Comprehensive Reconstruction of Mandibular Defects with Free Fibula Flaps and Endosseous Implants
February 18, 2017
https://doi.org/10.23999/j.dtomp.2017.1.1
J Diagn Treat Oral Maxillofac Pathol 2017;1:6−10.
Under a Creative Commons license
HOW TO CITE THIS ARTICLE
Fernandes RP, Quimby A, Salman S. Comprehensive reconstruction of mandibular defects with free fibula flaps and endosseous implants. J Diagn Treat Oral Maxillofac Pathol 2017;1(1):6−10.
Contents: Abstract | Introduction | Patients and Methods | Results | Discussion | Conclusions | References (17)
Abstract
Purpose: The goal of this paper is to review the use of fibula free flaps in reconstruction of various mandibular defects, as well as illustrate that placement of dental implants into free fibula flaps is a viable option ensuring a superior functional outcome.
Patients and Methods: Nine of patients with mandibular fibula free flap reconstruction who underwent dental implant placement were included in this study to demonstrate the versatility of this reconstructive technique.
Results: In all nine patients, fibula flaps provided adequate bone stock for implant placement. All 30 implants were placed in bicortical fashion and none had issues with primary stability at the time of placement.
Conclusion: Fibula free flap reconstruction is the treatment of choice for patients with various disease processes resulting in significant mandibular defects and can ultimately be restored with fixed dental prostheses.
Introduction
