrombosis,’’14 Chur et al described “phlebothrombosis” as deep vein thrombosis (DVT) without signs of inflammation of the vein wall.15 In their opinion this condition does not last long, because in response to the presence of a blood clot, the vein wall quickly responds with an inflammatory reaction.15 Term “IJV thrombosis” precisely indicates on the clot`s location and described by Leci-Tahiri et al as intraluminal thrombus located in any part of the IJV.1
The symptomatic cases of IJV thrombosis are described in the reports of Tannenbaum et al and others.16, 1 The statement of Lønnebakken et al17 that clinical symptoms of IJVT may be vague and misleading or even absent17 indicated that it`s also reasonable to name thrombosis in those cases as asymptomatic. And as there is no signs of inflammation in several decades before such type of thrombotic condition usually named as phlebothrombosis. Tymofieiev, describing facial vein thrombophlebitis, stated that at first, the thrombus may be aseptic, and in these cases there are no signs of acute soft tissues inflammation, but later clot undergoes proteolysis, and its decayed parts, as well as the products of the metabolism of microorganisms, are absorbed into the blood accelerating signs of inflammation.19
FIGURE 6. Clinical view of a patient in 10 days after the initiated treatment, and prohibition for the patient to inject the drug. Visual swelling of the neck is absent; movements of the head are not limited and painless. Arrows – places of the repeated injections (drug users name them “mines” or “volcanoes”) of a drug (heroin). A right place of injections has decreased in size in two times comparing to the first visit of patient.
FIGURE 7. 10 days follow-up: Longitudinal color Doppler ultrasound of the right IJV. Partial destruction of the thrombus is indicated by arrowheads, the irregularity of inner surface of the thickened vein walls – arrows, right sternocleidomastoid muscle – Right SCM. Depth of US investigation is 5.0 cm.
VIDEO 4. 10 days follow up. Transverse gray scale sonograms (A, B) demonstrate condition of the thrombus within a right IJV with multiple foci of clot`s destruction (arrowheads). Curved arrow – reactive lymph node, arrows – artifact of edge shadowing, asterisk – artifact of acoustic enhancing, right SCM – right sternocleidomastoid muscle, ECA – external carotid artery, and ICA – internal carotid artery. Depth of ultrasonography is 4.0 cm. Video is available in the page of the full-text article on dtjournal.org and in the YouTube channel “Videos DTJournal,” available at https://youtu.be/3yUCamR6ZXU. Total video`s duration: 4 sec.
VIDEO 5. 10 days follow up. Transverse gray scale sonograms (A, B) demonstrate incidental finding a Thrombus in a lumen of the left IJV. In a caudal part of the vein the thrombus filled the entire lumen, in a cranial part – located near its posterior wall. Left CCA – left common carotid artery, Left SCM – left sternocleidomastoid muscle. The depth of US examination is 4.0 cm. Video is available in the page of the full-text article on dtjournal.org and in the YouTube channel ‘Videos DTJournal’, available at https://youtu.be/StjTB8erYaQ. Total video`s duration: 4 sec.
FIGURE 8. 10 days follow-up. Two combined long-axis color Doppler images (A, cranial part of the left neurovascular bundle of the neck; B, caudal part) from adjacent sections. Sonograms demonstrate occlusive thrombus in the lumen of caudal part of the left IJV. Notes a flow in non-occluded cranial part of the IJV. Left common carotid artery is labeled as Left CCA, left sternocleidomastoid muscle – Left SCM.
VIDEO 5. 10 days follow up. Transverse gray scale sonograms (A, B) demonstrate incidental finding a Thrombus in a lumen of the left IJV. In a caudal part of the vein the thrombus filled the entire lumen, in a cranial part – located near its posterior wall. Left CCA – left common carotid artery, Left SCM – left sternocleidomastoid muscle. The depth of US examination is 4.0 cm. Video is available in the page of the full-text article on dtjournal.org and in the YouTube channel ‘Videos DTJournal’, available at https://youtu.be/StjTB8erYaQ. Total video`s duration: 4 sec.
Rhys and Tajima et al applied the word “acute” describing a symptomatic IJV thrombosis.7, 20 And it is very common in English-language publications to divide DVT into acute (first 27 days) and chronic (28 days or longer) (synonym: post-thrombotic syndrome) form according to the clinical course.21 The authors and practitioners from some East-European countries categorize vein thrombosis into three forms: 1) acute(first 7-14 days), 2) subacute (from 14 to 30 days), and 3) chronic (more than 1 month).