The advent of microvascular surgery facilitated the development of novel techniques that provided superior esthetic and functional reconstruction of large maxillofacial defects. One of the major advantages of microvascular free tissue transfer is that it contains its own vascular pedicle, thus allowing for improved healing in wounds compromised by radiation and chronic infection.1 The goal of any reconstructive surgery is to restore natural form and function. Mandibular defects resulting from ablative surgery due to malignant or benign pathology, osteonecrosis, or trauma often result in significant functional and esthetic compromise. The free fibula flap is considered the gold standard for mandibular reconstruction due to its versatility, outcome predictability, and suitability for dental implant placement.2 Dental rehabilitation plays a pivotal role in improving patient’s quality of life, since edentulism has been shown to result in significant psychological morbidity to patients.3
The goal of this paper is to review the use of fibula free flaps in reconstruction of various mandibular defects, as well as illustrate that placement of dental implants into free fibula flaps is a viable option ensuring a superior functional outcome.
Patients and Methods
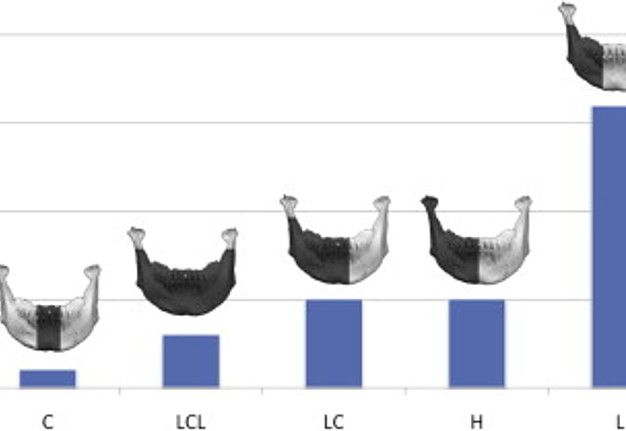
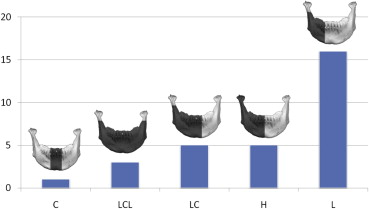
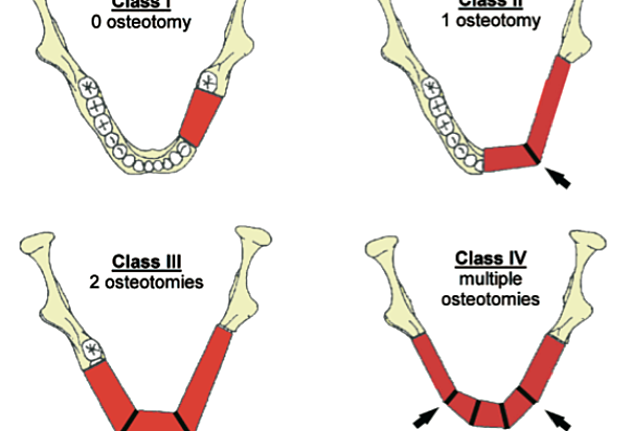
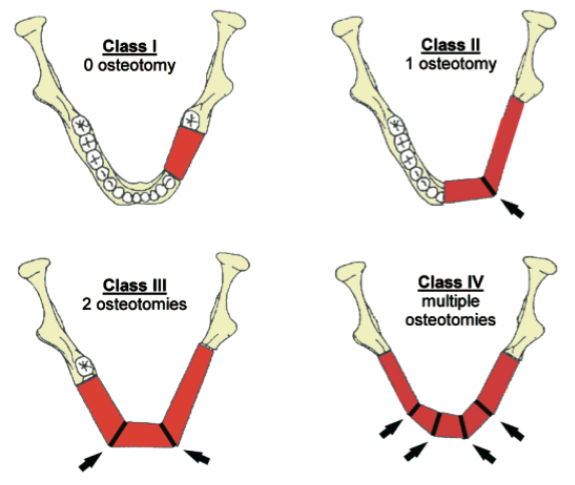
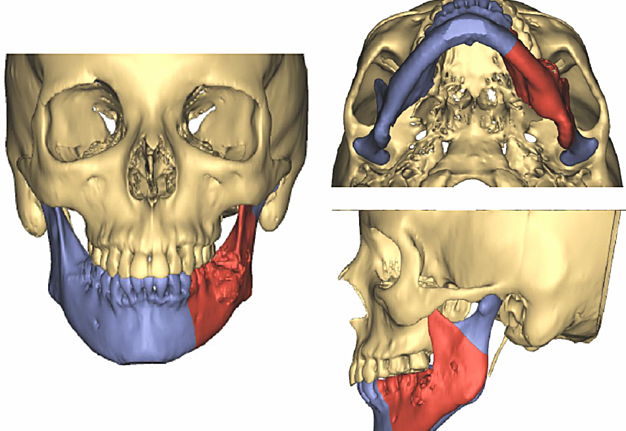
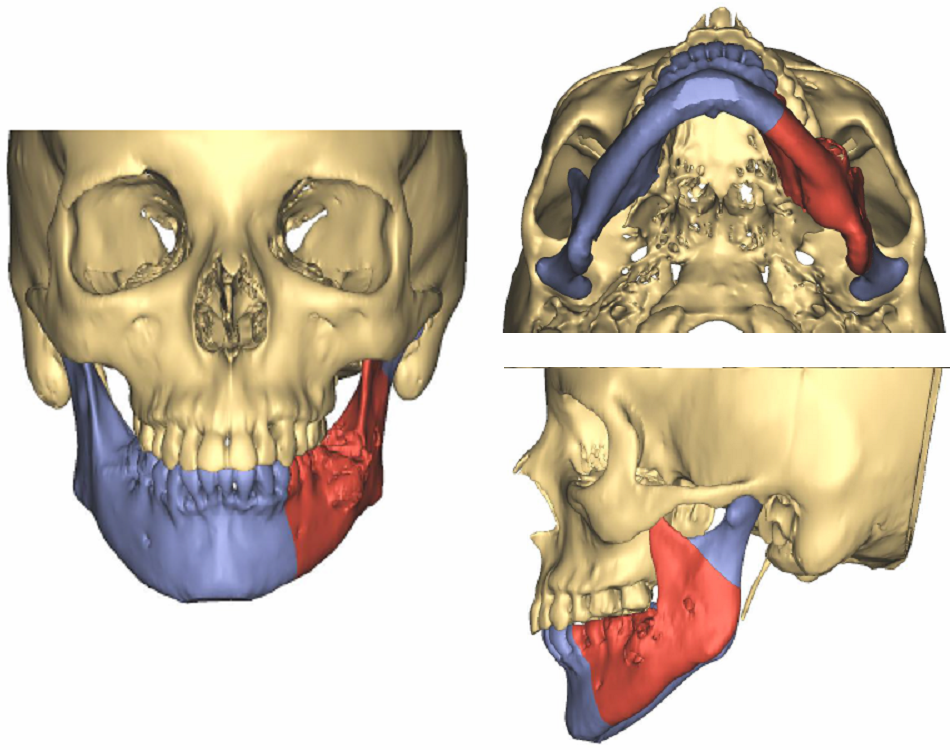
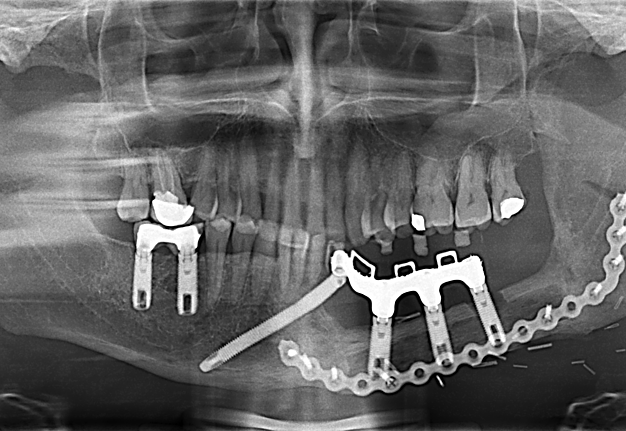
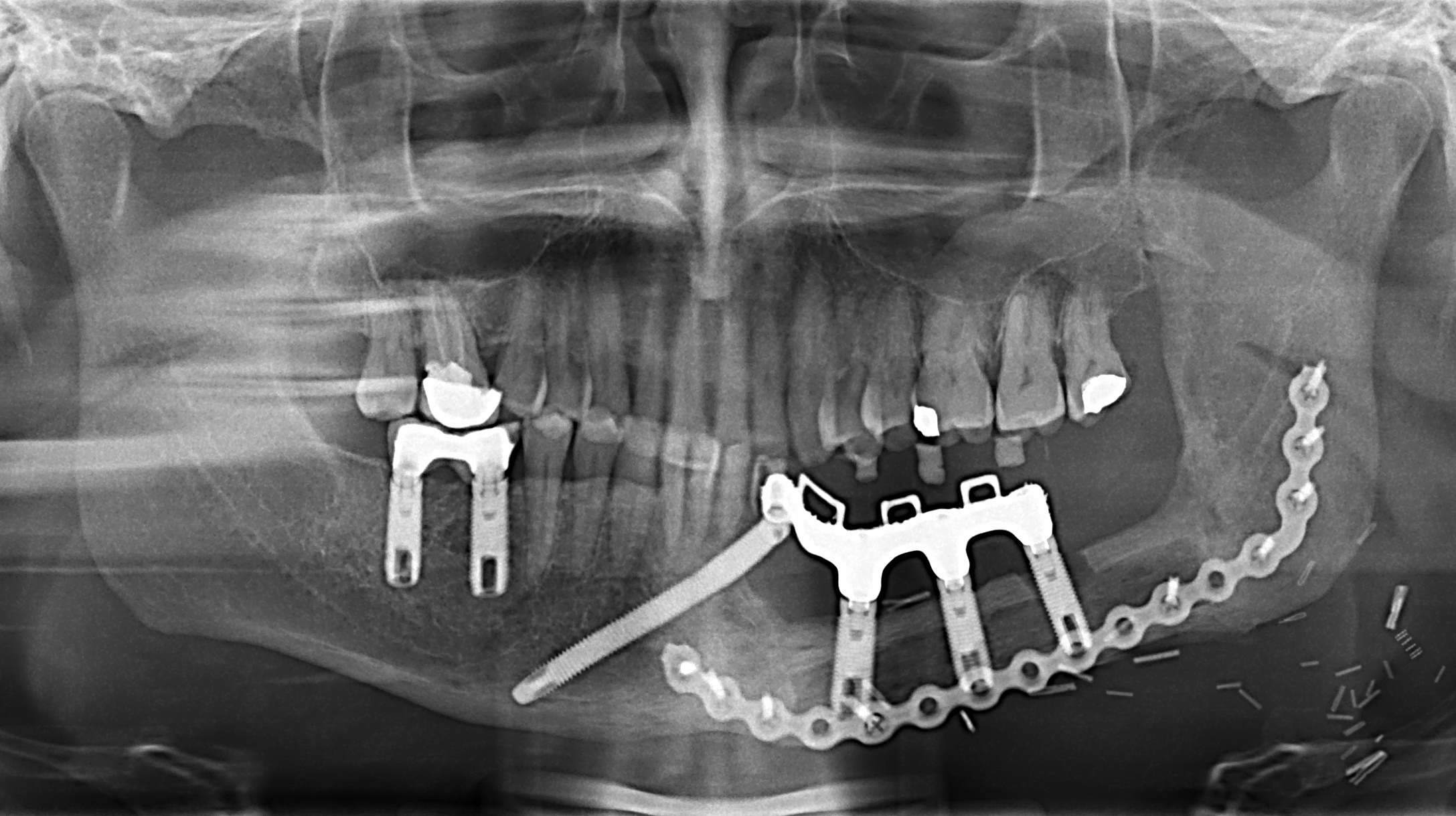
Retrospective review of patient charts treated from 2005-2015 was completed. Total of 116 patients with mandibular fibula free flap reconstruction were identified. Nine of these patients who underwent dental implant placement were included in this study to demonstrate the versatility of this reconstructive technique. Exclusion criteria were lack of dental implant placement, lack of adequate follow up, or incomplete and lacking records. Although dental implant placement can be recommended to everyone, the cost of dental implants is often prohibitive for a majority of our patients. Unfortunately, many medical and dental insurance companies do not offer 100% coverage for dental implant rehabilitation, even in cases of malignant disease. The selected patient group included 4 females, 5 males, age ranged from 20 to 72 years old with a mean age of 42. Follow up ranged from 1 year 5 months to 6 years 9 months, and median was approximately 4 years. The diagnoses included squamous cell carcinoma, ameloblastoma, glandular odontogenic tumor, and self-inflicted gunshot wound. The resulting mandibular defects and reconstruction were classified based on Jewer and fibula osteotomy classifications (Fig 1, Fig 2). Detailed patient information, including timing of implant placement, is presented in Table 1.
TABLE 1. Patient Data (Swipe right to view entire table).
|
Patient Age, Gender |
Diagnosis | Jewer Classification | Fibula Class | Timing of Implant Placement (Months) After FFFe |
|---|---|---|---|---|
| 20M | GSWa | LCL | Class III | 41 |
| 33M | Ameloblastoma | L | Class I | 33 |
| 42F | Ameloblastoma | L | Class I | 3 |
| 45M | Ameloblastoma | CL | Class II | 9 |
| 49M | SCCA,b post-op XRTc | CL | Class II | Immediate at time of FFFe surgery |