Deep vein thrombosis (DVT) is a formation of thrombi (ie blood clots) in the deep veins of the body.22 That term is very popular in describing a thrombosis in the limbs.23, 24 As IJV thrombosis can result in extension of the clot or pulmonary embolism, it is viewed as a DVT.25
The literature also identifies 4 syndromes which are related (Lemierre’s) or may be related (Trousseau’s, antiphospholipid, and ovarian hyperstimulation syndromes) with a formation of thrombi in the lumen of IJVs.
Lemierre’s syndrome (synonyms: Lemierre’s disease, Lemierre syndrome, necrobacillosis,26 and postanginal syndrome26) is a IJV thrombophlebitis and bacteremia caused by primarily anaerobic organisms, following a recent oropharyngeal infection.27 In those case such type of thrombophlebitis is named septic (synonym: suppurative) IJV thrombophlebitis.28
Despite the fact that Trousseau's syndrome (synonyms: malignancy-related thromboembolism, idiopathic thromboembolism associated with cancer, etc.)29 have multiple definitions29 and is related to venous thromboses in patient with cancer of different locations, it is also applied to head neck cases of IJV thrombosis. And in such cases Trousseau’s syndrome (synonym: cancer-associated IJV thrombosis) defines a unilateral or bilateral IJV thrombosis due to neoplasm.30, 1
Antiphospholipid syndrome (synonym: Hughes syndrome) is an autoimmune disorder with an association of thrombosis (in any tissue or organ) or recurrent pregnancy loss with persistent antiphospholipid antibodies (aPLs).31 Publications indicate that lumen of IJV is also a possible place of thrombosis upon that syndrome.3, 32
Ovarian hyperstimulation syndrome is a syndrome associated complications which include venous thromboembolism, renal failure, hypovolaemic shock, respiratory distress syndrome and death.33 According to the case studies of Fleming et al, the 78 percent of women with developed IJV thrombosis following in vitro fertilisation also experienced ovarian hyperstimulation syndrome.33, 34
IJV ANATOMY
The IJV follows a course from the jugular foramen in the base of the skull to a point between the clavicular and sternal heads of the sternocleidomastoid muscle.35 At the lower part, IJV joins subclavian vein and forms a brachiocephalic vein (synonym: innominate veins).35 IJVs are helping to drainage the deoxygenated blood from the head.
Farina et al stated that IJV can have 1) typical “telescopic” appearance, 2) malformed valves and septa, and 3) hypoplastic vein appearance.36 To these three morphological types of IJV it is reasonable to add a fourth and fifth type of IJV, which are related to malformations: a duplication (unilateral37/bilateral38) of IJV and unilateral IJV agenesis39 (can be found in only 0.05-0.25 percent of population).
Dhanger et al emphasized that many physicians are still unaware of the presence of the valves in the IJV.40 Being the only valve between the brain and the heart, it plays a crucial role in preventing backward flow of blood in the vein.41 Venous valves are potential locations for a venous stasis24 and for a blood clot formation as a result of vessel injury during the injections of drug. Also, Raut noted that valve damage during catheterization forms a nidus to further clot formation.41
An autopsy data of Furukawa et al depict the statistics of valves based on 60 individuals: in 96.7% of cases valves were found bilaterally and in 3.3% of cases – unilaterally, in 46.6 percent of cases the position of valves was relative to the clavicle and in 53.4 percent – directly posterior to the clavicle.42 72% valves were bicuspid, 26.3% were unicuspid, and 1.7% were tricuspid.42 In the report of Raut, it is emphasized that anatomical position of IJV valve usually is at a distance of 0 to 26 mm proximal to the junction of the internal jugular and subclavian vein. 41 Lack of mobile venous valves is also one of the thrombosis signs. 7
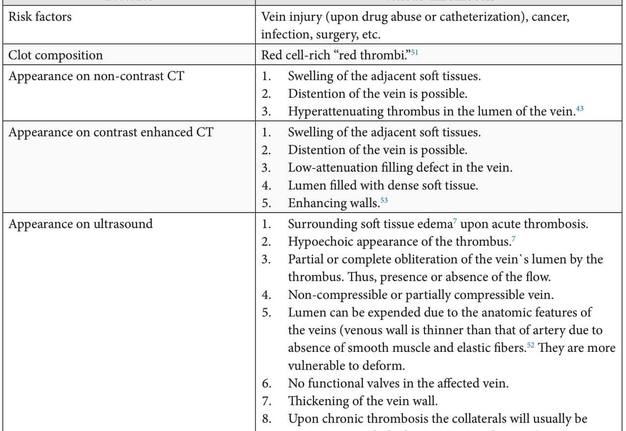
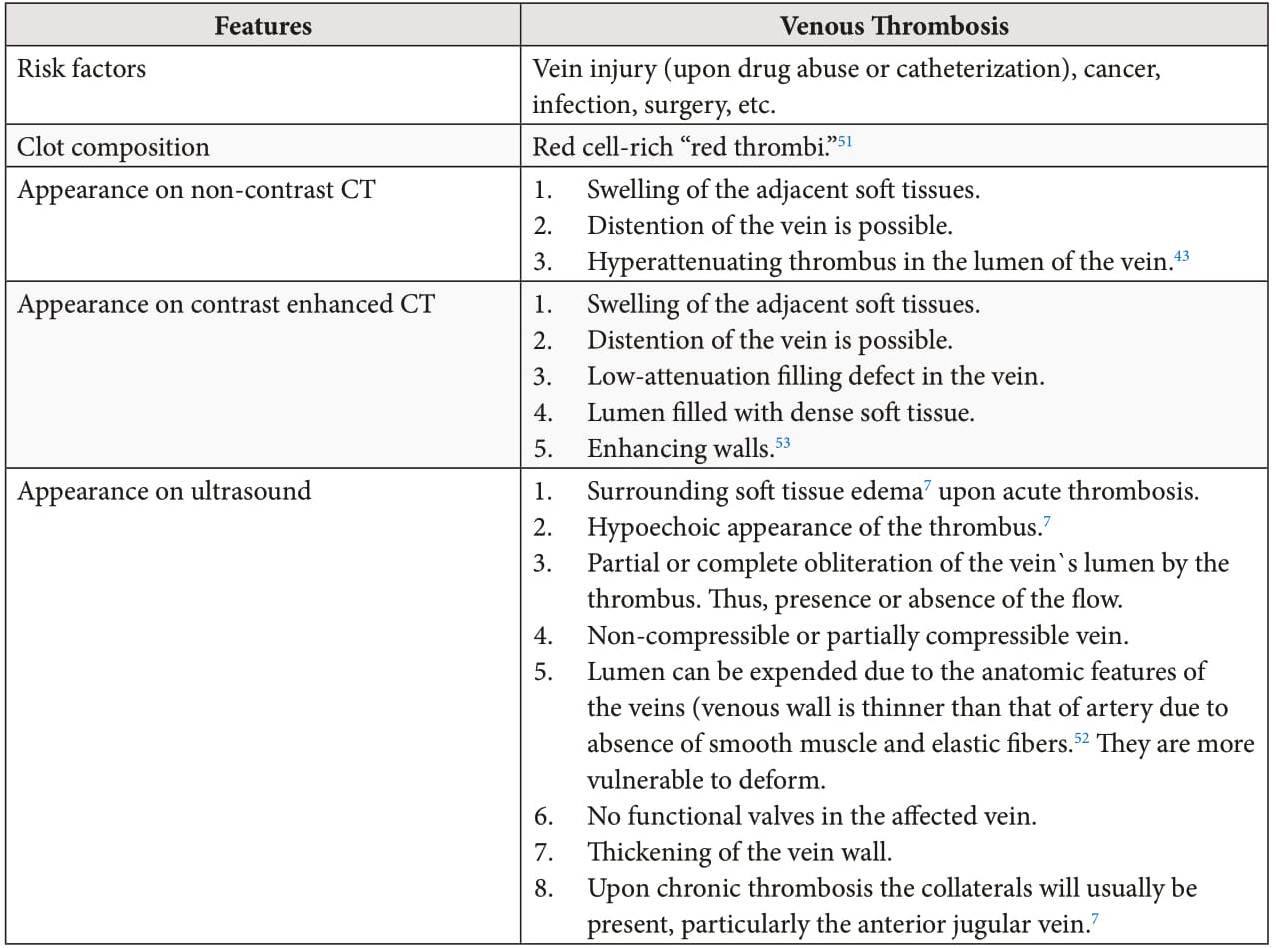
CONTRAST VS NON-CONTRAST CT
Similar to conclusion of Avsenik et al about noncontrast CT in case of cerebral venous sinus thrombosis, our case clearly proves that non-contrast multislice CT as an emergency examination has a high value for diagnosis of IJV thrombosis.43 Simultaneously with that statement, Leci-Tahiri et al and Tannenbaum et al insist on a need to perform contrast enhanced CT as it improves evaluation for acute bleeding and osseous injury and for additional pathologic conditions such as: 1) infection, 2) neoplasm, and 3) vascular dissection or thrombosis.1, 16
Windowing is a technique frequently used in the evaluation of CT scans to enhance contrast for the particular tissue or abnormality type being evaluated.44 Brain window can show differences among different types of soft tissues, such as brain, blood, vasculature, air-filled structures, and fluidcontaining spaces. 44 In our case, among 6 different CT window settings (chest, abdomen/pelvis, lung, brain, bone, and head neck) a good clot visualization during non-contrast CT analysis showed a head neck window and the best visualization – a brain window for a clear identification of the thrombus inside IJV.