| 52M | Glandular odontogenic tumor | LCL | Class II | 9 |
| 52M | SCCA, post op XRT | L | Class I | 7 |
| 55F | SCCA, no XRT | C | Class II | 8 |
| 72F | BRONJd | L | Class I | 12 |
a Gunshot wound
b Squamos cell carcinoma
c Radiotherapy
d Biphosphonate-related osteonecrosis of the jaws
e Fibula free flap
Results
In all nine patients reviewed, single barrel free fibula flaps were utilized. No intra-operative or immediate post-operative complications were noted and no flap failure occurred. Two out of nine patients developed intra-oral dehiscences that healed uneventfully and required no additional operating room interventions. In all nine patients, fibula flaps provided adequate bone stock for implant placement. All 30 implants were placed in bicortical fashion and none had issues with primary stability at the time of placement. No implants required removal to date. Additional surgical procedures, such as vestibuloplasty, keratinized mucosa grafting, and flap debulking were completed in four out of nine patients (Table 2). One patient with diagnosis of medication related osteonecrosis of the jaw did not complete dental rehabilitation due to issues with recurrent infection, need for fibula hardware removal and delayed healing complicated with extra-oral fistula. Three patients had implant supported overdentures fabricated and reported satisfaction with the results. Two patients underwent fixed partial denture fabrication and were also happy with the functional and esthetic results. The remaining four patients were awaiting final prosthesis delivery at the time of study.
TABLE 2. Patient Outcomes (Swipe right to view entire table).