IJV THROMBOSIS: ULTRASOUND APPEARANCE
Taking into account the advantages of US, it is important to understand the US appearance of thrombotic conditions in the neck tissues and monitor their state in dynamics. Rhys describes ultrasound appearance of both, acute and chronic IJV thrombosis.7
Thrombi have hypoechoic appearance.7 Partial destruction (hypoechoic areas) of the thrombus indicates the process of the resolution of the thrombus. IJVT as thrombosis in other veins can have occlusive or non-occlusive thrombus in the lumen of the vessel.45
The US appearance of free-floating thrombus (synonym: mobile thrombus) in the IJV is precisely described in report of Hsu et al.46
In our case, upon US examinations of the neurovascular bundles are usually visualized two artifacts: 1) edge shadowing and 2) posterior acoustic enhancement. According to Baad et al ‘edge shadowing’ is a refractive artifact that occurs at the edge of a significantly curved boundary (in our case boundaries of vessels) with a different speed of sound than that of the surrounding tissues.47
Artifact of edge shadowing can be noted at transverse gray scale sonograms in the next places: 1) edges of common carotid artery, 2) edges of external and internal carotid arteries and 3) edges of IJV (with or without colt in the lumen).
Artifact of the posterior acoustic enhancement (synonyms: acoustic enhancement48 and increased through transmission47) occurrs distal to lowattenuating structures (cystic formations, blood vessels,26 etc.). In our case this artifact occurred behind internal jugular veins and carotid arteries.
Reactive lymph nodes are also usually visualized on US upon IJV thrombosis with signs of inflammation. They look enlarged, with elongated form and marked echogenic hilus. Hilus is a part of lymph node where blood vessels enter and leave.49 Color and power Doppler shows increased hilar vascularity in the reactive lymph nodes.49
Deatrick et al suggested that the vein wall response is initiated early following the formation of the clot, and persists even in the presence of total resolution.50 Those conclusions were proved by the data of their study: the affected vein wall segment thickness in acute deep vein thrombosis cases measured 1.5-times greater than those in unaffected contralateral non thrombosed segments.50 At 6 months, a thickness can be 1.9-times greater than the measurable thickness in unaffected contralateral non-thrombosed vein segments.50
The multiplicity of an ultrasonography of the IJVs is as follows: in the absence of deterioration, the next US is done 1 week after the first examination, then another week, and later on as prescribed by the physician.15 Chur et al had emphasized that as a rule, the dynamics of thrombosis is already visible on the second US, and more often it is positive for the patient.15
Table 2 demonstrates a comparison of the IJV thrombosis characteristics upon different methods of investigation (non-contrast CT, contrastenhanced CT, and US).
DIFFERENTIAL DIAGNOSIS
Clinical symptoms of the symptomatic IJV thrombosis should be differentiated with 1) infection of the neck, 2) lymphadenitis, 3) external jugular vein thrombosis (which occurs both unilaterally45 and bilaterally54), and 4) benign clinical conditions of the neck (infected branchial cleft cyst, etc.), etc.