| Patient Age, Gender, and Diagnosis |
Jewer Classification |
Number of Implants in Fibula |
Additional Implant Surgery |
Prosthesis | Complications |
| 20M, GSW | LCL | 2 | Flap debulking | Overdenture | None |
| 33M, amelobasltoma | L | 3 | None | Fixed partial denture | Periimplantitis requiring granulation tissue debridement, oral hygiene |
| 42F, ameloblastoma | L | 3 | None | In process of being fabricated2 |
None |
| 45M, ameloblastoma | CL | 4 | Vestibuloplasty | In process of being fabricated |
None |
| 49M, SCCA | CL | 3 | None | In process of being fabricated2 |
None |
| 52M, glandular odontogenic tumor |
LCL | 4 | Vestibuloplasty | Overdenture | None |
| 52M, SCCA | L | 3 | None | Fixed partial denture | Peri-implantitis, radiographic bone loss distal implant |
| 55F, SCCA | C | 4 | Vestibuloplasty, flap debulking, palatal mucosa graft |
Overdentures | Peri-implantitis requiring granulation tissue debridement, antibiotic treatment, oral hygiene |
| 72F, BRONJ | L | 4 | None | None | Hardware infection requiring removal, extraoral fistula |
The most common complication encountered in our group was peri-implant tissue inflammation and infection. Peri-implantitis resolved with granulation tissue removal and meticulous oral hygiene without causing peri-implant bone loss in two patients. One of the patients developed bone loss adjacent to the terminal implant that at the time of evaluation did not appear to compromise stability of the implant. Although eventual loss of implant with compromised bone support is certainly possible, conservative measures to address peri-implantitis were undertaken to prolong the life-span of the existing prosthesis.
Discussion
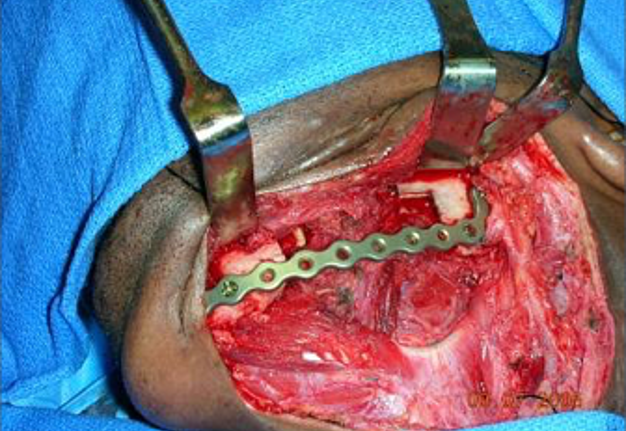
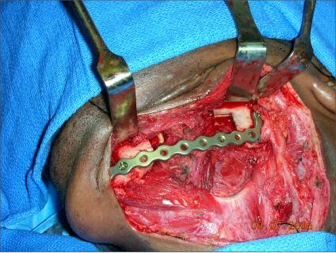
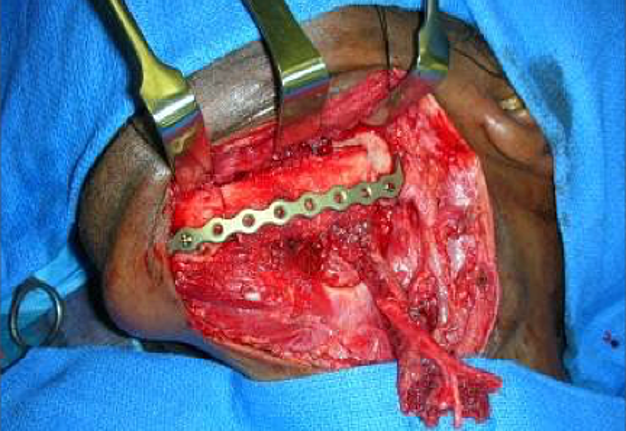
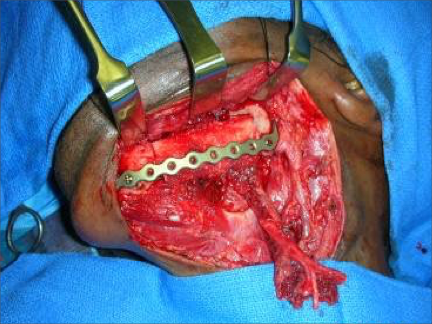
Free fibula flap for reconstruction of mandibular defects was first introduced by Hidalgo in 1989.6 Numerous studies since then have demonstrated the effectiveness and predictability of free fibula flaps for mandibular reconstruction (Fig 3, Fig 4, Fig 5, Fig 6).