TREATMENT AND COMPLICATIONS
Corral and Villanueva supported the opinions described in the literature prescribing for IJV thrombosis cases an anticoagulation therapy from 3 to 6 months.5 In rare selected cases with initial thrombolysis, venous thrombectomy, or placement of a superior vena cava filter the anticoagulation is contraindicated.5
Analysis of Ascher et al based on 210 patients proved that patients with isolated internal jugular deep venous thrombosis have mortality and morbidity rates comparable to those of subclavian vein thrombosis.55 In their study was found that
among 210 patients the 21 patients (10 percent) were with IJVT only; and 61 patients (29 percent) with concomitant internal jugular and subclavian/ axillary deep venous thrombosis.55 The mortality rates for 12 month follow-up period were 42% for a group with IJV thrombosis only, and 59 percent for a group with concomitant internal jugular and subclavian/axillary deep venous thrombosis.55
In the study of Gbaguidi et al the two main complications of the IJV thrombosis were: postthrombotic syndrome (41.4 percent) and pulmonary embolism (10.3 percent).56 Boedecker et al indicate other possible complications such as sepsis with septic emboli to different organs and tissues as well as intracranial propagation of the thrombus with cerebral edema.2
PROGNOSIS
Chur et al emphasize that there are 3 ways in which the thrombosis can develop:15
- Thrombolysis and restoration of full/partial patency of the vein’s lumen.15
- Reorganization of the thrombus, ie its replacement by connective tissue elements with obstruction of the lumen of the vein with a substrate that intergrows with the vein and
- its removal becomes extremely difficult or impossible at all.15
In rare cases, purulent fusion of the thrombus occurs with the involvement of cellular tissue (cellulite), requiring drainage the purulent foci.15
CONCLUSIONS
A detailed report of our experience in diagnostics and treatment of a first unilateral and then bilateral internal jugular vein thrombosis in a chronic heroin user is presented. This article provides a practical overview (with 5 supplementary videos) of advantages of non-contrast CT and ultrasound upon different stages of thrombosis treatment, whatis critically important for oral and maxillofacial/ head and neck surgeons.
PATIENT CONSENT
Patient provided written consent for the use of his images.
FUNDINGS
No funding was received for this study.
ACKNOWLEDGMENTS
None.
REFERENCES(56)
- Leci-Tahiri L, Zherka-Saracini H, Tahiri A, Koshi A. Bilateral internal jugular vein thrombosis due to malignant tumor. J Med Case Rep 2018;12:42. Crossref
- Boedeker CC, Ridder GJ, Weerda N, Maier W, Klenzner T, Schipper J. Etiology and therapy of the internal jugular vein thrombosis [German]. Laryngorhinootologie 2004;83:743–9.
- Al-Zoubi NA. Spontaneous internal jugular vein thrombosis as primary presentation of antiphospholipid syndrome: case report. Vasc Health Risk Manag 2018;14:153–5. Crossref
- Wang S, Raio C, Nelson M. Bilateral internal jugular vein thrombosis. Crit Ultrasound J 2011;3:161–2. Crossref
- Corral J, Villanueva G. A case study of deep vein thrombosis of the right internal jugular vein in a healthy 21-year-old male. Case Rep Hematol 2016;2016:7654749. Crossref
- Lin D, Reeck JB, Murr AH. Internal jugular vein thrombosis and deep neck infection from intravenous drug use: management strategy. Laryngoscope 2004;114:56–60. Crossref
- Rhys R. Ultrasound of the neck. In: Allan PL, Baxter GM, Weston MJ, editors. Clinical Ultrasound, 3rd ed. Churchill Livingstone, 2011:890–919. Crossref
- Chowdhury K, Bloom J, Black MJ, al-Noury K. Spontaneous and nonspontaneous internal jugular vein thrombosis. Head Neck 1990;12:168–73.
- Khaladkar S, Chauhan A, Ghosh A, Jain K, Chauhan S. Internal jugular vein thrombosis in isolated tuberculous cervical lymphadenopathy. Case Rep Radiol 2016;2016:5184196. Crossref
- Erkoç R, Uzun K, Yuca K, Etlik Ö, Doğan E, Sayarlıoğlu H, İşlek A, Çankaya H. Internal jugular vein thrombosis two different etiologies. Eur J Gen Med 2005;2:123–8.
- Darke S, Ross J, Sharlene K. Physical and geographical injecting sites among injecting drug users. 1999.
- Rafful C, Wagner KD, Werb D, González-Zúñiga PE, Verdugo S, Rangel G, Strathdee SA. Prevalence and correlates of neck injection among people who inject drugs in Tijuana, Mexico. Drug Alcohol Rev 2015;34:630–6. Crossref
- Ochsner A. Thrombophlebitis and phlebothrombosis. Med Clin 1953;37:1113–8. Crossref
- Leu HJ, Leu AJ. Phlebosclerosis, phlebothrombosis, and thrombophlebitis: a current perspective. Cardiovasc Pathol 1996;5:183–92.
- Chur NN, Kondratenko HH, Kazuschyk VL. Phlebotrombosis and thrombophlebitis of the lower extremities. [Russian]. 1st ed. Minsk: educational institution “Belarusian State Medical University”; 2013.
- Tannenbaum LI, April MD, Watts RE, Pearson NM. Thrombosis of the internal jugular vein. Intern Emerg Med 2016;11:487–8. Crossref
- Lønnebakken MT, Pedersen OM, Andersen KS, Varhaug JE. Incidental detection of internal jugular vein thrombosis secondary to undiagnosed benign substernal goiter. Case Rep Med 2010;2010:645193. Crossref
- Kannabiran N, Thangaswamy CR. Incidental detection of idiopathic internal jugular vein thrombus in pediatric patient-lessons learnt! J Anaesthesiol Clin Pharmacol 2018;34:548–50. Crossref
- Tymofieiev OO. Manual of maxillofacial and oral surgery [Russian]. 5th ed. Kyiv: Chervona Ruta-Turs; 2012.
- Tajima H, Murata S, Kumazaki T, Ichikawa K, Tajiri T, Yamamoto Y. Successful interventional treatment of acute internal jugular vein thrombosis. AJR Am J Roentgenol 2004;182:467–9. Crossref
- Saha P, Black S, Breen K, Patel A, Modarai B, Smith A. Contemporary management of acute and chronic deep venous thrombosis. Br Med Bull 2016;117:107- 20. Crossref
- Kesieme E, Kesieme C, Jebbin N, Irekpita E, Dongo A. Deep vein thrombosis: a clinical review. J Blood Med 2011;2:59–69. Crossref
- Needleman L, Cronan JJ, Lilly MP, Merli GJ, Adhikari S, Hertzberg BS, DeJong MR, Streiff MB, Meissner MH. Ultrasound for lower extremity deep venous thrombosis: multidisciplinary recommendations from the Society of Radiologists in Ultrasound Consensus Conference. Circulation 2018;137:1505–15. Crossref
- Stone J, Hangge P, Albadawi H, Wallace A, Shamoun F, Knuttien GM, Naidu S, Oklu R. Deep vein thrombosis: pathogenesis, diagnosis, and medical management. Cardiovasc Diagn Ther 2017;7(Suppl 3):S276–S284. Crossref
- Rivard AB, Burns B. Anatomy, head and neck, internal jugular vein. [Updated 2018 Dec 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: Medline
- Bansal AG, Oudsema R, Masseaux JA, Rosenberg HK. US of pediatric superficial masses of the head and neck. Radiographics 2018;38:1239–63. Crossref
- Eilbert W, Singla N. Lemierre's syndrome. Int J Emerg Med 2013;6:40. Crossref
- Alperstein A, Fertig RM, Feldman M, Watford D, Nystrom S, Delva G, Muddassir S. Septic thrombophlebitis of the internal jugular vein, a case of Lemierre's syndrome. Intractable Rare Dis Res 2017;6:137–40. Crossref
- Varki A. Trousseau's syndrome: multiple definitions and multiple mechanisms. Blood 2007;110:1723–9. Crossref
- Bandara AR, Wimalarathna H, Kalupahana R, Gunathilake SS. Internal jugular venous thrombosis due to Trousseau's syndrome as the presenting feature of metastatic prostate carcinoma: a case report. J Med Case Rep 2016;10:104. Crossref
- Farmer-Boatwright MK, Roubey RA. Venous thrombosis in the antiphospholipid syndrome. Arterioscler Thromb Vasc Biol 2009;29:321–5. Crossref
- Agrawal A, Bajaj D, Ruben M, George J. Idiopathic internal jugular vein and subclavian vein thrombosis: a rare case report. Cureus 2019;11:e4005. Crossref
- Schanzer A, Rockman CB, Jacobowitz GR, Riles TS. Internal jugular vein thrombosis in association with the ovarian hyperstimulation syndrome. J Vasc Surg 2000;31:815–8. Crossref