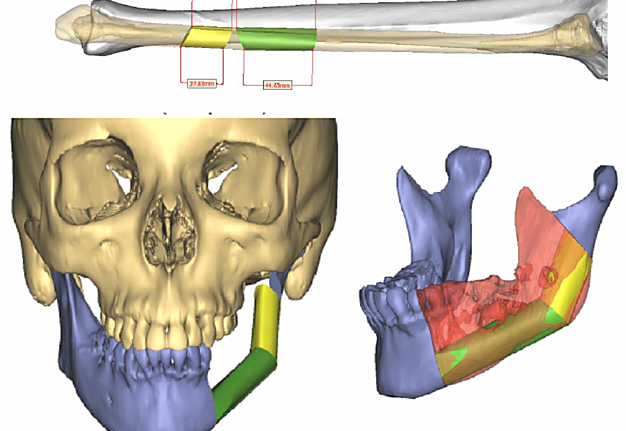
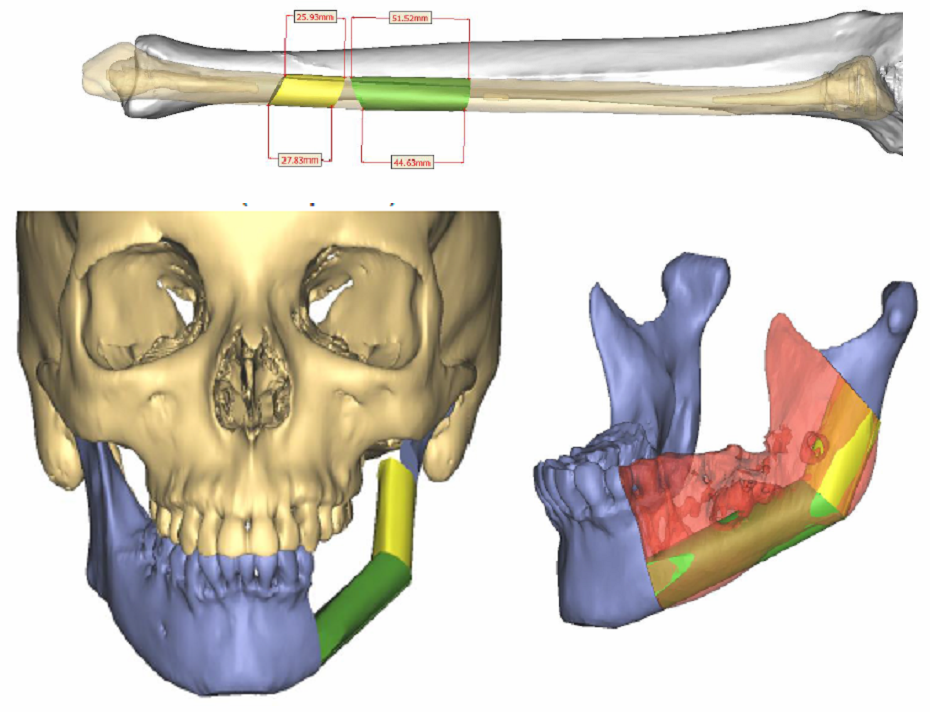
In order to facilitate comprehensive orofacial rehabilitation, a flap has to satisfy several requirements. First, it must provide sufficient bone length to ensure adequate repair of the continuity defect. Up to 26 cm of fibula can be harvested, which allows for reconstruction of mandibular defects spanning almost the entire length of mandible.7 The long segment of bone can be osteotomized in multiple locations, thus allowing for esthetic reconstruction of patient’s anatomy. Complex defects, requiring more than 2 osteotomies can be reconstructed with computer assisted virtual surgical planning (Fig 7A, B).7 Second, adequate bone and tissue stock has to be available for endosseous implant placement and provide satisfactory longterm implant survival rates. The dense cortical bone of the fibula, and its 1.0-3.0 cm thickness, provide ample primary implant stability by allowing bicortical engagement of conventional 12-14-mm implants.7 Skin paddle size can reach up to 32 x 14 cm thus allowing reconstruction of significant intraoral and extraoral soft tissue defects as well.8 Next, for a successful microvascular anastomosis, donor and recipient vessels must be of similar caliber. The flap is based on the peroneal artery, 1.5-2.5 mm diameter, and two venae comitantes, 2-4 mm in diameter which is similar to the diameter of commonly used recipient vessels in the head and neck.7, 8, 9 In addition, donor site morbidity is minimal with anticipated return to normal ambulation in 4 weeks after surgery.8
Several specific considerations must be taken into account when planning implant placement into fibula free flap. Optimal results can be achieved only when orofacial reconstruction is approached with the end result in mind. Thus input from the restorative dentist responsible for fabrication of the final prosthesis is essential in order to avoid unfavorable outcomes.