- Belaen B, Geerinckx K, Vergauwe P, Thys J. Internal jugular vein thrombosis after ovarian stimulation: case report. Hum Reprod 2001;16:510–512, Crossref
- Hatfield A, Bodenham A, Ultrasound for central venous access. Contin Educ Anaesth Crit Care Pain 2005;5:187– 90. Crossref
- Farina M, Novelli E, Pagani R. Cross-sectional area variations of internal jugular veins during supine head rotation in multiple sclerosis patients with chronic cerebrospinal venous insufficiency: a prospective diagnostic controlled study with duplex ultrasound investigation. BMC Neurol 2013;13:162. Crossref
- Nayak SP, Ashraf M, Dam A, Biswas J. Internal jugular vein duplication: review and classification. Indian J Surg Oncol 2017;8:222–6. Crossref
- Downie SA, Schalop L, Mazurek JN, Savitch G, Lelonek GJ, Olson TR. Bilateral duplicated internal jugular veins: case study and literature review. Clin Anat 2007;20:260–6. Crossref
- Filograna L, Calcagni A, Rossi G, Di Stefano C, Beninati E, Collura A, Floris R. Internal jugular vein agenesis: a rare vascular abnormality and incidental finding. A case of internal jugular vein agenesis in a 52-years old male. Radiol Case Rep 2019;14:452–5. Crossref
- Dhanger S, Vaidiyanathan B, Tripathy DK. Internal jugular venous valve: well-known but mostly neglected. Indian J Anaesth 2016;60:602–3. Crossref
- Raut MS. Internal jugular vein valve—not to be ignored. J Cardiothorac Vasc Anesth 2017;31:e87–e88. Crossref
- Furukawa S, Wingenfeld L, Takaya A, Nakagawa T, Sakaguchi I, Nishi K. Morphological variations of the internal jugular venous valve. Anat Physiol 2012;2:108. Crossref
- Avsenik J, Oblak JP, Popovic KS. Non-contrast computed tomography in the diagnosis of cerebral venous sinus thrombosis. Radiol Oncol 2016;50:263– 8. Crossref
- Xue Z, Antani S, Long LR, Demner-Fushman D, Thoma GR. Window classification of brain CT images in biomedical articles. AMIA Annu Symp Proc 2012;2012:1023–9.
- Tojo Villanueva C, Ruiz Ruiz J. Idiopathic external jugular vein thrombosis. EJCRIM 2019;6. Crossref
- Hsu YH, Hsu HT, Cheng KI. Ultrasound detection of free-floating thrombus during internal jugular vein catheterisation. Br J Anaesth 2018;120:882–3. Crossref
- Baad M, Lu ZF, Reiser I, Paushter D. Clinical significance of US artifacts. Radiographics 2017;37:1408–23. Crossref
- Henderson M, Dolan J, Challenges, solutions, and advances in ultrasound-guided regional anaesthesia. BJA Education 2016;16:374–80. Crossref
- Ahuja AT, Ying M. Sonographic evaluation of cervical lymph nodes. AJR Am J Roentgenol 2005;184:1691–9. Crossref
- Deatrick KB, Elfline M, Baker N, Luke CE, Blackburn S, Stabler C, Wakefield TW, Henke PK. Postthrombotic vein wall remodeling: preliminary observations. J Vasc Surg 2011;53:139–46.Crossref
- Lowe GD. Common risk factors for both arterial and venous thrombosis. Br J Haematol 2008;140:488–95. Crossref
- Li M, Sun Y, Chan CC. Fan C, Ji X, Meng R. Internal jugular vein stenosis associated with elongated styloid process: five case reports and literature review. BMC Neurol 2019;19:112. Crossref
- Albertyn LE, Alcock MK. Diagnosis of internal jugular vein thrombosis. Radiology 1987;162:505–8. Crossref
- Hindi Z, Fadhel E. Idiopathic bilateral external jugular vein thrombosis. Am J Case Rep 2015;16:554– 7. Crossref
- Ascher E, Salles-Cunha S, Hingorani A. Morbidity and mortality associated with internal jugular vein thromboses. Vasc Endovascular Surg 2005;39:335–9. Crossref
- Gbaguidi X, Janvresse A, Benichou J, Cailleux N, Levesque H, Marie I. Internal jugular vein thrombosis: outcome and risk factors. QJM 2011;104:209–19. Crossref