Optimal timing of implant placement has yet to be agreed upon to date. Eight out of nine patients included in this study underwent delayed implant placement with mean delay of 23 months, ranging from 3 to 41 months. In one case immediate implant placement was performed at the time of reconstruction. Prolonged interval to implant placement was primarily a result of socioeconomic or personal issues rather than medical complications. The timing of implant placement did not appear to have an effect on the overall outcome in our patients. Some authors recommend at least a 6-month period of healing prior to implant surgery,10 while others advocate immediate implant insertion into fibula at the time of reconstructive surgery.11 Delayed implant placement allows for sufficient bone remodeling and soft tissue healing thus allowing more precise implant placement (Fig 8A, B).12
In cases of malignant disease, a 6-12 month waiting period also allows monitoring for early disease recurrence, presence of which would discourage implant surgery due to poor overall prognosis. Disadvantages of this treatment option include need for additional surgery and prolonged period of time with suboptimal function due to delayed prosthetic rehabilitation. Immediate implant placement eliminates the need for additional surgery and its associated morbidity. However, it increases the risk of future implant disuse due to difficulty predicting final implant position once bone remodeling and soft tissue healing reach its final stages.13 Since cone beam CTs became widely used in dental practices, computer assisted surgical planning has also gained wide acceptance and has been shown to provide more predictable results with optimal final restorations.14 Nevertheless, desired implant placement may be impossible due to position of internal fixation screws necessary to secure the flap to native mandible. With delayed implant placement, simultaneous removal of fixation hardware is also possible, thus eliminating the risk of future hardware infection development. A total of 12 to 16 weeks are recommended for healing and osseointegration of implants prior to uncovering.8
Discrepancy in the bone height between native mandible and fibula was implicated in creation of unfavorable crown to fixture ratio that may increase the risk of implant failure.10 Several strategies were devised to circumvent this problem. Positioning of the fibula superior to the inferior border of the mandible improves the crown to implant ratio, but may result in evident facial deformity.9 Placement of the reconstruction plate along the inferior border is often used to correct this issue.9 Double-barrel fibula and vertical distraction osteogenesis are more technically challenging and demanding options available for fibula height correction.8 From a restorative stand point, a milled bar framework may be used to help correct the height discrepancy, as well as facilitate distribution of masticatory forces (Fig 9).8
All of our patients were reconstructed with fibulas that were aligned with inferior border of the mandible and 8 out of 9 were satisfactorily restored with dental prosthesis, or are in the process of being restored, without the above-mentioned corrections. One patient with a history of medication related osteonecrosis of the jaw (MRONJ) did not have a prosthesis fabricated to date due to delay in healing that was complicated by hardware infection.
One of the disadvantages from the standpoint of dental rehabilitation is the excessive mobility and thickness of the fibula skin paddle. Reconstruction of intraoral soft tissue defects often results in vestibular obliteration and requires vestibuloplasty with tissue debulking to facilitate prosthesis fabrication and use.8 Lack of attached mucosa adjacent to the implant abutments increases risk of irritation and inflammation of the hypermobile fibula skin paddle.10
One of our patients required vestibuloplasty, flap debulking, and keratinized tissue graft. Two others required vestibuloplasty and one more patient required flap debulking. In total 4 out of 9 patients (i.e., 44%) required additional procedures, which is consistent with reports in the literature.6
Conclusions
Implants placed in fibulas have high success rates comparable to native mandible, >95%.15 Immediate or late implant failure is uncommon, and in our cohort, no implants were lost. Two out of nine patients developed peri-implantitis that had eventually resolved, although required invasive intervention. Peri-implant tissue inflammation is one of the most common complications reported in the literature.16 Chronic peri-implantitis may result in peri-implant bone loss as was observed in one of our patients.
As illustrated by our selection of cases, fibula free flap reconstruction is the treatment of choice for patients with various disease processes resulting in significant mandibular defects and can ultimately be restored with fixed dental prostheses (Fig 10).
Since comprehensive orofacial rehabilitation is a multistep complex process involving different healthcare specialists and multiple surgeries, patients’ prognoses, interest and enthusiasm needs to be assessed. Multiple studies have shown that patient’s quality of life is dramatically improved when these surgical techniques are used to restore patient’s form and function.17
References (17)
- Markiewicz MR, Bell RB, Bui TG, Dierks EJ, Ruiz R, Gelesko S, Pirgousis P, Fernandes R. Survival of microvascular free flaps in mandibular reconstruction: a systematic review and meta-analysis. Microsurgery 2015;35:576–87. Crossref | Medline | Google Scholar
- Boyd JB, Rosen I, Rotstein L, Freeman J, Gullane P, Manktelow R, Zuker R. The iliac crest and the radial forearm flap in vascularized oromandibular reconstruction. Am J Surg 1990;159:301–8. Crossref | Medline | Google Scholar
- Rogers SN, McNally D, Mahmoud M, Chan MF, Humphris GM. Psychologic response of the edentulous patient after primary surgery for oral cancer: a cross-sectional study. J Prostate Dent 1999;82:c317. Crossref | Medline | Google Scholar
- Ooi A, Feng J, Tan HK, Ong YS. Primary treatment of mandibular ameloblastoma with segmental resection and free fibula reconstruction: achieving satisfactory outcomes with low implant-prosthetic rehabilitation uptake. J Plast Reconstr Aesthet Surg 2014;67:498–505. Crossref | Medline | Google Scholar
- Iizuka T, Häfliger J, Seto I, Rahal A, Mericske-Stern R, Smolka K. Oral rehabilitation after mandibular reconstruction using an osteocutaneous fibula free flap with endosseous implants. Factors affecting the functional outcome in patients with oral cancer. Clin Oral Implants Res 2005;16:69–79. Crossref | Medline | Google Scholar
- Hidalgo DA. Fibula free flap: a new method of mandible reconstruction. Plast Reconstr Surg 1989;84:71–9. Medline | Google Scholar
- Wei F-C, Mardini S. Flaps and reconstructive surgery. 1st ed. Philadelphia: Saunders Elsevier; 2009.
- Kademani D, Tiwana P. Atlas of oral and maxillofacial surgery. 1st ed. Philadelphia: Saunders Elsevier; 2015.
- Su T, Fernandes R. Microvascular reconstruction of the mandible: an argument for the fibula osteocutaneous free flap. Rev Esp Cirug Oral Maxilofac 2014;36:1–8. Crossref
- Anne-Gaëlle B, Samuel S, Julie B, Renaud L, Pierre B. Dental implant placement after mandibular reconstruction by microvascular free fibula flap: сurrent knowledge and remaining questions. Oral Oncol 2011;47:1099–104. Crossref | Medline | Google Scholar
- Sclaroff A, Haugey B, Gay W, Paniello R. Immediate mandibular reconstruction and placement of dental implants at the time of ablative surgery. Oral Surg Oral Med Oral Pathol 1994;78:711–7. Crossref | Medline | Google Scholar
- Chiapasco M, Abati S, Ramundo G, Rossi A, Romeo E, Vogel G. Behaviour of implants in bone grafts or free flaps after tumor resection. Clin Oral Implants Res 2000;11:66–75. Crossref | Medline | Google Scholar
- Disa J, Hidalgo D, Cordeiro P, Winter R, Thaler H. Evaluation of bone height in osseous free flap mandible reconstruction: an indirect measure of bone mass. Plast Reconstr Surg 1999;103:1371–7. Crossref | Medline | Google Scholar
- Okay DJ, Buchbinder D, Urken M, Jacobson A, Lazarus C, Persky M. Computer-assisted implant rehabilitation of maxillomandibular defects reconstructed with vascularized bone free flaps. JAMA Otolaryngol Head Neck Surg 2013;139:371–81. Crossref | Medline | Google Scholar
- Kramer FJ, Dempf R, Bremer B. Efficacy of dental implants placed into fibula-free flaps for orofacial reconstruction. Clinical Oral Implants Research 2005;16:80–8. Crossref | Medline | Google Scholar
- Blake F, Bubenheim M, Heiland M, Pohlenz P, Schmelzle R, Gbara A. Retrospective assessment of the peri-implant mucosa of implants inserted in reanastomosed or free bone grafts from the fibula or iliac crest. Int J Oral Maxillofac Implants 2008;23:1102–8. Medline | Google Scholar
- Vu DD, Schmidt BL. Quality of life evaluation for patients receiving vascularised versus nonvascularized bone graft reconstruction of segmental mandibular defects. J Oral Maxillofac Surg 2008;66:1856–63. Crossref | Medline | Google Scholar